
Understanding Red Flags as a US Citizen IMG in EM-IM
For a US citizen IMG, applying to Emergency Medicine–Internal Medicine (EM IM combined) programs can feel intimidating—especially if your application includes “red flags” such as exam failures, gaps, leaves of absence, professionalism concerns, or multiple attempts at matching. But having a red flag does not automatically exclude you from training in emergency medicine internal medicine. What matters most is how you understand, own, and explain those issues.
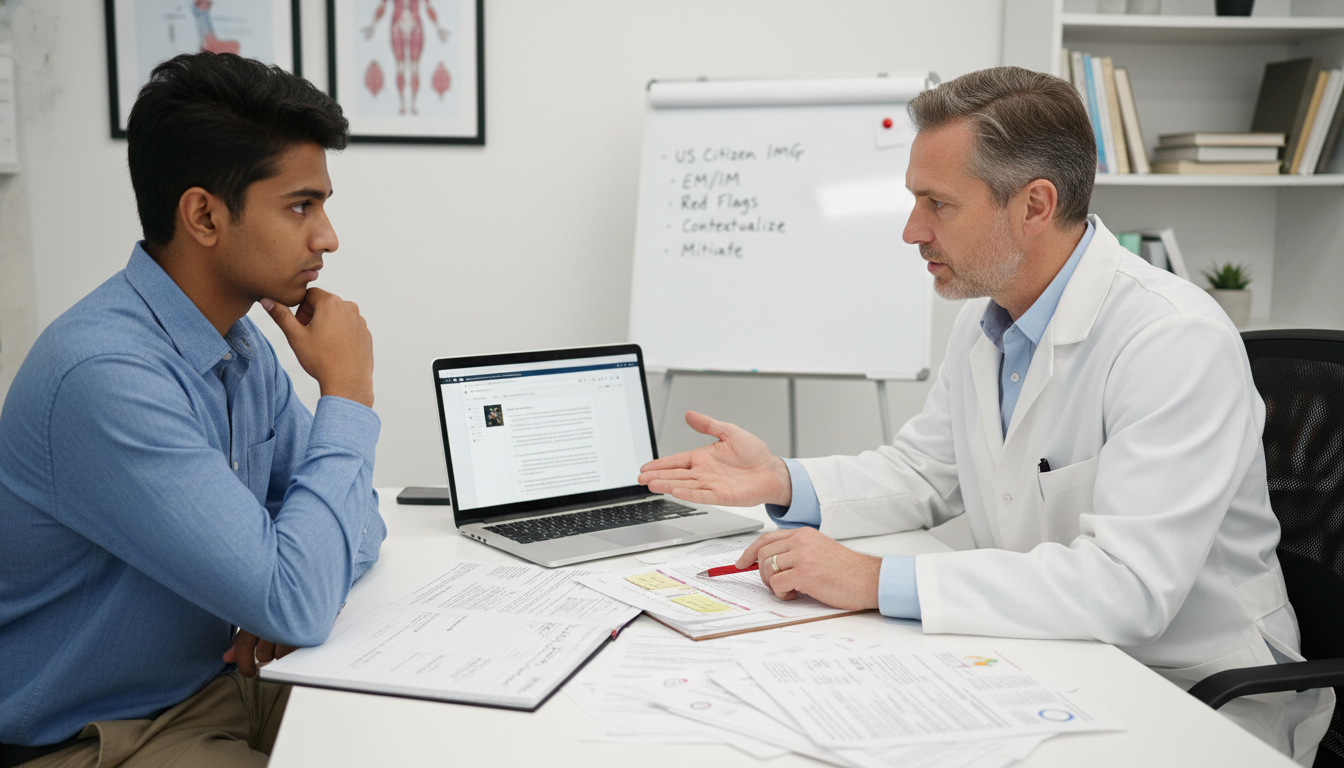
This article is designed specifically for the US citizen IMG / American studying abroad who is applying to EM-IM combined or closely related tracks (categorical EM or IM with strong cross-training interest). You’ll learn how program directors think about red flags in residency applications, how to explain gaps and failures, and how to convert liabilities into evidence of growth, maturity, and resilience.
