Why Interoperability in Electronic Health Records Matters More Than Ever
In today’s complex, high‑acuity healthcare environment, your ability as a clinician to access the right information at the right time is often the difference between safe, high‑quality care and preventable harm. Electronic Health Records (EHRs) were supposed to solve this challenge—yet many systems remain fragmented, siloed, and difficult to navigate across institutions.
Interoperability—the capacity of different systems, applications, and devices to exchange, interpret, and use health data seamlessly—is what turns a static EHR into a dynamic clinical tool. For residents, fellows, and early‑career attendings navigating a multi‑hospital ecosystem, understanding interoperability is no longer optional. It directly impacts patient care, clinical workflows, research opportunities, and even your future employability in a healthcare market driven by value-based care and digital transformation.
This expanded guide explains what interoperability really means in the context of Electronic Health Records, why it is central to modern patient care, how it shapes healthcare technology decisions, and what barriers and strategies you should be aware of as you move into practice and leadership roles.
Defining Interoperability in Electronic Health Records
Interoperability in healthcare refers to the ability of various health information systems, software applications, and devices to work together, exchanging and using data consistently and reliably. In an interoperable environment, a patient’s health information can follow them across:
- Different hospitals and clinics
- Outpatient and inpatient settings
- Primary care, specialty care, and ancillary services
- Telemedicine platforms, remote monitoring tools, and wearables
Levels of Interoperability: From Data Exchange to Shared Understanding
Interoperability is often described in three progressive levels. Understanding these is crucial when you hear vendors, administrators, and policymakers talk about “interoperable” systems.
1. Foundational Interoperability: Basic Data Exchange
Foundational interoperability is the most basic level—it ensures that one IT system can send data to another and that the receiving system can receive it.
- Example: A hospital’s EHR sends a discharge summary as a PDF or structured message to a skilled nursing facility.
- Limitation: The receiving system may not be able to automatically integrate or process that data. It may simply store it as an attachment or static document.
This level is like sending a fax electronically: the information is transmitted, but not necessarily usable at scale.
2. Structural Interoperability: Standardized Formats
Structural interoperability defines the format, organization, and syntax of data so that receiving systems can parse and display the content in predictable ways.
- Example standards:
- HL7 v2 messages for lab results and ADT (admission/discharge/transfer) information
- CDA (Clinical Document Architecture) for clinical summaries
- FHIR (Fast Healthcare Interoperability Resources) for modern, API‑driven data exchange
- Clinical example: A lab result sent from an external laboratory appears in your EHR in the correct “Labs” section, with discrete values and reference ranges—not just as a scanned PDF.
This level supports more efficient workflows, but systems still might not fully agree on what each data element means.
3. Semantic Interoperability: Shared Clinical Meaning
Semantic interoperability is the highest and most clinically meaningful level. Here, systems not only exchange data in standard formats, they understand and interpret it the same way.
- Uses standardized clinical vocabularies:
- SNOMED CT for diagnoses and problem lists
- LOINC for lab tests and measurements
- RxNorm for medications
- Clinical example: A diagnosis of “myocardial infarction” from an outside cardiology practice appears in your EHR’s problem list coded in SNOMED CT, allowing:
- Clinical decision support alerts to fire correctly
- Population health algorithms to count that patient in MI registries
- Quality metrics and research queries to identify the patient accurately
Semantic interoperability is what truly enables safe, scalable data sharing, advanced analytics, AI tools, and high‑quality patient care across organizations.

