
Understanding Resident Turnover as a DO Applicant in Orthopedic Surgery
When you’re a DO graduate targeting orthopedic surgery—a historically competitive and often MD-dominated specialty—you can’t afford to overlook warning signs in residency programs. One of the most important red flags is resident turnover: residents leaving the program early, transferring out, or an unusually high number of residents failing to complete training.
For a DO graduate, the osteopathic residency match (now unified under the NRMP system) still carries unique challenges: you may be more vulnerable to unsupportive cultures, hidden bias, and weak educational environments. Programs with frequent resident departures or constant “gaps” in classes can signal deeper program problems that may directly affect your training, mental health, and eventual ortho match success.
In this article, we’ll break down:
- Why resident turnover matters specifically for DOs in orthopedic surgery
- Concrete warning signs to look for during interviews, socials, and research
- How to ask tactful but revealing questions
- How to interpret what you learn and protect your career
Why Resident Turnover Matters So Much in Orthopedic Surgery
Resident turnover happens everywhere—people have legitimate reasons to leave: family emergencies, spouse relocation, significant health issues, or rare, genuine misfit with the specialty. Isolated cases are not necessarily a resident turnover red flag.
But in orthopedic surgery, patterns of residents leaving a program or ongoing “holes” in the call schedule can indicate structural issues that will impact:
- Your operative exposure
- Your board pass rates
- Your fellowship prospects
- Your physical and emotional well-being
Unique Vulnerabilities for DO Graduates
As a DO graduate, these patterns carry additional weight:
Subtle or overt bias
Programs with poor experience training DO graduates—or with unspoken bias—may inadvertently make your experience harder: less support, assumptions about your knowledge, or fewer high-value opportunities. If multiple DOs have left or transferred, that’s important to know.Less margin for a bad fit
Orthopedic surgery is already demanding. If you train in a chaotic, understaffed, or toxic environment and struggle to perform, it can affect:- Letters of recommendation
- Faculty advocacy for fellowship
- Your reputation within the small ortho community
Educational risk
In weaker programs, DO residents may be pushed disproportionately into service-heavy roles with limited structured teaching, especially if there’s a preexisting hierarchy favoring MD grads or “home-grown” students.
So, the pattern and context of residents leaving a program is critical data—especially for a DO graduate trying to secure a strong foothold in this specialty.
Concrete Warning Signs of Problematic Resident Turnover
Not all turnover is bad. Your job is to discern normal variation from systemic program problems. Below are specific warning signs you can actively look for and verify.
1. Multiple Recent Residents Leaving the Program
A single resident departure in 5–10 years can be benign. But watch for:
- More than one resident leaving or transferring from the same class or adjacent classes
- PGY-2s or PGY-3s who have left recently without clear reasons
- Faculty or residents vaguely referencing people who “moved on” or “decided this wasn’t for them” without detail
Why it matters in ortho:
Orthopedic surgery has one of the strongest “tribe” cultures in medicine. Multiple departures suggest something seriously misaligned in expectations, workload, supervision, or culture.
Follow-up questions to ask (residents, not faculty):
- “In the last 5 years, how many residents have left the program before finishing?”
- “Did they transfer to other ortho programs, switch specialties, or leave medicine entirely?”
- “How did the program handle it—were their reasons understood and addressed?”
You’re looking for both the number and the tone of the answer. Defensiveness, abrupt topic changes, or vague explanations are concerning.