How EM-IM Programs View Red Flags in US Citizen IMGs
EM-IM combined programs are small, competitive, and demanding. They expect residents to perform in high-stress, high-acuity settings while also excelling in complex inpatient medicine. Because of this, program leadership scrutinizes applications for reliability, professionalism, and long-term trajectory, not just test scores.
Why US Citizen IMGs Are Scrutinized Differently
As a US citizen IMG, you sit in a gray zone:
- You have US citizenship (no visa issues), which is an advantage.
- But you trained outside the US, which raises questions about:
- The rigor and structure of your school
- Clinical exposure to US-style systems
- Communication, documentation, and EMR use
- How you’ll adapt to US emergency departments and inpatient medicine services
Add a clear red flag, and program directors will ask:
- What exactly happened?
- What have you learned and changed since then?
- Is there objective evidence that you’re now ready for a rigorous EM-IM combined program?
Your strategy is to answer those questions clearly and proactively—in your application, personal statement, interviews, and letters.
Common Red Flags for US Citizen IMGs in EM-IM
Below are the issues EM-IM program directors frequently watch for, especially in American studying abroad applicants:
Board exam failures or multiple attempts
- USMLE Step 1/COMLEX Level 1 fail
- USMLE Step 2 CK / COMLEX Level 2 CE fail
- Multiple attempts needed to pass a given step
Gaps and leaves of absence
- Semesters or years off from medical school
- “Inconsistent” academic timeline or delayed graduation
- Time taken off after graduation prior to applying or reapplying
Academic performance concerns
- Repeated courses or clerkships
- Poor clinical evaluations, especially on EM or IM rotations
- No or weak EM rotations in the US
Professionalism or behavioral flags
- Documented professionalism concerns
- Conduct issues, academic dishonesty, or complaints
- Interpersonal difficulties on teams
Multiple application cycles / prior unmatched attempts
- Previous unsuccessful match in EM, IM, or another specialty
- Changing specialties late (e.g., from surgery to EM-IM)
Each of these is addressable, but not if you ignore it or hope it will go unnoticed. For EM-IM in particular, leadership wants residents who can handle constant evaluation, heavy workload, and acute responsibility. Showing that you’ve faced adversity, learned from it, and improved is very powerful.
Red Flag #1: Exam Failures and Low Scores – How to Explain and Recover
Board performance is often the most visible red flag. EM-IM programs typically want residents who can pass in-training exams and boards on the first try. But a past failure does not automatically disqualify you if you can show clear improvement and insight.
How Programs Interpret Exam Failures
Program directors commonly ask:
- Was it a single isolated exam failure, or a pattern?
- Did the applicant improve significantly on subsequent attempts?
- Is there a plausible and honest explanation (not excuses)?
- Has the applicant demonstrated new habits and support systems?
A US citizen IMG with USMLE Step 1 fail followed by strong Step 2 CK and solid clinical evaluations in EM/IM is very different from someone with repeated failures and no explanation.
How to Explain Exam Failures in Your Application
Use your personal statement and/or the ERAS “Impactful Experiences” / “Additional Information” section to address exam issues. Focus on:
Specific cause
- Poor study strategy (e.g., memorization instead of practice questions)
- Underestimation of time or over-commitment to work/family
- Health or personal crises (only share what you’re comfortable with)
- Mental health challenges now properly treated
Concrete corrective actions
- Structured study plans with question banks and spaced repetition
- Formal tutoring, academic coaching, or learning specialist support
- Regular self-assessments and timed practice exams
- Time management and schedule changes
Objective evidence of improvement
- Higher Step 2 CK scores relative to Step 1
- Passing on first attempt for subsequent steps
- Strong subject-specific performance in EM and IM rotations
- Good in-training or shelf exam scores (if reported in MSPE)
Sample Language for Addressing Failures (Adapt as Needed)
During my initial attempt at Step 1, I relied heavily on passive review and underestimated the importance of timed practice questions. This approach was not effective, and I did not pass on my first attempt. After this setback, I met with my school’s academic support team, restructured my study plan around daily question blocks, dedicated review of missed concepts, and weekly self-assessments. I also reduced extracurricular commitments. Using this new strategy, I passed Step 1 on my second attempt and improved my performance further on Step 2 CK. This experience taught me how to adapt my learning approach, seek help early, and maintain discipline under pressure—skills I now apply consistently in clinical practice.