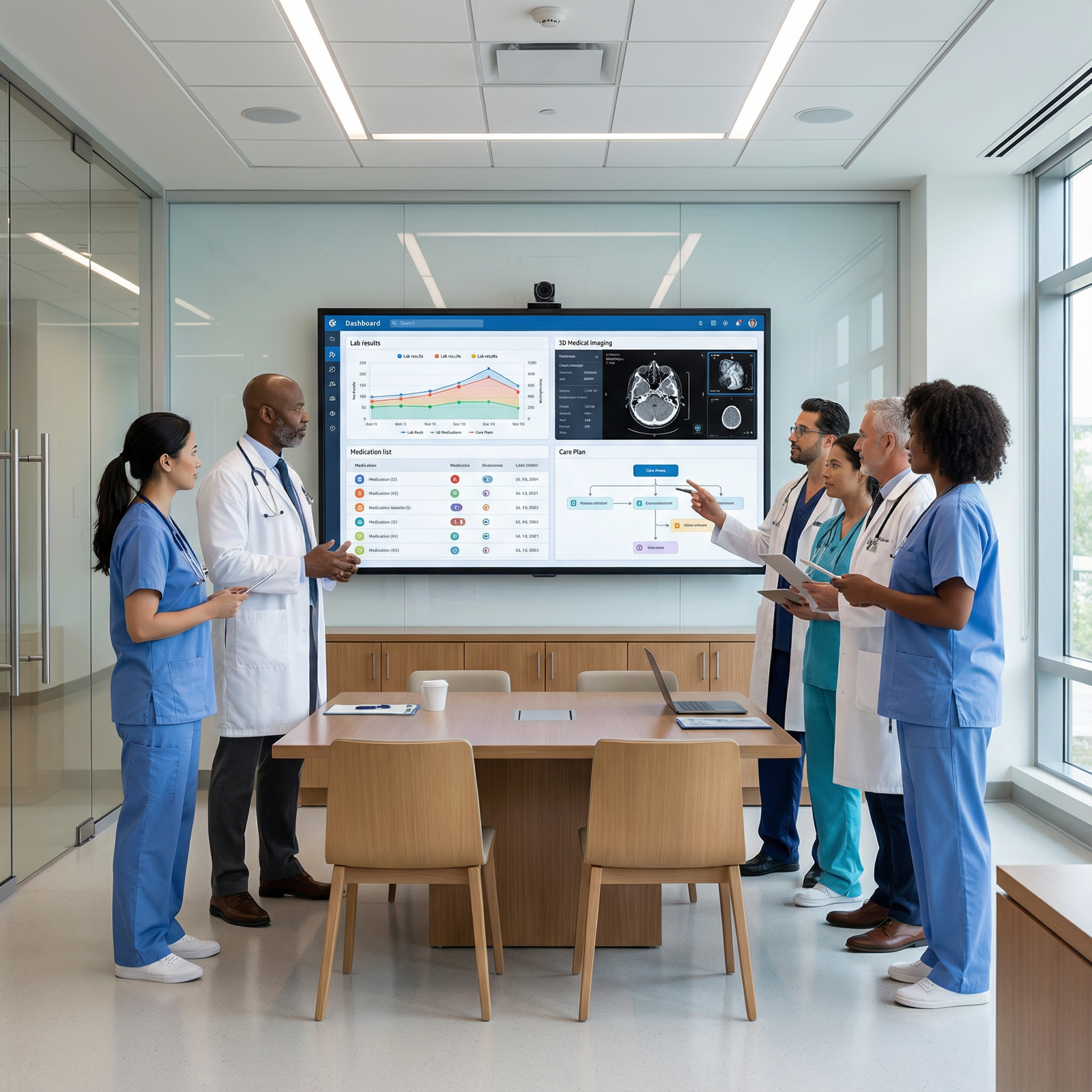
How Interoperability Transforms Patient Care and Clinical Practice
1. Delivering Safer, Higher-Quality Patient Care
Interoperability directly impacts daily clinical decision‑making and patient outcomes.
Comprehensive Patient Profiles at the Point of Care
When EHRs can seamlessly share data, you gain access to:
- Up‑to‑date medication lists from pharmacies and other health systems
- Prior imaging and reports, avoiding unnecessary radiation
- Historical lab values and trends across institutions
- Allergy information and prior adverse drug reactions
- Past operative notes, discharge summaries, and consults
Clinical impact examples:
- You can avoid prescribing a medication that previously caused severe side effects at another facility.
- A patient with chest pain doesn’t need a repeat CT scan if a recent high‑quality study and report are available from another hospital.
- In emergency situations, an interoperable system can immediately surface critical information (e.g., anticoagulant use, baseline creatinine) that changes your management.