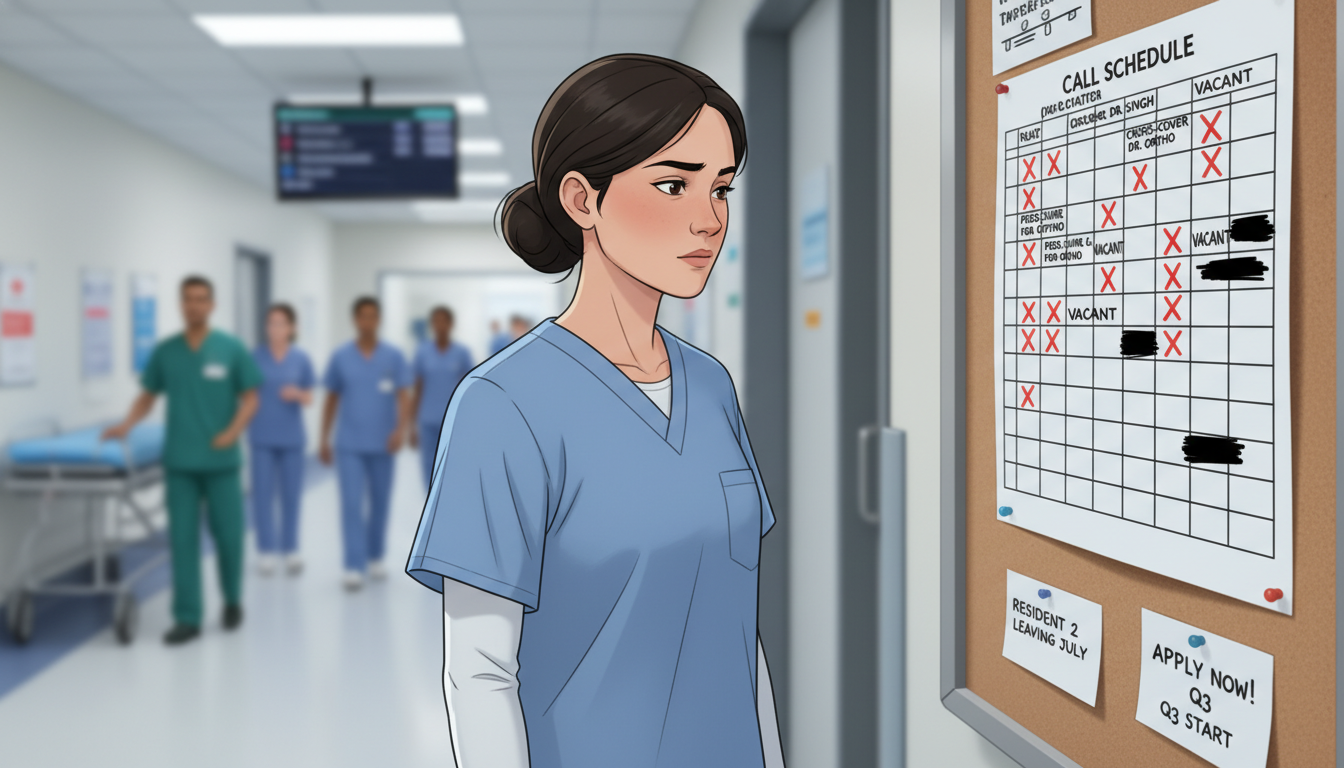
2. Chronic Understaffing and Persistent Gaps in Classes
This is a classic and highly visible warning sign:
- Missing residents in one or more PGY classes (e.g., a PGY-3 class with only 2 residents when it should have 4–5)
- Residents frequently covering multiple services or locations simultaneously
- Call schedules showing:
- “TBD,” “float,” or “cross-cover from PGY-2” routinely
- Night float systems stretched thin
- Faculty or chief residents admitting they “never seem to be fully staffed”
Why it matters:
Constant understaffing increases:
- Burnout and resentment
- Risk of medical errors
- Poor operative experience (you’re plugging service holes instead of learning)
Orthopedic surgery context:
Subspecialty rotations (trauma, spine, sports, joints, hand, pediatrics) require focused time. If resident coverage is patchy, you may miss critical cases—directly impacting case logs and fellowship competitiveness.
What you might hear that’s concerning:
- “We’re working on recruiting a PGY-3 transfer; we’ve had a couple people leave recently.”
- “We’re short on seniors, so juniors have had to step up a lot this year.”
- “It’s been tough, but we’re managing.”
Individually, not damning. Together, especially across multiple classes, they signal chronic turnover.
3. Defensive or Evasive Responses About Past Residents
You are absolutely allowed to ask about residents leaving the program. Programs that react poorly to this question raise red flags about transparency.
Warning behaviors:
- Faculty or residents quickly changing the subject
- “We don’t really discuss that.” (without ANY explanation)
- “They just weren’t a good fit” repeated with different names and years
- Blaming all departed residents (“lazy,” “weak,” “not cut out for ortho”) without ever acknowledging systems issues
How this relates to DO applicants:
If a DO resident left and is always described negatively, ask yourself:
- Is the program introspective at all?
- Could there be a pattern of blaming individuals—especially DOs—rather than acknowledging program structure or culture issues?
A healthy response might sound like:
“We did have a PGY-2 leave a few years ago due to family reasons. Another resident changed to PM&R after realizing ortho wasn’t their long-term fit. We took those situations seriously and made adjustments where we could.”
A defensive or hostile response is a resident turnover red flag you shouldn’t ignore.