This framing:
- Accepts responsibility
- Shows insight
- Demonstrates growth
- Connects improvement to readiness for EM-IM
Red-Flag Mitigation Strategies for Exam Issues
For emergency medicine internal medicine applicants with exam-related red flags:
- Take and excel on USMLE Step 2 CK if you haven’t already (even if your school doesn’t require it).
- Add US-based EM and IM rotations with strong performance and narrative evaluations to show you perform well clinically, despite earlier exam concerns.
- Ask letter writers to explicitly highlight your knowledge base and reliability on shift/ward.
- If possible, acquire evidence of improvement over time (e.g., shelf scores, mock exam scores, or performance trends noted in the MSPE).

Red Flag #2: Gaps, Leaves of Absence, and Non‑Traditional Timelines
Program directors are wary when they see unexplained gaps in training or long periods of inactivity. For a US citizen IMG, they may worry about visa issues (less applicable to you), academic difficulties, or unresolved personal problems.
You must show that:
- The gap had a specific and understandable reason.
- It is resolved or stable now.
- You used the time productively, or at least learned from it.
- You have a clear, continuous trajectory into EM-IM now.
How to Explain Gaps in Residency Applications
Whether it’s time off during medical school or after graduation, use clear, chronological explanations. Avoid vague terms like “personal reasons” without elaboration; they invite speculation.
Common legitimate reasons and how to frame them:
Health or family issues
- Briefly state: “I took a medical leave to address a health issue that is now resolved and does not affect my ability to meet residency demands.”
- Emphasize current stability and any accommodations you may or may not need.
Research or degree programs
- Describe specific projects, skills, and outcomes.
- Highlight how research taught you time management, critical thinking, and data interpretation—helpful for EM-IM.
Personal or financial hardship
- Explain the need (e.g., working to support family).
- Connect to your motivation for EM-IM and resilience under stress.
Reapplication cycles / unmatched year
- Be direct: “I did not match in my first cycle. I spent the following year in [research/clinical work/observerships] to strengthen my application and confirm my commitment to EM-IM.”
Sample Language for How to Explain Gaps
After graduating in 2022, I did not match into residency. During the following year, I completed a clinical research fellowship in sepsis management in the emergency department at [Institution]. I worked closely with EM and IM faculty, participated in data collection and manuscript preparation, and completed multiple US-based observerships. This experience deepened my understanding of acute care and reaffirmed that a combined emergency medicine internal medicine training pathway aligns with my long-term goal of practicing in high-acuity hospital settings.
Concrete Ways to Fill or Mitigate Gaps
If you are currently in a gap period or anticipating one, consider:
US clinical experience (USCE)
- EM and IM observerships or hands-on electives where allowed
- Ideally at institutions that can write strong letters for EM or IM
Research or quality improvement
- Projects in sepsis, resuscitation, ED crowding, inpatient medicine workflows
- Attempt to present at conferences or co-author a paper/poster
Employment in a clinical-adjacent role
- Scribe, clinical research coordinator, medical assistant, EMT, paramedic (if licensed)
- Emphasize how this maintained your clinical exposure and communication skills
Formal coursework
- MPH, MHA, or critical care/acute care–related certificates—if they align with EM-IM.
The key is to avoid an explanation like: “I was studying at home for a year” with no documentation or outcomes. Show that you remained engaged in medicine and personal development.
