Understanding Red Flags in EM-IM Residency Applications
Emergency Medicine-Internal Medicine (EM IM combined) residencies attract driven applicants who thrive on complexity and acuity. Because these programs are small, competitive, and intensive, program directors scrutinize applications closely for signs of risk—often referred to as “red flags.”
Red flags are not automatic rejections, but they do demand an explanation. The stronger and more coherent your narrative, the more likely programs will see you as a resilient, self-aware future colleague rather than a risky match.
Common red flags in emergency medicine internal medicine applications include:
- Low or failing USMLE/COMLEX scores
- Course failures or repeated clerkships
- Gaps in training or employment
- Disciplinary actions or professionalism concerns
- Multiple attempts at the Match
- Visa or international medical graduate (IMG) complexities
- Significant specialty switches, especially late ones
This guide focuses on how to explain gaps, addressing failures, and reframing these challenges within the specific context of EM-IM combined programs.
How EM-IM Programs View Red Flags
EM-IM programs are uniquely demanding. Residents must meet dual board requirements, cover multiple clinical settings, and switch mindsets quickly—from rapid ED triage to nuanced inpatient management. Because of this, program leadership worries about:
- Reliability and professionalism
- Stamina and resilience
- Testing and board exam performance
- Ability to work in high-pressure, high-stakes settings
When program directors see red flags, they ask:
- Is this a pattern or a one-time issue?
- Has the applicant demonstrated insight and growth?
- Will this impact their ability to complete a dual residency and pass both boards?
- Does their explanation align with letters, MSPE, and other parts of the file?
Your job is to provide a clear, consistent, and honest narrative that reassures programs on those points.
The Three Core Principles of Addressing Red Flags
No matter the specific issue, your explanation should reliably do three things:
Take ownership without self-sabotage
- Avoid blaming faculty, “unfair exams,” or vague “personal issues” if you can be more specific.
- Accept responsibility where appropriate: “I underestimated…,” “I did not seek help early enough…,” “I needed to improve my study strategies…”
Provide context without making excuses
- Briefly outline what was happening (illness, family crisis, mental health, adjustment to a new system, etc.).
- Emphasize what you learned and how you changed behavior going forward.
Show evidence of improvement
- Improved scores on later exams
- Strong clinical evaluations or senior rotations
- Additional coursework, research, or advanced clinical roles
- Leadership or quality improvement projects demonstrating responsibility and maturity
Program directors are more reassured by objective evidence of improvement than by polished wording alone.

