
Understanding “Malignant” Residency Programs as a Caribbean IMG
For Caribbean international medical graduates aiming for a preliminary medicine year (prelim IM) in the United States, the residency match is already a high‑stakes, high‑stress process. Layer on the fear of landing in a malignant residency program, and it can feel overwhelming—especially if you’re relying on a prelim year for future categorical IM, anesthesiology, radiology, neurology, or PM&R training.
“Malignant” isn’t an official ACGME term. In resident culture, it refers to programs with:
- Chronic disrespect toward residents
- Unsafe workloads and lack of supervision
- Toxic culture of blame, intimidation, or retaliation
- Poor educational value and little support for career goals
As a Caribbean IMG—whether from SGU, Ross, AUC, Saba, or other schools—you may already worry about reputation and visa issues. That vulnerability can make you a target for exploitative or toxic environments. This article will help you:
- Understand what “malignant” looks like in preliminary medicine specifically
- Recognize residency red flags before ranking a program
- Use available data to evaluate Caribbean medical school residency outcomes
- Ask high‑yield questions on interview day
- Make safer rank list decisions—even if your options feel limited
Why Preliminary Medicine Is a Special Risk Zone
A preliminary medicine year is unique compared with a categorical IM position:
- It’s a one‑year contract (not 3 years)
- Residents are often viewed as a workforce stopgap rather than long‑term trainees
- Many prelims are matched into advanced specialties (anesthesia, neuro, etc.), not invested in IM long‑term
- Program leadership may prioritize categorical residents for teaching and opportunities
That combination can turn some programs into service-heavy, education-light experiences, especially for IMGs. For a Caribbean IMG, it’s critical to understand how you might be treated as a prelim versus categorical resident.
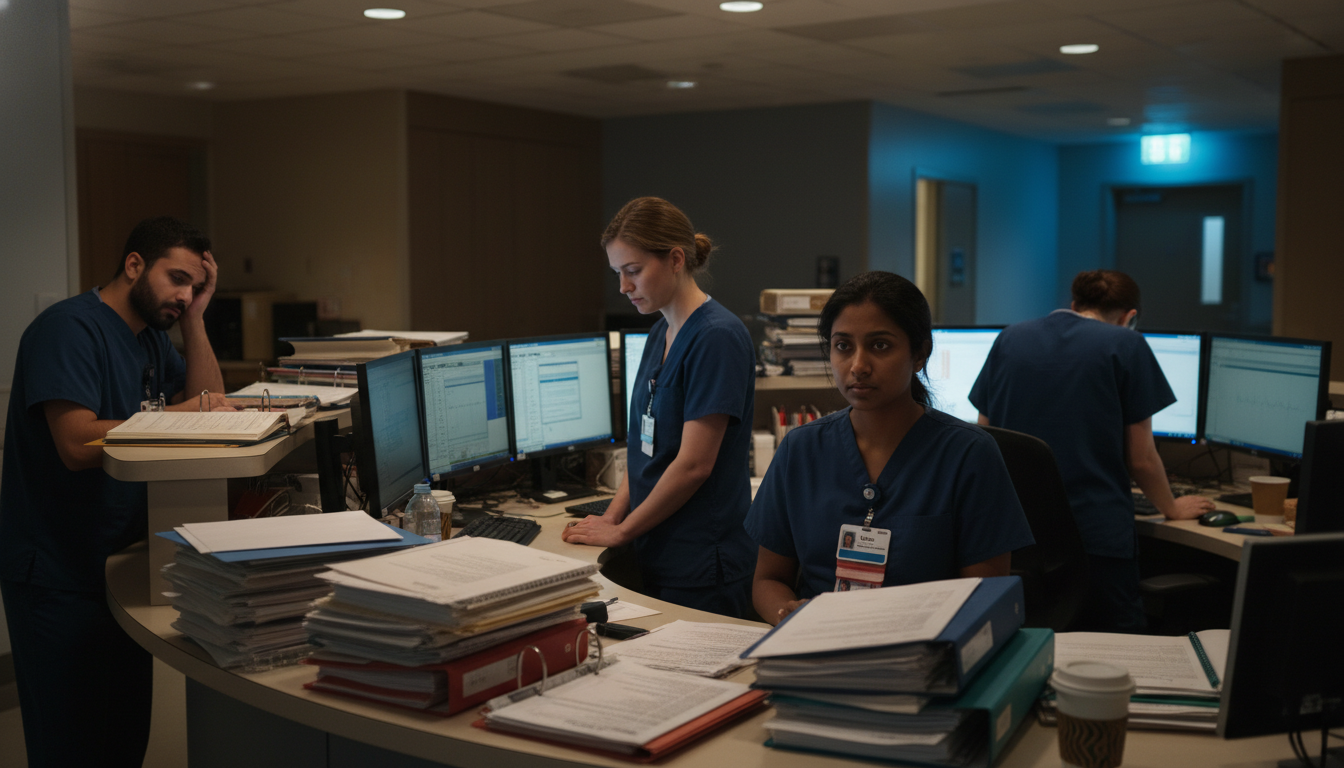
How Malignancy Shows Up in Prelim IM
Common malignant patterns in preliminary medicine programs:
“Scut-heavy” year with minimal teaching
- Prelims primarily do admissions, cross-cover, and paperwork
- No consistent didactics, bedside teaching, or feedback
- Little to no faculty mentorship for advanced specialty plans
Unequal treatment of IMGs and prelims
- IMGs get heavier call, more nights, less elective time
- Prelims excluded from conferences, research, or leadership roles
