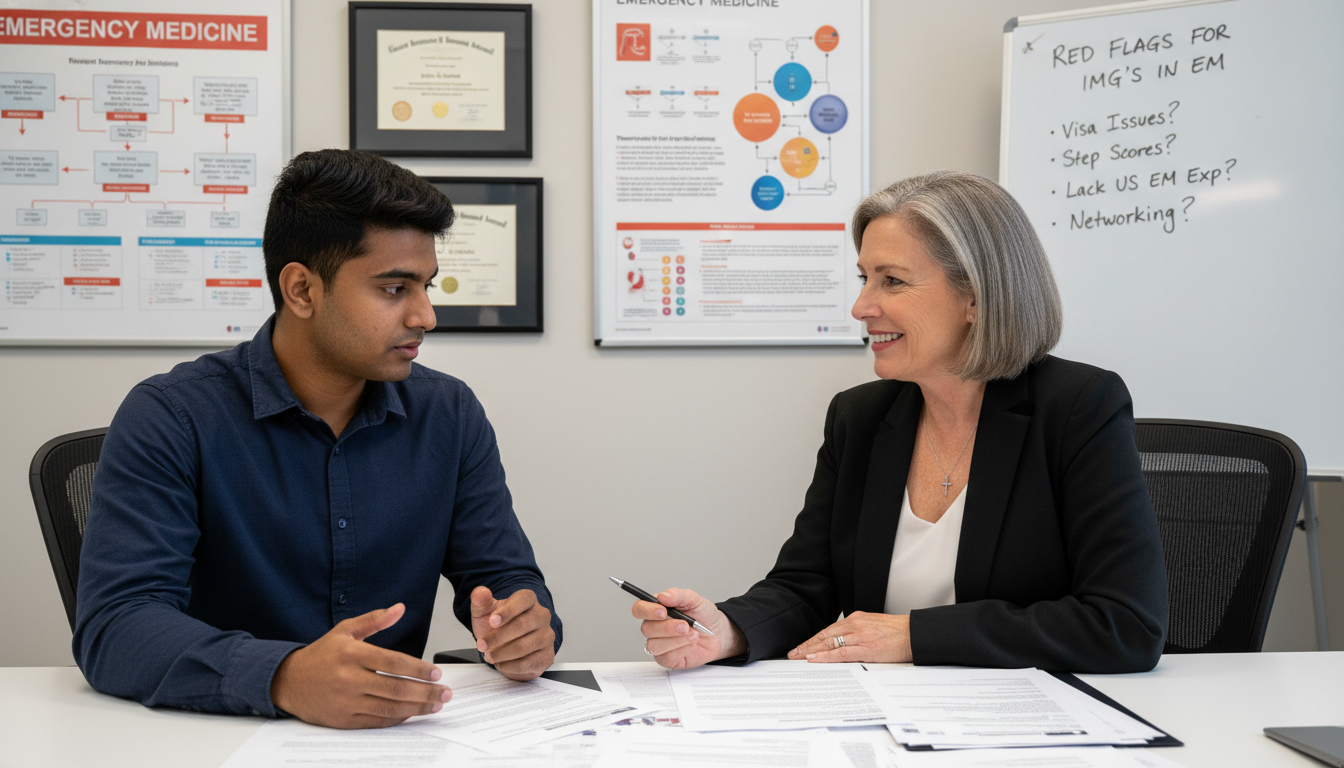
For a non-US citizen IMG, emergency medicine (EM) can feel like one of the toughest specialties to break into—especially if your application includes potential “red flags.” Yet every year, foreign national medical graduates with imperfect records successfully match into EM. The difference is rarely perfection; it’s understanding how to identify, strategically address, and convincingly explain your weaknesses.
This guide is written specifically for the non-US citizen IMG targeting emergency medicine residency in the US. It will walk you through:
- Common red flags in EM applications
- What they actually mean to program directors
- How to explain gaps and failures without making things worse
- Strategies to mitigate risk and strengthen your overall EM match profile
Understanding Red Flags in Emergency Medicine Residency Applications
In residency selection, a “red flag” is any element that makes a program pause, question reliability, or worry about future performance. In a competitive, high-acuity field like EM, red flags are taken seriously—but they are not always automatic rejections.