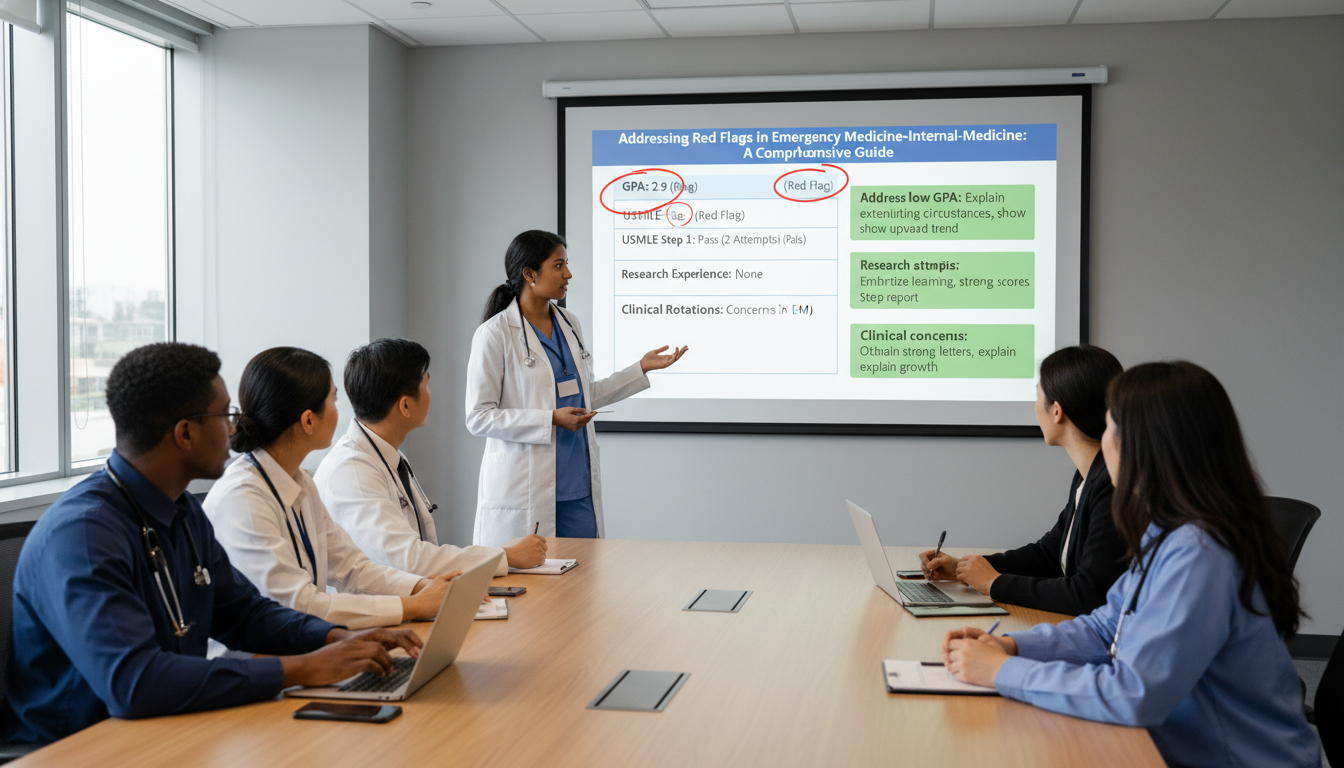
Common Red Flags in EM-IM Applications and How to Address Them
1. Exam Failures and Low Scores
In a dual residency where residents must pass two sets of boards (EM and IM), exam performance matters. A failed USMLE Step/COMLEX Level or low scores can trigger strong concern.
What Program Directors Worry About
- Risk of failing in-training exams and boards
- Needing remediation time during residency
- Added stress in an already intense combined curriculum
How to Explain Exam Failures
Use a structure like this:
State the issue plainly
- “I failed USMLE Step 1 on my first attempt.”
- “I underperformed on COMLEX Level 2, scoring below the national average.”
Provide concise context
- Was it poor study strategy? Personal/family crisis? Health issue? Test anxiety?
- Focus on what you could control and how you misjudged or mishandled it.
Describe concrete changes you made
- New study techniques (e.g., question banks, spaced repetition, dedicated schedule)
- Seeking help (tutors, learning specialists, mental health support)
- Adjusting lifestyle (sleep, exercise, time management)
Present evidence of improvement
- Strong performance on Step 2/Level 2 or shelf exams
- Improvement on subsequent in-training exams (if applying as a reapplicant or prelim resident)
Example: Addressing a Step Failure
“I failed USMLE Step 1 on my first attempt due to ineffective study strategies and underestimating the exam’s breadth. I focused on passive reading instead of active question-based learning, and I did not seek help when I fell behind.
After failing, I met with our academic support office, transitioned to a structured schedule using question banks and spaced repetition, and completed weekly progress checks. I also limited extracurricular commitments and improved my sleep routine.
On my second attempt, I passed with a score above the national average and subsequently scored strongly on Step 2. My clerkship evaluations in IM and EM were consistently high, which I believe better reflect my clinical reasoning and application of knowledge.”
This approach:
- Accepts responsibility
- Explains context without drama
- Shows a clear arc of growth—critical for EM-IM combined programs that worry about long-term test performance.
2. Course Failures, Remediations, and Clerkship Repeats
Failing a course or clerkship—even more so if it’s in Internal Medicine or Emergency Medicine—will be examined carefully.
What Program Directors Worry About
- Clinical judgment and patient safety
- Professionalism or reliability issues (missed shifts, incomplete notes)
- Difficulty adapting to complex clinical environments
How to Explain Clinical or Course Failures
Clarify exactly what you failed
- “I failed my Internal Medicine clerkship due to performance on the NBME shelf exam,” or
- “I remediated my Surgery clerkship after concerns about organization and note completion.”