Red Flag #3: Professionalism Concerns and Difficult Feedback
Professionalism red flags are particularly serious because EM-IM combined residents are constantly interacting with multidisciplinary teams, consultants, nurses, and patients in high-pressure environments. Program directors will think: “If this behavior repeats in our ED or ICU, the consequences could be severe.”
Types of Professionalism Red Flags
- Negative comments in MSPE or dean’s letter about:
- Reliability, punctuality, or attendance
- Teamwork or conflicts with staff
- Documentation or compliance issues
- Behavioral incidents:
- Classroom or clinical professionalism violations
- Unprofessional communication or boundary problems
- Academic integrity issues:
- Cheating, plagiarism, falsifying documentation
Professionalism concerns are not always fatal, but they are a major concern. You must demonstrate that the underlying issue has been identified, addressed, and resolved.
How to Address Professionalism Red Flags
Accept responsibility clearly.
Avoid denial or blaming others. Even if circumstances were complicated, acknowledge your part.Describe the feedback and your response.
- “I received feedback that…”
- “Initially, I reacted by…, but I realized…”
- “I then met with [mentor/dean] and developed a plan to…”
Outline specific behavioral changes.
- Improved time management systems
- Communication training, conflict resolution courses
- Regular check-ins with faculty mentors or advisors
- Documented improvement in subsequent rotations
Back it up with evidence.
- Later clerkship evaluations that mention improved professionalism
- Strong letters highlighting reliability, humility, and teamwork
- Formal remediation completed and cleared by your school
Sample Language for Addressing Professionalism Concerns
In my third year, I was cited for repeated lateness to rounds on my internal medicine rotation. At the time, I was struggling with commute logistics and poor time management, but I did not recognize how my behavior affected the team. After meeting with the clerkship director and academic dean, I created a structured schedule, built in earlier arrival times, and sought feedback weekly from my residents. On my subsequent EM and IM rotations, I consistently arrived early, took responsibility for pre-rounding, and received positive feedback about my reliability. This experience made me more aware of how small actions affect team trust—an awareness I carry with me into every clinical environment.
Programs want to see insight, humility, and consistent improvement. That is especially critical in EM-IM, where professionalism under stress determines how safe and effective you are.
Strategic Application Planning: Turning Red Flags into a Coherent Story
Even with multiple red flags, a thoughtful strategy can significantly improve your chances as a US citizen IMG targeting emergency medicine internal medicine pathways.
1. Build a Clear, Credible Narrative
Your entire application should tell a consistent story:
- Why EM-IM (or EM and IM separately) makes sense for you.
- How your experiences—including setbacks—shaped that interest.
- How you’ve developed the resilience and habits needed for a demanding combined program.
Use your personal statement to integrate:
- Your path as an American studying abroad
- Key clinical experiences in EM and IM
- Brief, honest discussion of red flags with emphasis on growth
Aim for ownership without over-disclosure. Share enough to be transparent, but keep the focus forward.
2. Leverage Targeted Letters of Recommendation
For EM-IM specifically, try to secure:
At least one strong letter from emergency medicine faculty who can:
- Comment on your performance on shift
- Highlight your ability to think quickly yet thoroughly
- Address reliability and teamwork
At least one strong letter from internal medicine faculty who can:
- Speak to your clinical reasoning and longitudinal patient care
- Highlight maturity, follow-through, and communication with consultants/families
If you have a notable red flag:
- A letter from a mentor or program director who knows the context and can attest to your improvement can be powerful.
Give your letter writers:
- An updated CV
- Your personal statement draft
- A brief, honest summary of your red flags and how you’ve addressed them
So they can reinforce your narrative and not be surprised if asked.
3. Program Selection and Realistic Targeting
Even with red flags, you can be strategic:
Apply broadly to:
- A range of EM-IM combined programs (recognizing they are few)
- Strong internal medicine programs with robust critical care or hospitalist tracks
- Emergency medicine programs open to US citizen IMGs
Research:
- Programs with a history of interviewing or matching IMGs
- Hospitals that value diverse paths and non-traditional applicants
- Places where faculty have interest in education and remediation
Consider a “tiered” list:
- Dream EM-IM programs
- Solid categorical EM or IM programs with research/critical care focus
- Safety programs where your profile fits well
For some applicants with multiple or severe red flags, it may be wise to:
- Prioritize strong IM programs first, then later add EM fellowship/acute care focus.