Why EM Program Directors Are Cautious
Emergency medicine involves:
- High-volume patient care
- Shift work and circadian disruption
- Rapid decision-making with incomplete information
- Heavy reliance on teamwork and communication
Program directors (PDs) need residents who are reliable under pressure, emotionally stable, and capable of consistent performance. Any sign that you might struggle to complete training, handle stress, or work well on a team becomes a concern.
For a foreign national medical graduate, PDs may also wonder:
- Will visa issues cause delays or complications?
- Has the applicant had enough US clinical exposure to understand the system?
- Are communication skills strong enough for busy ED environments?
Because of this, context and narrative matter immensely. PDs don’t just look at your red flag—they ask:
“Does this applicant understand what went wrong, have they grown from it, and can they demonstrate reliability now?”
Common Red Flags for Non-US Citizen IMGs in EM—and What They Signal
Below are some of the most frequent red flags for non-US citizen IMGs aiming for emergency medicine residency, and how PDs interpret them.
1. Multiple USMLE Attempts or Low Scores
- Multiple attempts on Step 1, Step 2 CK, or OET/English assessments
- Very low Step 2 CK relative to EM applicant averages
- Long delay between graduation and taking/retaking exams
What PDs may think:
- “Will this applicant pass our in-training exams and ABEM boards?”
- “Can they handle intense cognitive load and time pressure?”
Key point: A single failure or low score is not automatically disqualifying—especially if there is a clear upward trend and a solid explanation.
2. Extended Gaps in Medical Training or Employment
Examples:
1–2 years after graduation with no clinical work
- Long “research” periods with shallow or unclear outputs
- Time away from medicine due to immigration, personal, or financial issues
Concerns:
- Knowledge and clinical skills may be outdated
- Motivation or commitment to EM may be inconsistent
- Applicant may be using EM as a backup or late decision
3. Failed Courses, Clerkships, or Rotations—Especially in Core or EM-Related Fields
- Remediation of internal medicine, surgery, pediatrics, psychiatry
- Failed sub-internships or EM electives
- Negative comments in MSPE/dean’s letter about professionalism or reliability
Red flags to PDs:
- Struggles in core rotations raise concern about day-to-day clinical performance
- Any mention of unprofessional behavior is taken extremely seriously in EM
4. Professionalism or Conduct Issues
- Academic probation, suspension, or disciplinary action
- Documentation of dishonesty, plagiarism, or exam misconduct
- Conflicts with supervisors, nurses, or team members
EM depends heavily on trust, teamwork, and rapid, clear communication. Any professionalism red flag is more serious than a test failure in the eyes of many PDs.
5. Multiple Program Transfers or Incomplete Residencies
- Starting a residency in another specialty and leaving early
- Failed or incomplete EM or non-EM residency training in another country
- Repeated moves without clear rationale
Programs will worry about:
- “Will this resident quit EM if things get difficult?”
- “Is there a pattern of interpersonal or professionalism issues?”
6. Very Late Graduation or Multiple Years Since Medical School
- ECFMG-certified for 5–10 years or more without US residency
- Primarily non-clinical work (e.g., business, non-medical job) during that period
PDs may see this as increased risk for:
- Skill decay
- Difficulty adapting to fast-paced ED care
- Possible mismatch between long-term career goals and EM training
How to Explain Gaps, Failures, and Other Red Flags Effectively
You cannot erase a red flag from your record, but you can reshape how it is perceived. The way you explain gaps, failures, and problems often matters more than the issue itself.
Principles for Addressing Any Red Flag
Be honest and consistent.
- Never falsify dates, change exam attempts, or hide disciplinary actions.
- Inconsistency between ERAS, personal statement, and interviews is worse than the original red flag.
Avoid over-explaining or emotional self-defense.
- Stick to facts and reflection: what happened, what you learned, how you changed.
- Don’t blame others, your school, or “bad luck” as the primary explanation.
Show insight and responsibility.
- PDs want to see: “I understand why this happened, and I’ve taken ownership of my growth.”