Differentiate knowledge vs. professionalism issues
- Knowledge → focus on study skills and subsequent improvement.
- Professionalism/behavior → focus on insight, feedback acceptance, and systematic behavior change.
Highlight clear, documented improvement
- Honors or high passes in later clinical rotations
- Strong sub-internship in EM or IM
- Letters that explicitly speak to your reliability, teamwork, and growth
Example: Remediated Internal Medicine Clerkship
“During my core Internal Medicine rotation, I struggled to balance clinical responsibilities with shelf exam preparation and ultimately failed the NBME exam, resulting in a remediation requirement. My clinical evaluations noted that I worked hard and communicated well with patients, but my knowledge base and test performance lagged.
I remediated the rotation with a structured daily study plan and more active use of question banks. I also met weekly with a faculty advisor to review challenging cases. On remediation, I passed the rotation comfortably and received improved clinical evaluations.
In my subsequent IM sub-internship and EM rotation, I received strong evaluations for clinical reasoning, reliability, and teamwork. My performance on Step 2/Level 2 also reflected this growth. These experiences have made me much more proactive in seeking feedback and using it to guide my learning.”
For EM-IM programs, note specifically how you used feedback in both acute care and longitudinal care settings—this dual adaptability is vital.
3. Gaps in Education or Employment
Program directors are always looking for unexplained time periods. Gaps may occur:
- Between medical school and application
- After failing to match previously
- During medical school (leave of absence, extended curriculum)
Why Gaps Raise Concerns
- Questions about health, motivation, or professionalism
- Suspicion of unreported failures or disciplinary issues
- Worries about clinical skill decay
How to explain gaps is a key question many applicants struggle with. The goal is to be:
- Honest but appropriately bounded regarding personal details
- Specific enough to avoid appearing evasive
- Focused on how you maintained or rebuilt readiness for EM-IM
Framework to Explain Gaps
Name the gap and duration clearly
- “I took a one-year leave of absence from August 2021 to July 2022.”
Give brief, honest rationale
- Health condition, family responsibility, personal/mental health, visa delays, research, etc.
- You do not need to disclose every clinical detail; instead, describe the impact and recovery.
Emphasize constructive activities during that time
- Research in EM or IM
- Clinical observerships or hands-on experience where permissible
- Coursework (public health, statistics, quality improvement)
- Volunteer work, especially in acute or underserved care
Reassure programs about current readiness
- “My condition is now stable and does not interfere with my ability to meet residency demands.”
- “I have been back in full-time clinical training for X months with strong evaluations.”
Example: One-Year Leave of Absence
“I took a one-year leave of absence between my third and fourth years of medical school to manage a significant family obligation. I was the primary support for a close family member dealing with a serious illness. This required my presence and made it impossible to fully engage in clinical training.
During this period, I remained connected to medicine by completing a remote research project in emergency department flow and reading core internal medicine texts. Once the situation stabilized, I returned to school full time. Since returning, I have completed all remaining clerkships on schedule and received strong evaluations, particularly in EM and IM.
This experience deepened my empathy for patients and families facing crises and reinforced my commitment to EM-IM, where I can combine acute problem-solving with ongoing relationship-based care.”
For EM-IM, explicitly tying your gap experience to resilience and empathy in crisis contexts can be a real strength.
4. Professionalism Concerns or Disciplinary Actions
These are among the most serious red flags: documented academic dishonesty, unprofessional conduct, recurrent lateness, communication problems, or boundary violations.
What Program Directors Worry About
- Risk to patient safety and team function
- Liability for the institution
- Difficulty remediating entrenched behavior patterns
How to Address Professionalism Red Flags
These require direct, humble, and fully honest explanations. Attempted minimization is usually more damaging than the event itself.
State what happened and own your role
- “I was placed on professionalism remediation after repeated tardiness to clinical duties,” or
- “I received a disciplinary note for inappropriate use of social media.”