- Or complete a preliminary year in IM or transitional year, then re-apply to EM or EM-IM (with guidance from mentors).
4. Interview Preparation: Addressing Failures and Gaps in Person
Every interviewer who notices your red flag is thinking: “If I bring this up, will the applicant get defensive, evasive, or insightful?”
Prepare concise, honest, non-defensive responses:
- Acknowledge what happened.
- Explain contributing factors (briefly, factually).
- Describe what you changed.
- Highlight your current, improved performance and readiness.
Example for an EM-IM interview:
“I failed Step 1 on my first attempt due to an ineffective study strategy and overcommitting to outside responsibilities. After that, I worked closely with our academic support office to re-structure my study plan around daily timed questions and systematic review of missed concepts. I reduced non-essential activities, passed Step 1 on the second attempt, and improved further on Step 2 CK. Since then, on my EM and IM rotations, I’ve applied the same disciplined approach to preparation and patient care. I’m confident in my ability to handle the exam and cognitive demands of a combined EM-IM program.”
Deliver this calmly, without over-apologizing or sounding rehearsed. Your demeanor is as important as your words.
Frequently Asked Questions (FAQ)
1. As a US citizen IMG, is it realistic to match into EM-IM combined if I have a red flag?
It is more challenging, but not impossible. EM-IM programs are small and selective, so some may screen out applicants with significant exam failures or major professionalism concerns. However:
- Strong Step 2 CK scores, excellent US clinical experience in EM/IM, and compelling letters can offset some red flags.
- A clear, honest explanation and documented improvement are essential.
- You may need to apply broadly and include categorical EM and IM programs in your strategy as well.
Your goal is to show that your red flag is an event in the past, not a predictor of future performance.
2. How much detail should I share when addressing failures or personal issues?
Share enough to make the situation understandable and credible, but not so much that the focus shifts entirely to your struggles. Emphasize:
- The nature of the problem in broad but honest terms.
- The steps you took to address it (treatment, academic support, schedule adjustments).
- Your current stability and readiness for residency.
For sensitive topics (mental health, family trauma), you can be general:
- “I faced a significant family health crisis that required my attention.”
- “I sought treatment for depression and, with therapy and medication, I am now stable and fully able to meet residency demands.”
If you are unsure, discuss the level of detail with a trusted advisor or dean.
3. Does being a US citizen IMG help offset red flags compared with non‑US IMGs?
Being a US citizen removes visa uncertainty, which is a real advantage for some programs. However, in terms of red flags, the core concerns are the same:
- Can you pass boards?
- Will you be reliable and professional?
- Can you function safely in EM and IM environments?
Your US citizenship may make some programs more willing to consider you, but you still need to prove readiness through performance, letters, and a coherent narrative.
4. If I don’t match EM-IM on the first try, how should I use the year before reapplying?
Use the year to actively strengthen your application:
- Seek US clinical roles (research fellow, scribe, clinical coordinator, observerships) in EM or IM.
- Work with mentors to join research or quality improvement projects in acute care, critical care, or hospital medicine.
- Address any deficiencies directly:
- Retake exams if needed (where allowed).
- Obtain new letters emphasizing your growth.
- Reflect and refine:
- Reassess whether EM-IM combined is the right path versus strong categorical EM or IM with later fellowship.
In your reapplication, focus on how you used the extra time intentionally to become a stronger, more committed candidate.
By understanding how program directors interpret red flags, planning your explanations carefully, and aligning your experiences with the demands of emergency medicine internal medicine, you can transform setbacks into evidence of resilience and maturity. As a US citizen IMG and American studying abroad, your path is non-traditional—but with honest reflection, strategic preparation, and strong mentorship, it can also be a compelling one.






