Improved Care Coordination Across the Continuum
Modern patient care is rarely confined to a single provider or setting. Interoperability allows:
- Smooth transitions from inpatient to outpatient care, with timely discharge summaries and follow‑up instructions sent to primary care and specialists.
- Coordinated management of chronic conditions (e.g., diabetes, CHF, COPD) across primary care, specialty clinics, home health, and telehealth platforms.
- Real-time communication between EDs, urgent care centers, and primary practices to reduce fragmentation.
For patients with complex, multi‑morbid conditions, interoperability reduces the risk of conflicting treatment plans, duplicated medications, and miscommunication between teams.
Enhanced Patient Safety and Decision Support
With integrated, high‑quality data, EHRs can power robust clinical decision support:
- Drug–drug and drug–allergy interaction alerts based on a complete medication profile, not just the medications prescribed in your institution.
- Renal dosing and lab‑based alerts that include outside laboratory results.
- Sepsis alerts, VTE risk assessments, and other predictive tools that perform better with more comprehensive datasets.
When data is fragmented across non‑communicating systems, these safety nets are incomplete—and occasionally dangerous, if they give a false sense of reassurance.
2. Increasing Efficiency and Reducing Waste
Interoperability is also a powerful driver of operational efficiency and cost savings.
Minimizing Redundant Testing and Procedures
Without access to outside records, clinicians often repeat:
- Imaging studies (CTs, MRIs, echocardiograms)
- Laboratory panels and specialized tests
- Cardiac stress tests, pulmonary function tests, and other diagnostics
Interoperable EHRs and Health Information Exchanges (HIEs) allow you to:
- Quickly verify whether a recent, clinically adequate study already exists.
- Focus on additional or complementary testing rather than repeating what’s already been done.
- Reduce patient burden, radiation exposure, and overall healthcare costs.
For health systems in value‑based contracts or risk‑sharing arrangements, reducing redundant testing is not just clinically appropriate—it’s financially essential.
Streamlining Administrative and Clinical Workflows
Interoperable systems can automate and simplify many routine tasks:
- Admission and registration: Patient demographics, insurance information, and primary care provider details can be pulled from other systems or HIEs.
- Referral management: Clinical data packages (history, imaging, labs) accompany referrals so specialists can triage more efficiently.
- Documentation: Prior history and results can be reconciled instead of manually re‑entered, which reduces errors and documentation burden.
For residents and early‑career physicians, time saved from hunting for outside records or copying data manually can be reinvested in direct patient care, teaching, or research.
Timely Access to Critical Information
In acute care scenarios—stroke, STEMI, sepsis—minutes matter. Interoperability can:
- Surface outside imaging or labs within minutes rather than hours of faxing and scanning.
- Provide real-time access to prehospital EMS records and medication administration.
- Enable rapid verification of prior conditions (e.g., previous tPA, anticoagulant use) that change emergent treatment decisions.
This timeliness not only improves patient care, it helps clinicians feel more confident and supported in high‑stakes situations.
3. Supporting Population Health, Research, and Innovation
Interoperable EHR data is foundational for modern population health management and healthcare technology innovation.
Aggregated Data for Population Health and Quality Improvement
When data can flow across organizations and systems, you can:
- Build disease registries (e.g., heart failure, diabetes, cancer) that capture patients regardless of care location.
- Track readmissions, ED use, and follow‑up adherence across networks.
- Measure quality metrics (e.g., screening rates, blood pressure control, A1c levels) more accurately.
This supports:
- Targeted outreach to high‑risk patients
- Performance on value‑based contracts and pay‑for‑performance measures
- Quality improvement initiatives that rely on robust, longitudinal data
Early Detection of Health Trends and Public Health Surveillance
Interoperable systems also power:
- Syndromic surveillance (e.g., influenza‑like illness, COVID‑like symptoms)
- Early identification of outbreaks or clusters of rare events
- Monitoring of vaccination rates and preventive care across populations
Health agencies can use aggregated, de‑identified EHR data for real‑time situational awareness, helping them deploy resources and interventions more effectively.
Fueling Research, AI, and Advanced Analytics
For clinician‑scientists and those interested in informatics or digital health:
- Interoperable EHR data creates large, diverse datasets for observational research, pragmatic trials, and outcomes studies.