- Comments like “You’re just here for a year” or “You IMGs should be grateful for anything”
No support for next steps
- No real help with LORs, interview scheduling, or fellowship planning
- Minimal mentorship on career transitions after the prelim year
- Poor track record of prelims successfully moving into advanced positions or categorical IM spots
Burnout and safety issues
- Chronic duty hour violations
- Unsafe patient caps and poor supervision
- Hostility if residents call attendings for help or raise safety concerns
For Caribbean grads, whose visa, financial, and career trajectories may hinge on this single year, avoiding these toxic program signs is crucial.
Concrete Red Flags: How to Spot a Malignant Residency Program
You won’t find a label that says “malignant” on the program website. Instead, you have to interpret patterns from multiple sources: FREIDA, program websites, interviews, social media, GME reports, and personal networks. Below are the major residency red flags, tailored to Caribbean IMGs and prelim IM positions.
1. Reputation Among Residents & Alumni (Especially IMGs)
Informal reputation carries a lot of truth. Warning signs:
- Multiple residents describe it as “toxic” or “malignant” on forums, Reddit, or word of mouth
- Caribbean IMGs report:
- “I was worked to the bone with no support”
- “Attendings were hostile if I asked questions”
- “They made it clear IMGs were second-class”
Actionable tips:
- Reach out to Caribbean alumni from your school who matched there—busy SGU residency match lists and other Caribbean medical school residency outcomes are a starting point. Ask:
- “Would you rank this program again as a prelim?”
- “How did they treat IMGs versus US grads?”
- “Did you feel supported to get into your advanced specialty?”
If two or more independent sources call the environment “toxic,” consider it high risk unless you have no alternatives.
2. High Turnover, Non-Renewals, or Withdrawals
A classic marker of a malignant residency program is churn—residents constantly leaving or being “counseled out.”
Watch for:
- Many residents with “transferred from” or “prior training at” in their bios on the website
- Gaps in the resident roster (missing PGY‑2 or PGY‑3 names)
- Rumors or reports of multiple terminations or non‑renewed contracts
Ask residents discreetly:
- “Has anyone left the program or transferred in the last few years? Why?”
- “Does the program support residents who are struggling, or do they get pushed out?”