Demonstrate a clear corrective path.
- Concretely show what you did after the problem to improve your performance or circumstances.
End with current competence.
- Emphasize recent achievements that support your readiness for EM now, not who you were then.
How to Explain Gaps in Training or Time Away from Medicine
Extended gaps are common among non-US citizen IMGs due to visas, finance, family obligations, or working in other countries. The risk comes when gaps are poorly explained or unsupported by meaningful activity.
Strong vs Weak Explanations of Gaps
Weak explanation:
“I had difficulty with personal and family things and could not pursue medicine for several years.”
Stronger explanation:
“Between 2019–2021, my plans to pursue US training were delayed due to visa restrictions and family health responsibilities in my home country. During this time, I remained engaged in medicine by working as a general practitioner in an outpatient clinic, completing an online EM ultrasound course, and volunteering in local emergency services during the COVID-19 pandemic. These experiences reinforced my commitment to emergency medicine and sharpened my interest in acute care.”
What makes this stronger:
- Specific dates and reasons
- Medical involvement maintained
- Actions directly connected to EM interest
Where to Address Gaps
- ERAS Experience section (with clear dates and descriptions)
- Personal statement (briefly, not the entire essay)
- Interviews, with concise and prepared talking points
Avoid: Long, dramatic narratives. Two to four well-structured sentences usually suffice in writing; in interviews, aim for 1–2 minutes.
Addressing Failures: USMLE, Courses, and Rotations
A failed exam or failed rotation can be reframed as a turning point—if your later record shows true improvement.
USMLE Failures or Multiple Attempts
When addressing USMLE red flags, focus on:
- Specific obstacles you faced (language, test strategy, personal situation)
- Concrete steps you took to improve for the next attempt
- Demonstrable improvement in subsequent scores or performance
Example (for personal statement or interview):
“Initially, I underestimated the difference between factual recall and the clinical reasoning style required by the USMLE. My first Step 2 CK attempt did not reflect my true abilities, and I failed. I responded by restructuring my study approach: I completed a comprehensive QBank twice, used timed blocks to mimic test conditions, and joined a structured study group with weekly progress checks. On my second attempt, I improved my performance significantly and passed with a score that more accurately reflects my current clinical reasoning. This experience has made me more disciplined and strategic in how I approach high-stakes assessments.”
You don’t need to apologize repeatedly. State the facts, show insight, and move on.
Failed or Remediated Clerkships
For a failed rotation, especially in a core field, PDs want to know:
- Was this a one-time issue or part of a pattern?
- Was it knowledge-based, skills-based, or professionalism-related?
- What specific improvements have been documented since?
Example (knowledge and adaptation issue):
“During my third year, I failed my internal medicine clerkship due to difficulty with time management and documentation in a high-volume ward. I met with my clerkship director, received feedback, and repeated the rotation. I implemented a daily to-do list system, sought mid-rotation feedback, and practiced structured presentations. On my repeat rotation, my evaluations improved markedly, noting better organization and more concise communication. This experience has since helped me function more efficiently during my EM rotations in the US.”
If the failure involved professionalism, you must be especially clear:
- Acknowledge the behavior
- Explain what changed (mentorship, counseling, formal remediation)
- Provide supporting evidence of improved behavior (recent strong evaluations)

Professionalism Concerns, Communication Issues, and EM-Specific Red Flags
Emergency medicine programs are particularly sensitive to red flags involving behavior, reliability, and communication.
1. Professionalism and Conduct Issues
These include:
- Documented unprofessional behavior (rudeness, disrespect, absenteeism)
- Academic probation for non-academic reasons
- Dishonesty or integrity violations (plagiarism, falsified records)
If this is part of your record, you must not pretend it didn’t happen. Instead:
- Acknowledge it clearly and briefly.
- Explain the circumstances without blaming others.
- Emphasize what you learned and how you changed concretely.