- Machine learning models for risk prediction or clinical decision support perform better with cleaner, more standardized, and more complete data.
- Multi‑site collaboration becomes simpler when participating institutions can map to common data models and coding standards.
As you think about career pathways after residency, literacy in interoperability and data standards is increasingly relevant for roles in clinical informatics, quality leadership, digital health startups, and health system administration.
Barriers to Achieving True Interoperability
Despite the clear benefits, full interoperability remains elusive in many settings. As a future leader or decision‑maker, it’s important to understand the main obstacles.
1. Inconsistent Standards and Data Fragmentation
- Different EHR vendors and ancillary systems may implement HL7, FHIR, and other standards in partially incompatible ways.
- Variation in coding practices (e.g., free text vs. standardized terminologies) reduces semantic interoperability.
- Legacy systems may not support modern interfaces or APIs, making integration complex and costly.
Result: Even when data is technically exchanged, it may not be usable in a consistent, computable form.
2. Data Security, Privacy, and Regulatory Concerns
Healthcare data is highly sensitive and heavily regulated:
- Organizations must comply with HIPAA (in the U.S.) and other privacy regulations.
- Each additional interface or data‑sharing connection expands the “attack surface” for cyber threats.
- Concerns about ransomware, unauthorized access, and data breaches may cause organizations to limit data sharing.
Balancing robust Data Security with meaningful data exchange is a core design challenge in healthcare technology.
3. Financial and Operational Costs
- Upgrading legacy systems, implementing interfaces, and maintaining integrations require significant investment.
- Smaller practices, rural hospitals, and safety‑net institutions may lack capital and IT resources.
- Short‑term disruption during implementation can strain already overburdened clinical teams.
From a leadership perspective, you’ll need to think about return on investment, funding models, and phased implementation strategies.
4. Resistance to Change and Workflow Disruption
- Clinicians and staff may resist new systems or workflows, especially if they feel imposed from above or poorly designed.
- Poorly implemented interoperability solutions can generate alert fatigue, duplicates, or confusing documentation.
- Competing priorities—productivity targets, staffing shortages, regulatory deadlines—can delay adoption.
Effective change management, frontline engagement, and user‑centered design are essential to overcome this barrier.
5. Vendor Lock‑In and Competitive Dynamics
- Some EHR vendors historically created “walled gardens,” making it difficult or expensive to connect with competitors’ systems.
- Health systems may be reluctant to share data fully with perceived competitors in their market.
- Contractual and technical barriers can hinder true cross‑vendor interoperability.
Recent regulatory moves, such as information blocking rules in the U.S., are pushing vendors and organizations toward more open, patient‑centric data exchange—but cultural and market barriers persist.
Practical Strategies to Advance EHR Interoperability
As a resident or early‑career physician, you may not be making IT purchasing decisions yet—but you do influence how systems are used, and you can play a critical role in advocating for better interoperability.
1. Support Adoption of Modern Standards and APIs
Encourage your institution to:
- Implement FHIR‑based APIs for data access and integration with third‑party apps.
- Standardize coding of problem lists, allergies, procedures, and labs using SNOMED CT, ICD‑10, LOINC, and RxNorm.
- Participate in national or regional initiatives that promote cross‑vendor interoperability.
Clinically, you can:
- Use standardized terms rather than ambiguous free text where feasible.
- Help identify where poor coding or data duplication is creating patient safety risks.
2. Strengthen Collaboration Across Stakeholders
Interoperability is not purely a technical problem; it’s an ecosystem challenge.
- Clinicians, administrators, IT teams, EHR vendors, health information exchanges (HIEs), and policymakers must align around common goals.
- Engage with clinical informatics committees, quality councils, or digital health working groups at your institution.
- When possible, provide frontline feedback on what data you need across settings and how you use it in real clinical scenarios.
Initiatives led by national bodies (e.g., ONC in the U.S.) are increasingly emphasizing real‑world usability and minimizing information blocking—your voice can help shape local implementation.
3. Invest in Training, Literacy, and Change Management
Interoperability features are only helpful if clinicians know they exist and how to use them:
- Ask for training on how to locate outside records, use HIE portals, and reconcile external data within your EHR.