One or two cases over years may be benign. A pattern suggests serious problems.
3. Chronic Duty Hour Violations and Workload Exploitation
Excessive workload is a hallmark of malignant culture, especially for prelim IM and IMGs.
Red flags:
- Residents say things like:
- “We’re always finishing notes at home”
- “We routinely stay 2–3 hours beyond our shifts”
- “We’re told not to log violations”
- Call schedule is extremely heavy for prelims:
- Many 24+4 calls, q3 or q4 nights without recovery
- Frequent “short call” that regularly runs long
- Prelims have higher patient caps or more cross-coverage than categorical residents
You can ask:
- “How often do you leave on time?”
- “Do you ever feel pressured not to report duty hour violations?”
- “How are admissions divided between prelim and categorical residents?”
If the tone is: “We make it work, just don’t complain,” that’s a strong warning.
4. Hostile or Fear-Based Culture
Culture is the core of malignancy. Key toxic program signs:
- Attendings or senior residents publicly humiliate juniors
- Mistakes are met with shaming rather than teaching
- Residents fear retaliation for:
- Reporting safety events
- Asking for mental health time
- Requesting schedule accommodations for health or family emergencies
Ask questions like:
- “What happens if a resident misses something important on a patient?”
- “How does the program respond if a resident is struggling?”
- “Can residents safely give feedback about faculty or administration?”
You’re listening less to the words and more to the emotional undercurrent—do they seem genuinely safe to speak up, or cautious and guarded?
5. Lack of Educational Structure for Prelims
A residency can be busy but still high-quality. The malignant variant is busy, disorganized, and educationally hollow—especially for prelims.
Signs:
- Prelims excluded from:
- Morning report
- Board review
- Scholarly projects
- Minimal or no:
- Protected didactic time
- Simulation training or procedure workshops
- Structured feedback or mid-year evaluations
- When you ask about prelim-specific teaching, the answer is vague:
- “You’ll learn by doing”
- “We don’t really separate prelims from categoricals, so there’s no specific curriculum”
For Caribbean IMGs who may need strong letters and skill-building to progress, this lack of structure can be devastating.
6. Poor Transparency About Outcomes and Support
A high-quality prelim program should proudly show:
- Where their prelim graduates go (advanced specialties, categorical IM spots)
- How often prelims secure SGU residency match–style success stories: anesthesiology, radiology, etc.
Red flags:
- No data on prelim graduates’ next steps
- Evasive answers when you ask:
- “What percentage of prelims match into advanced positions each year?”
- “How many prelims convert to categorical IM here or elsewhere?”
If they minimize your question or say, “It depends” without numbers, consider why.
7. Visa Hostility or Administrative Neglect of IMGs
For Caribbean IMGs, visa and credentialing issues are not trivial—your legal ability to stay in the country depends on them.
Red flags:
- History of DS‑2019 or H‑1B delays leading to late starts
- Residents needed to hire lawyers or intervene repeatedly
- Program saying:
- “We’ve never done H‑1B before; you’ll have to figure it out”
- “We can’t guarantee anything—HR handles that”
Ask directly:
- “How many current residents are on a visa?”
- “Has any Caribbean IMG ever had issues starting on time due to visa delays?”
- “Who in the GME office is the point person for visa issues?”
A strong program has clear processes and recent IMG success stories.
Doing Your Homework: Pre-Interview Research for Caribbean IMGs
Before you even accept an interview, you can screen out many high‑risk programs.
1. Use Public Data (FREIDA, Program Websites, NRMP)
- Review FREIDA and the program’s website for:
- Number of prelim positions vs categorical
- Faculty-to-resident ratio
- Presence of fellowships (a rough marker of academic environment)
- Look for:
- Transparent lists of current residents and alumni
- Evidence of Caribbean graduates among them
If a program has no identifiable Caribbean IMGs in recent years, it doesn’t automatically mean malignancy—but it suggests you should press harder about how they treat IMGs.