Explain what you learned
- What feedback did you receive?
- How did you come to see the seriousness of the issue?
Describe the behavior changes you implemented
- Systems (alarms, commute planning, reduced outside commitments)
- Mentorship or counseling
- Participation in professionalism or communication workshops
Provide evidence it is not a pattern
- No further incidents over X years
- Explicit mention in letters that the issue was resolved and that you are now reliable and professional
Example: Professionalism Remediation
“In my second year of medical school, I was placed on professionalism remediation for frequent tardiness to required sessions. At the time, I was balancing off-campus responsibilities and underestimated the impact of my late arrivals on my classmates and faculty.
Through remediation meetings, I came to understand that reliability is a core professional obligation, especially critical in acute settings like the emergency department and inpatient wards. I worked with the dean’s office to restructure my schedule, built in earlier departure times for commuting, and limited some extracurricular activities.
Since then, I have had no further professionalism concerns. My clinical evaluations repeatedly describe me as dependable and prepared. My EM and IM faculty have trusted me with increased responsibility on shift and on the wards, and this growth is reflected in my letters of recommendation.”
In EM-IM, where teamwork under time pressure is constant, programs must believe this issue is fully resolved.

Crafting Your Application Narrative: Where and How to Address Red Flags
1. Personal Statement
Your personal statement is a strategic place to proactively, but briefly, address major red flags—especially those that influence your motivation for EM-IM combined training.
When to include it:
- Significant exam failures that might raise concern about persistence
- Longer leaves of absence
- Serious professionalism or disciplinary issues (if not fully explained elsewhere)
How to write it:
- Devote one concise paragraph to the issue.
- Avoid making it the centerpiece; your passion for EM-IM should remain central.
- Focus on what you learned and how it improved your readiness.
Example sentence structures:
- “Early in medical school, I struggled with… This led to… Since then I have…”
- “A personal challenge during [time frame] resulted in… Returning to training, I approached my work differently by…”
2. ERAS “Education” and “Experience” Sections
Use these fields to:
- Clearly indicate leaves of absence, repeated years, or extended programs
- Briefly explain gaps or non-traditional timelines in the comments section
- Highlight continuity experiences (e.g., ongoing EM scribing, IM research, clinical observerships)
This supports a transparent, consistent story that aligns with your MSPE and transcripts.
3. Dean’s Letter / MSPE
The Medical Student Performance Evaluation often mentions red flags explicitly. You cannot control its content, but you can:
- Request to meet your dean or advisor to discuss context you’d like emphasized
- Make sure your self-explanations in ERAS and interviews match the MSPE tone and facts
4. Letters of Recommendation
Letters can be your most powerful tool to offset red flags, especially in EM-IM combined programs.
Seek letters from:
- EM and IM faculty who supervised you closely and can speak to resilience and reliability
- Mentors who know the story behind your red flags and can attest to your growth
- If available, a program director or clerkship director explicitly addressing prior concerns
You may politely ask a trusted letter writer:
“Would you feel comfortable commenting on my growth since [exam failure/professionalism issue], especially in terms of reliability and readiness for a combined EM-IM training program?”
Preparing to Discuss Red Flags in EM-IM Interviews
Many red-flag issues come up during interviews. Being ready—and steady—is critical.
Anticipate Common Questions
For EM-IM combined applicants, expect variations of:
- “Tell me about your Step failure / low score.”
- “I noticed you took some time off—how did that shape you?”
- “Can you walk me through what happened with your [clerkship/course/professionalism concern]?”
- “Given the intensity of EM-IM training, how have you shown you can handle sustained stress and dual demands?”
Use a Three-Part Interview Response Structure
- What happened (briefly and objectively)
- What you learned and what you changed
- How you’ve done since, with specific examples
Example: Interview Answer About a Gap
“In my third year, I took a six-month leave to address a mental health challenge that had been affecting my academic performance. During that time, I worked closely with a therapist, developed more effective coping strategies, and restructured my daily habits around sleep, exercise, and time management.