4. Excessive Reliance on Non-Resident Labor to Cover Core Work
Turnover often shows up as heavy reliance on:
- Physician assistants (PAs) or NPs doing much of the core floor work
- Contracted “moonlighters” covering night ortho call
- Community surgeons taking emergency cases with minimal resident involvement
- Rotating residents from other specialties filling key service roles
Some PA/NP and collaborative coverage is normal and can be beneficial. But in a struggling ortho program:
- PAs function as the continuity providers while residents constantly rotate and just “drop in”
- Residents miss operative opportunities because faculty “prefer the PA” who’s always there
- Night coverage is so outsourced that residents get limited emergency/trauma experience
For a DO graduate trying to build a solid foundation for fellowship, you want high resident involvement, not a service model where residents are optional.
Questions to ask:
- “How are PAs and NPs integrated with the resident team? Does their presence increase or decrease your operative time?”
- “How often do residents scrub urgent/emergent cases after hours, versus attendings or moonlighters handling them alone?”
You’re looking for evidence that residents—not ancillary staff—are the educational priority.
5. Poor Board Pass Rates, Case Logs, or Fellowship Match Outcomes
Resident turnover is often a symptom of deeper educational problems. Some concrete markers:
- Below-average ABOS board pass rates
- Chronic remediation or delayed graduation
- Consistent under-reporting of case logs or missing case categories
- Weak fellowship placements compared with peer institutions
You won’t always find this info easily, but ask:
- “How have your residents performed on the OITE and ABOS exams over the last 5 years?”
- “Can you share recent trends in fellowship match for your graduates?”
- “Have you had residents struggle to meet case minimums?”
If residents have left the program and remaining residents are still struggling, the problem is institutional—not just a few “bad fits.”
For DOs, these outcomes heavily influence future perceptions:
- A DO graduating from a strong program → easily competitive for top joints/spine/sports fellowships
- A DO graduating from a program known for weak training or high turnover → may face questions or assumptions, fair or not
6. Culture of Burnout, Fear, and Blame
Multiple residents leaving frequently reflects an unhealthy culture:
- Seniors who publicly belittle juniors
- Attendings who normalize humiliation as “old school ortho”
- Residents talking openly about “just surviving” or “getting through” rather than learning
- High rates of sick calls, mental health crises, or LOA (leave of absence) behind vague language
Signals during interviews:
- Residents appear exhausted or disengaged at the dinner/social
- They dodge questions about wellness, call schedules, or support
- Offhand comments like:
- “You just have to grind it out for a few years.”
- “Nobody has time to teach; you learn by doing.”
- “We don’t have complainers here. If you can’t handle it, you leave.”
Orthopedic surgery is demanding, but there is a difference between rigorous training and punitive, unsupported training. High turnover combined with a culture of fear is a strong program red flag.
How to Ask Smart Questions About Resident Turnover Without Burning Bridges
As a DO graduate, you may worry about coming across as “high maintenance” if you probe too much. You can still be strategic, tactful, and professional.

1. Ask Residents Privately, Not Only in Groups
At pre-interview dinners, post-interview socials, or breaks between sessions, find opportunities to speak with:
- A junior resident (PGY-1 or PGY-2)
- A mid-level resident (PGY-3)
- A senior resident (PGY-4 or PGY-5)
You can phrase questions like:
- “How has resident staffing been over the last few years? Any times when classes were short?”
- “In the last 5–7 years, have many residents left the program or switched specialties?”
- “If someone is struggling—clinically, academically, or personally—how does the program respond?”
Compare answers across levels. If stories conflict significantly or juniors seem unaware of recent history, that’s notable.
2. Normalize Your Curiosity
To reduce defensiveness, frame your questions in a way that shows you understand that turnover can have many causes:
- “I know all programs occasionally have residents who leave for family or personal reasons. Has that happened here recently?”
- “I’m interested in how programs support residents during difficult times. Can you share an example of how leadership responded when someone was struggling?”
This open framing allows people to share candidly without feeling attacked.
3. Specifically Ask About DO Residents
As a DO applicant to orthopedic surgery, you should absolutely ask:
- “Have there been DO residents in the program recently? How have they done?”
- “Do you feel DO and MD residents have similar opportunities for cases, research, and fellowships?”
- “Have any DO residents left the program or transferred, and if so, how was that handled?”
You’re listening for:
- Genuine, positive engagement with DOs as peers
- Concrete examples of DO graduates succeeding (e.g., “Our last DO matched into a sports fellowship.”)
- Absence of stereotypes or dismissiveness
If there were DO residents who left and the stories are vague, consistently negative, or surrounded by tension, that’s a serious warning sign.
Interpreting What You Learn and Protecting Your Career
After you’ve collected information about resident turnover, the challenge is interpreting it objectively. Not every concerning detail is a deal-breaker; not every positive interaction means the program is healthy.