2. Track Caribbean Medical School Residency Outcomes
Your own school is a valuable reference:
- Check SGU residency match or your school’s match list for that program:
- Has your school sent multiple graduates there?
- Do they go back year after year, or was it a one-time placement that never repeated?
Patterns to trust:
- Repeated placements over several years → program likely workable for Caribbean grads
- One Caribbean graduate from 8 years ago and none since → proceed with caution and ask direct questions
3. Read Between the Lines of Online Reviews
Sites like Reddit, Student Doctor Network, and specialty forums can be noisy, but look for overlapping themes:
- Repeated mentions of:
- “Overworked, under-supported”
- “Residents are scared of leadership”
- “Caribbean IMGs are used for the worst rotations”
No single anonymous post should decide your rank list. But if 3–4 independent sources describe similar problems, that’s strong evidence.

High-Yield Interview Questions to Detect Toxic Program Signs
The interview day is your best window into the inner workings of a program. As a Caribbean IMG seeking a preliminary medicine year, you should intentionally probe culture, workload, and support.
Below are targeted questions, sorted by who to ask and what to listen for.
Questions for Current Residents (Preferably IMGs and Prelims)
Workload & Duty Hours
- “On your busiest rotations, what does a typical day look like? When do you usually go home?”
- “How often do you log duty hour violations? What happens when you do?”
Good signs:
- “We’re busy, but we leave close to sign-out most days.”
- “We’ve logged violations and the program adjusted coverage.”
Red flags:
- “We never log violations; it just causes trouble.”
- Nervous laughter, vague answers, or “it depends” without examples.
Culture & Safety
- “Is it safe to admit when you don’t know something?”
- “Have you seen residents punished for mistakes or speaking up?”
Healthy answer:
- “We have M&Ms, but they’re blame-free and focused on systems.”
Toxic answer:
- “You just have to be careful what you say and to whom.”
Treatment of Caribbean IMGs
- “Are IMGs treated any differently from US grads here?”
- “Do prelims carry similar responsibilities as categoricals?”
Green flags:
- “Our chief last year was an IMG.”
- “We don’t distinguish; we cover the same services and get similar opportunities.”
Red flags:
- “Prelims take more nights because they’re only here a year.”
- “IMGs usually get the tougher rotations first.”
Support for Future Plans
- “Where did recent prelim grads go after this year?”
- “Do faculty help with letters and networking for advanced positions?”
Good:
- Residents can name recent prelims and their destinations.
Bad:
- “I’m not sure what happened to most of them.”
Questions for Program Leadership
Program Philosophy on Prelims
- “How do you view the role of preliminary medicine residents within the department?”
Positive:
- “Prelims are fully integrated into our teaching and mentorship structure.”
Concerning:
- “They mainly help us staff the services, but they’re welcome at conferences.” (Emphasis on service over learning.)
Outcomes Data
- “What proportion of your prelims match into advanced specialties or categorical IM within 1–2 years?”
Green flag:
- They can quote approximate percentages and provide examples.
Red flag:
- “We don’t really track that; they go all over.”
Feedback & Grievances
- “How do residents provide feedback about the program? Can you share a recent example of feedback that led to change?”
Healthy:
- Leadership gives a clear example of a change prompted by resident input.
Malignant:
- “We have anonymous surveys,” but no examples of responsive change.
Support for IMGs and Visas
- “How many current residents are on visas, and who helps them with the process?”
- “Have any residents had issues starting late due to visa delays in recent years?”
Reassuring:
- Concrete examples of recent, successful visa processing and clear internal support.
Worrisome:
- No clear point person; vague answers like “HR takes care of that.”
Making Rank List Decisions When Options Are Limited
Caribbean IMGs often feel pressure to rank every program that offers an interview, fearing they may otherwise go unmatched. But a truly malignant residency program can cause long-term harm: burnout, mental health crises, and poor career trajectories.