- Participate in pilot projects or user‑testing sessions for new interoperability tools.
- Provide constructive feedback on usability, workflow fit, and alert design.
Understanding the basics of healthcare technology and interoperability will also make you more competitive for leadership, informatics, and health system roles.
4. Foster a Culture of Ethical Data Sharing
Culturally, a mindset shift is needed:
- Move from “owning” patient data within one organization to stewarding data in the patient’s best interest across the care continuum.
- Encourage policies that share clinically relevant information with outside providers and with patients themselves (e.g., open notes, integrated patient portals).
- Support regional HIE participation and cross‑organizational care coordination programs.
As a clinician, you can reinforce that withholding accessible, relevant clinical data is increasingly seen as a patient safety and quality issue—not a competitive advantage.
5. Prioritize Data Security and Privacy by Design
Robust Data Security must be built into every interoperability initiative:
- Ensure encryption in transit and at rest for health data.
- Advocate for strong authentication (e.g., multi‑factor) and role‑based access controls.
- Support regular security audits, penetration testing, and incident response planning.
- Educate patients about how their data is used, their rights to access, and how privacy is protected.
Security and interoperability are often framed as competing priorities, but modern architectures can and should support both.

FAQs: Interoperability, EHRs, and Your Future Practice
Q1: How does interoperability affect my day-to-day work as a resident or early-career physician?
Interoperability directly shapes how quickly and completely you can see a patient’s history, medications, imaging, and prior care. In practice, it means less time chasing faxes and phone calls, fewer redundant tests, better-informed decisions, and safer prescribing. It also affects your documentation workload—well‑designed interoperable systems reduce manual data entry and make it easier to reconcile outside information into your notes and problem lists.
Q2: What role does interoperability play in telemedicine and virtual care?
For telemedicine to be safe and effective, clinicians must be able to see a comprehensive record of the patient’s health, not just what’s captured during a video visit. Interoperability allows telehealth platforms to pull in past diagnoses, labs, imaging, and medications from EHRs, and to push visit notes and orders back into those systems. This ensures continuity of care, prevents fragmented documentation, and enables integrated decision support—even when care is delivered remotely.
Q3: How are patients personally affected when EHRs are not interoperable?
Patients may experience:
- Repeated tests and procedures, often at significant cost
- Conflicting treatment plans or medications from different providers
- Delays in diagnosis or treatment while records are requested and manually reviewed
- Frustration at having to repeat their history multiple times
In contrast, interoperable systems support smoother care transitions, better coordination, and more transparent access to their own records through patient portals and apps.
Q4: What are some key interoperability standards I should be familiar with?
For clinical practice and informatics literacy, it’s helpful to know:
- HL7 v2: Widely used messaging standard for lab results, ADT, and other clinical data
- FHIR (Fast Healthcare Interoperability Resources): Modern, web‑based standard enabling APIs and app integration with EHRs
- SNOMED CT: Standardized terminology for clinical concepts and diagnoses
- LOINC: Codes for lab tests and clinical measurements
- RxNorm: Standardized naming for medications
You don’t need to implement these yourself, but understanding their purpose helps you interpret how your EHR organizes data.
Q5: How can I, as an individual clinician, advocate for better interoperability and data security?
You can:
- Join or collaborate with your institution’s clinical informatics or EHR optimization groups.
- Provide specific examples where lack of interoperability compromised care or efficiency.
- Encourage standardized coding practices and good data hygiene in your own documentation.
- Support participation in regional HIEs and use available tools to access outside records.
- Advocate for investments in secure, standards‑based interfaces rather than workarounds like faxing and scanning.
Clinician voices are influential; framing interoperability as a patient safety and quality issue often resonates with both administrators and policymakers.
Interoperability in Electronic Health Records is no longer just a technical aspiration—it is a foundational requirement for safe, efficient, and patient‑centered care. As you move from training into independent practice and potential leadership roles, your understanding of interoperability, healthcare technology, and data security will shape not only how you care for individual patients but also how you help transform systems to deliver better care for entire populations.





