1. Distinguish Between Isolated Events and Patterns
One resident leaving in 8 years:
- Ask about it, but don’t panic.
- Look for a clear, specific reason (e.g., spouse relocation, career switch with support).
Multiple residents leaving in overlapping years:
- Stronger concern.
- Especially problematic if explanations are vague, hostile, or consistently blame the residents.
Multiple classes with missing residents:
- High likelihood of substantial program problems.
2. Weigh Fit for a DO Graduate Specifically
When deciding how much resident turnover matters for you as a DO applicant, consider:
- Presence of DO faculty or alumni
Programs with DO faculty or multiple DO grads are more likely to understand your background and be committed to your success. - Historical DO success
If you hear, “Our DO graduates have done really well here—fellowships in [X, Y, Z],” that’s reassuring. - Tone around osteopathic training
Any jokes, microaggressions, or dismissive comments about DOs are a major red flag, especially if combined with resident turnover.
If multiple DOs have left or transferred out of the program in recent years, treat that as a high-stakes signal.
3. Consider the Overall Package: Volume, Culture, and Outcomes
Some programs are:
- High volume, intense, but supportive → limited turnover despite heavy workload → potentially great training
- Moderate volume, chaotic, and unsupportive → high turnover, poor outcomes → risky
- Low volume but stable and healthy → fewer cases but good teaching and excellent fellowship support → may still be strong for the right resident
Ask yourself:
- Will I be able to safely learn complex orthopedic surgery here?
- Will this environment respect and develop me as a DO surgeon?
- Will I be taken care of as a person, not just a service provider?
Matching into any orthopedic surgery program is hard as a DO—but not every ortho slot is worth taking, especially if it puts your long-term career and health at risk.
4. Use Resident Turnover as a Tiebreaker
If you’re torn between:
- Program A: Slightly less “big-name,” but stable resident classes, happy seniors, DO-friendly culture, and strong support
- Program B: Prestigious name, but multiple residents leaving, defensive leadership, unclear support for DOs
For a DO graduate, Program A is often the wiser choice. Long-term success in orthopedic surgery depends more on:
- Solid operative skills
- Good mentorship and letters
- Balanced, sustainable training
than on a shiny name attached to a troubled environment.
Frequently Asked Questions (FAQ)
1. Is any resident turnover automatically a red flag?
No. Occasional turnover is normal—people change careers, relocate for family, or face unexpected life events. Focus on patterns:
- Multiple residents leaving over a short time
- Multiple PGY classes with missing residents
- Notably vague or hostile explanations
These patterns, especially in a demanding field like orthopedic surgery, are more concerning than a single isolated case.
2. As a DO graduate, should I avoid programs that have never had a DO resident?
Not automatically, but you should be more cautious. Ask:
- “Have you had DO rotators or DO preliminary interns, and how have they done?”
- “How do you view COMLEX vs USMLE scores in screening and evaluation?”
If faculty are open, respectful, and specific about evaluating DO applicants fairly—and you don’t see other resident turnover red flags—such a program can still be a good choice. But if there’s no DO history and signs of resident turnover, that’s more worrisome.
3. How can I find out if residents have left a program if no one mentions it?
You can:
- Check the program website’s “current residents” and compare with past versions via web archives (e.g., Wayback Machine).
- Ask senior residents directly:
- “Was your class always this size?”
- “Have you had co-residents transfer out or switch specialties?”
- Ask program leadership a neutral question:
- “Has the program size changed in the last 5–10 years?”
You don’t need full names or personal details—just enough to understand whether there is a pattern of residents leaving the program.
4. If I match into a program and then discover turnover and problems, what can I do?
First, seek support within the program:
- Trusted faculty or mentors
- Chief residents
- Program leadership if appropriate
If the environment is unsafe or unsustainable:
- Talk confidentially with GME (Graduate Medical Education) or a designated ombudsperson.
- Reach out to mentors outside the program (e.g., medical school faculty, osteopathic orthopedic organizations).
- If absolutely necessary, explore options for transferring or changing specialties—but understand this is complex and should be carefully planned with mentorship.
Your priority is safety, mental health, and long-term career viability, not just enduring a toxic environment because it’s “ortho.”
Resident turnover is one of the clearest signals of the hidden reality inside a residency program. As a DO graduate pursuing orthopedic surgery, pay close attention to how many residents have left, how their departures are described, and how those gaps are affecting current trainees. A program that values transparency, supports its residents, and learns from past turnover will set you up not just to match—but to thrive as an orthopedic surgeon.






