- Provide current evidence of improvement:
- Recent strong evaluations
- Leadership roles
- Letters of recommendation speaking to your professionalism
Example (in an interview):
“In my final year, I was placed on academic probation due to repeated tardiness and missed deadlines. At the time, I was struggling to balance a long commute and family obligations, but I did not communicate this effectively to my supervisors. Through the remediation process, I learned the importance of proactive communication and time management. I developed a scheduling system, shared conflicts with my team early, and sought feedback regularly. Since then, I have completed multiple rotations—both at my home institution and in the US—without any similar issues, with evaluations noting improved reliability and teamwork.”
2. Communication and Accent Concerns
For a non-US citizen IMG, PDs may worry about:
- Clarity of spoken English in high-stress resuscitations
- Ability to communicate with patients and families from diverse backgrounds
- Understanding of US cultural and medicolegal norms
To address this:
- Aim for US-based clinical experiences (USCE), especially EM observerships or externships.
- Ask attendings to comment directly on your communication and teamwork in letters of recommendation.
- If applicable, mention OET or Step 2 CS-equivalent performance that supports your skills.
- Practice EM-style SBAR or concise case presentations before interviews.
In your application, highlight:
- Teaching roles in English
- Presentations at international or US conferences
- Patient education or community outreach activities
3. Previous Residency Attempts, Specialty Switches, or Withdrawals
If you started another specialty (e.g., internal medicine, surgery) and now want EM, PDs will ask:
“Why EM now, and how do we know you won’t leave again?”
How to frame it:
- Acknowledge the previous path clearly: country, specialty, duration.
- Explain what you liked but ultimately found lacking.
- Connect your decision to EM-specific aspects: acute care, variety, resuscitation, teamwork.
- Show that your transition is thoughtful and informed, not impulsive.
Example:
“I began a three-year internal medicine residency in my home country in 2018 and completed one year. During that time, I enjoyed the diagnostic reasoning and continuity of care, but I consistently felt most engaged during admissions and acute situations in the emergency department. After careful reflection and discussion with mentors, I realized that my strengths and interests align more with the fast-paced, team-based environment of emergency medicine. I completed EM electives in the US to confirm this fit, and the feedback I received from attendings on these rotations strongly supports my choice. I am now fully committed to pursuing emergency medicine as my long-term career.”
Strategic Ways to Mitigate Red Flags and Strengthen Your EM Profile
Addressing red flags is not only about explaining them; it’s also about proving you are now a strong candidate through your recent track record.
1. Maximize the Power of Recent Performance
PDs look most closely at your most recent 2–3 years. Use this to your advantage:
Strong US Clinical Experience (USCE) in EM or acute care
- EM electives, sub-internships, or hands-on externships
- ICU, urgent care, trauma, or acute internal medicine rotations
High-quality EM letters of recommendation (LoRs)
- At least 2–3 letters from US EM physicians if possible
- Letters that explicitly mention:
- Work ethic and reliability
- Clinical reasoning and resuscitation potential
- Communication and teamwork
- Any observed growth after a known red flag
Recent exam success
- Strong Step 2 CK and/or Step 3 (if taken) scores can mitigate earlier failures
- Consider taking Step 3 before applying if:
- You have prior exam failures
- You need to demonstrate readiness for independent decision-making
- You are a non-US citizen IMG seeking a visa (some programs prefer Step 3 completed)
2. Tailor Your Application Strategy to Risk Level
If you have multiple red flags (e.g., exam failure + gap + professionalism concern), you must:
Apply broadly and strategically
- Target a wide range of EM programs, including community-based and newer programs
- Consider combined EM/IM or EM/FM programs if available and of interest
- Investigate programs historically friendly to IMGs and visa sponsorship
Consider parallel planning
- Apply to a second specialty that is more IMG-friendly (e.g., Family Medicine, Internal Medicine)
- Be honest with yourself about risk tolerance, visa needs, and long-term goals
Parallel planning does not mean giving up on EM; it means protecting your chance to train in the US in case EM is not achievable in this cycle.