1. How Risky Is “Malignant” vs. “Going Unmatched”?
This is deeply personal and complex. Factors to consider:
- Your Step scores, clinical performance, and repeat applicant status
- Whether you already have an advanced position secured
- Your visa status and ability to reapply or pursue other clinical routes
As a rule of thumb:
- A simply busy or imperfect prelim program may still be worth ranking, especially if alternatives are few.
- A clearly malignant program, with multiple strong red flags (hostility, persistent duty hour abuse, IMG discrimination, lack of supervision), may be worse than not matching—particularly if you have some chance at reapplying or pursuing a different pathway.
2. Prioritizing Among Imperfect Programs
Most programs will have some drawbacks. Focus on what matters most for your one-year prelim:
- Safety and culture → non-negotiable
- Supervision and teaching → you must come out competent and confident
- Support for next steps → strong letters, time to interview for advanced/categorical spots
- Visa and administrative competence → essential for Caribbean IMGs
It’s reasonable to accept:
- Busy services
- Limited research
- Small city or less glamorous location
It’s not reasonable to accept:
- Systemic disrespect or abuse
- Repeated cover-ups of patient safety issues
- A pattern of IMGs being scapegoated or overworked
3. Strategic Use of Backup Options
To reduce pressure to tolerate malignancy:
Consider a broader application strategy from the start:
- Community-based IM programs with a history of Caribbean grads
- Transitional year programs with solid reputations
- Less competitive regions or smaller cities
Use your school’s network:
- SGU residency match data and similar lists from your school can highlight programs that consistently take Caribbean IMGs and are less likely to be toxic.
Discuss with advisors:
- Ask specifically: “Have you ever heard this program described as malignant or toxic?”
Frequently Asked Questions (FAQ)
1. Are all busy community programs “malignant”?
No. High workload alone does not equal malignancy. Many community prelim IM programs are busy but supportive, with approachable attendings and strong camaraderie. Malignancy involves culture and response to stress—how the program treats residents under pressure, handles errors, and responds to feedback.
Look for:
- Respectful interactions
- Evidence of resident advocacy
- Reasonable response when residents raise concerns
2. How can I tell the difference between “just one bad review” and a truly toxic program?
Single anecdotes—especially anonymous ones—should be weighed cautiously. What matters is pattern and consistency:
- Multiple independent residents or alumni sharing similar concerns
- Overlap between online reviews, your school’s advisors, and what you see/feel on interview day
- Clear structural red flags (high turnover, obvious duty hour abuse, evasive leadership)
If you see 3 or more major red flags from different sources, treat the program as high risk.
3. As a Caribbean IMG, do I have to accept a malignant program just to get into the system?
You should not feel forced to endure abuse or unsafe training. However, your decision must consider:
- Your realistic match chances
- Alternative pathways (research positions, reapplication strategies, broader specialty choices)
- Visa constraints
Work closely with mentors who understand Caribbean medical school residency trends and can help estimate your risk. Sometimes, ranking slightly less competitive but supportive programs above more prestigious but toxic ones is the safest strategy.
4. Are university-affiliated prelim IM programs always safer than community ones?
Not always. Academic affiliation can bring resources and structure, but doesn’t guarantee non-malignancy. Some malignant programs exist within brand-name institutions; some of the most humane, supportive environments are at smaller community hospitals.
Evaluate each program on:
- Resident reports of culture and safety
- Transparency about outcomes
- Treatment of IMGs and prelims
- Responsiveness to feedback
By approaching the process systematically—researching programs, recognizing residency red flags, asking focused questions, and leveraging your Caribbean IMG network—you can significantly reduce the risk of landing in a malignant residency program. A preliminary medicine year should be a launching pad, not a trap. Your goal is simple: find a place where you will be worked hard, taught well, treated fairly, and supported into the next phase of your career.






