When I returned, I completed my remaining rotations without delay and received strong evaluations, particularly in EM and IM. I now have a sustainable system for managing stress and have been stable for over two years. I believe this experience has made me more attuned to the mental health struggles our patients face and better able to handle the demands of a program as rigorous as EM-IM combined.”
You don’t have to share diagnostic labels unless you choose to. Focus on impact, treatment, stability, and current readiness.
Practice Aloud
- Rehearse your answers until they are fluent but not robotic.
- Aim for a calm, matter-of-fact tone—no defensive edge, no over-apology.
- Consider doing mock interviews with a mentor, advisor, or EM-IM resident.
Turning Red Flags into Evidence of Readiness for EM-IM
EM-IM combined programs value:
- Resilience under pressure
- Adaptability between very different clinical settings
- Insightful, reflective practitioners
- Strong teamwork and communication
Handled well, your red flags can demonstrate:
- Resilience: You encountered difficulty, adapted, and came back stronger.
- Self-awareness: You recognized your limitations and sought help.
- Commitment to EM-IM: Despite setbacks, you deliberately chose a demanding path.
- Patient-centered empathy: Your struggles make you more attuned to patient and colleague challenges.
Concrete Steps to Strengthen Your Application After Red Flags
Excel in EM and IM rotations and sub-internships
- Ask for direct feedback; show that you implement it.
- Volunteer for responsibility within appropriate limits.
Engage in EM or IM research or QI projects
- Focus on systems issues relevant to both specialties (sepsis, ED throughput, transitions of care).
- This shows long-term commitment and ability to see the big picture.
Maintain or regain clinical currency
- Scribe work, hospitalist assistant roles, clinical observerships (especially for IMGs or reapplicants).
Build a mentorship “team”
- At least one EM mentor, one IM mentor, and ideally someone familiar with EM-IM combined training.
- Discuss openly how to present your story and where to apply strategically.
Be realistic with your program list
- Include a range of EM-IM, categorical EM, and categorical IM programs depending on your profile.
- Consider programs known to be holistic and IMG-friendly if relevant.
Frequently Asked Questions (FAQ)
1. Should I always mention my red flags in my personal statement?
Not always. Include red flags in your personal statement when:
- They are substantial (exam failures, leaves of absence, major professionalism issues), and
- You can connect them meaningfully to your growth and motivation for EM-IM.
For minor issues (e.g., slightly low scores without failures; small, short gaps already well explained in ERAS), a brief explanation in the appropriate ERAS field may be sufficient. If you’re unsure, ask an advisor or mentor familiar with EM-IM combined programs.
2. How detailed do I need to be about health or mental health issues?
Programs need to understand:
- The general nature of the impact (e.g., required time off, temporary performance issues).
- That the issue has been adequately addressed.
- That you are currently able to meet the demands of residency.
You do not need to share specific diagnoses or intimate personal details. Focus on what you did to recover, how you manage your health now, and a track record of stable performance since.
3. I failed to match previously. How do I explain this without sounding defensive?
Be straightforward:
- Describe briefly why you think you didn’t match (timing, exam performance, limited applications, late specialty switch).
- Emphasize what you did in the interim year: research, clinical work, additional courses, improved scores.
- Articulate why EM-IM combined (or EM/IM) remains the right fit and how you’re more prepared this cycle.
Programs frequently take successful residents who are reapplicants—especially when they show clear, documented growth.
4. Is it realistic to match into EM-IM combined if I have a major red flag?
It depends on the type and severity of the red flag, but it’s not impossible:
- Single exam failures with subsequent strong performance are often recoverable.
- A well-managed and well-documented gap with clear growth can be reframed positively.
- Serious professionalism violations are harder but not always disqualifying if distant, clearly remediated, and strongly counterbalanced by impeccable recent performance and supportive letters.
You may need to:
- Apply broadly to both EM-IM and categorical EM/IM programs.
- Prioritize programs known for holistic review.
- Invest heavily in strong clerkship performance and letters.
Handled thoughtfully, addressing failures and explaining gaps can demonstrate the very qualities—resilience, self-reflection, and commitment—that EM-IM programs value most.






