3. Use Your Personal Statement Wisely
For a foreign national medical graduate with red flags, your personal statement should:
- Clearly articulate why EM and why the US system
- Briefly acknowledge major red flags, framed as turning points
- Emphasize your recent achievements and current strengths
- Demonstrate maturity, reflection, and commitment to growth
Avoid:
- Turning the personal statement into a long apology
- Over-focusing on one negative event at the expense of your EM story
- Generic EM narratives that could apply to anyone
4. Prepare Intentionally for Interviews
During EM interviews, you should expect versions of:
- “Tell me about this gap in your CV.”
- “Can you explain your exam history?”
- “What did you learn from [specific failure]?”
- “Why should we be confident that you will complete our program successfully?”
Prepare structured, concise answers using a simple framework:
Event – Reflection – Action – Result
- Event: Briefly state what happened.
- Reflection: What did you realize about yourself or your approach?
- Action: What specific steps did you take to change?
- Result: How is your behavior/performance different now?
Practicing aloud with a mentor, advisor, or friend can reduce anxiety and help you avoid defensive or overly emotional responses.
Final Thoughts: Red Flags Are Risk Factors, Not Final Judgments
For a non-US citizen IMG applying to emergency medicine residency, red flags can feel overwhelming. However:
- Many successful EM residents and attendings once had similar issues—failed exams, changed specialties, or past professionalism concerns.
- What allowed them to succeed was honesty, reflection, sustained improvement, and strong mentorship.
Your goal is to convince program directors that:
- You understand your past issues clearly.
- You have taken meaningful, verifiable steps to address them.
- Your recent record demonstrates the reliability and resilience needed to thrive in the intense environment of emergency medicine.
If you approach your EM match process with strategic planning, humility, and persistence, your red flags do not have to define your future in emergency medicine.
FAQs: Addressing Red Flags as a Non-US Citizen IMG in Emergency Medicine
1. I am a non-US citizen IMG with a failed Step 2 CK. Should I still apply to emergency medicine?
Yes, you may still apply, but you must be strategic:
- Retake Step 2 CK promptly and aim for a clear improvement.
- Consider taking Step 3 to further demonstrate readiness.
- Obtain strong EM letters that highlight your current clinical skills and work ethic.
- Apply broadly and consider a parallel application in another specialty in case EM programs are highly selective regarding exam histories.
A single exam failure, if followed by strong performance, is often viewed as a yellow flag rather than a permanent barrier.
2. How should I document and explain a 3-year gap due to immigration and financial issues?
Be transparent and structured:
- In ERAS, list your activities during the gap: language courses, informal clinical exposure, research, non-medical employment, or family responsibilities.
- In your personal statement or interview, summarize in 3–5 sentences:
- The main reason for the gap (immigration process, finances, etc.)
- How you stayed connected to medicine if possible
- What you learned, and why you are now fully able to commit to residency
- Emphasize any recent clinical experiences and current stability in your situation.
The key is to show that the gap is resolved, and you are now ready for full-time training.
3. I previously started a residency in another specialty outside the US. Will this hurt my EM application?
It depends on how you explain it and what you have done since:
- Be honest about your prior training: duration, specialty, and reasons for leaving.
- Show that your shift to EM is based on clearly understood interests: acute care, resuscitation, ED pace, or team-based practice.
- Obtain at least one letter from a supervisor in that previous training who can attest to your professionalism and work ethic.
- Confirm your interest and fit by doing recent EM rotations, ideally in the US.
PDs mainly worry about instability or poor performance; if you frame your prior training as a step that clarified your true calling, it can be neutral or even positive.
4. My MSPE mentions concerns about professionalism in medical school. Can I still match into EM?
Professionalism concerns are serious, but not always insurmountable:
- You must acknowledge, not deny, the issue in interviews.
- Emphasize remediation steps you took: counseling, mentorship, feedback, leadership roles.
- Provide recent evidence, especially from US EM or acute care rotations, showing reliable attendance, good teamwork, and positive evaluations.
- Ask letter writers to comment directly on your professional behavior and growth.
Programs will be cautious, but many are willing to consider candidates who demonstrate clear, sustained change and strong current performance.
By understanding how to address red flags thoughtfully and proactively, you can significantly improve your chances of a successful EM match, even as a non-US citizen IMG and foreign national medical graduate.






















