
Why “Malignant” Programs Matter Even More for IMGs in General Surgery
For an international medical graduate (IMG), choosing the right general surgery residency is not just about matching—it’s about surviving and thriving for 5–7 intense years. In surgery, the stakes are high: operative experience, board eligibility, visas, and your future fellowship prospects all depend heavily on the culture and quality of your program.
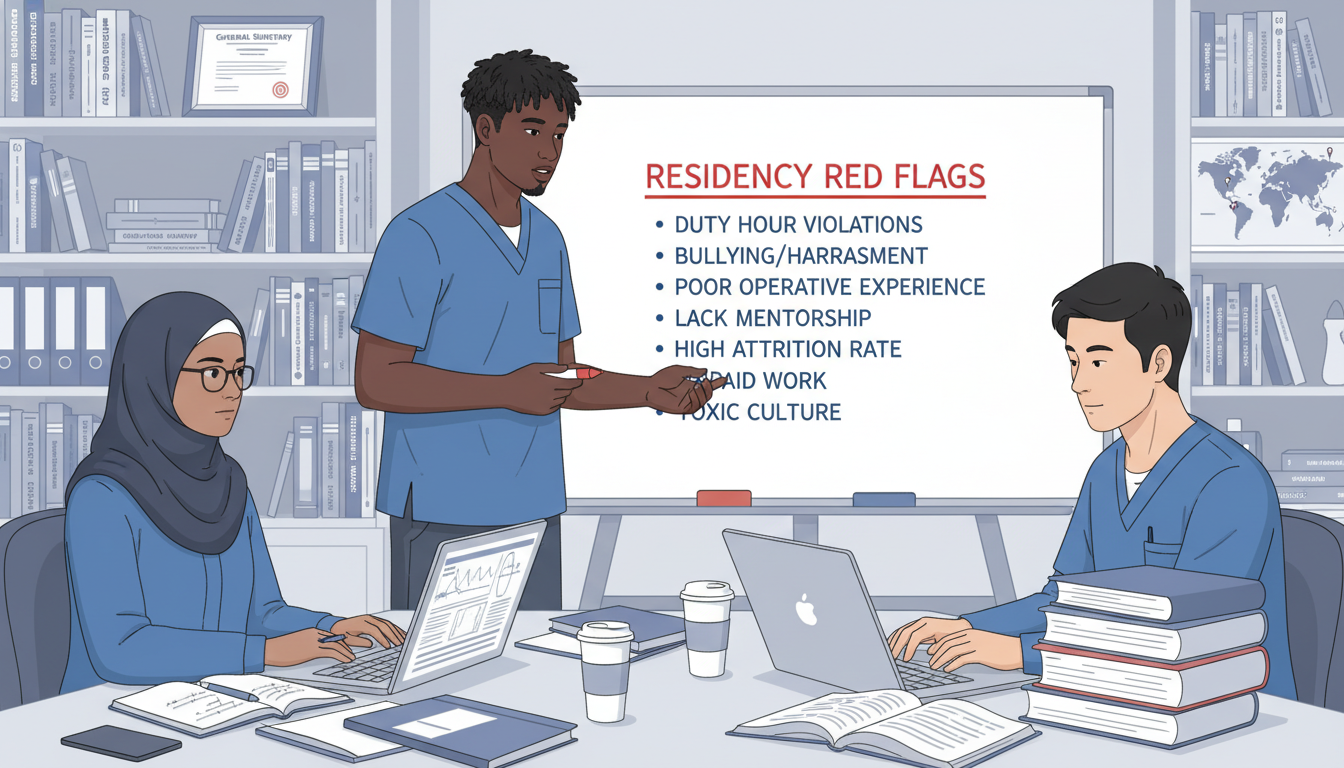
A “malignant” residency program is informally defined as one with a chronically hostile or exploitative culture: excessive workload without support, bullying, lack of educational focus, retaliation against residents who speak up, and little concern for well-being or career development. In contrast, a “benign” or “supportive” program can still be demanding, but tends to be fair, transparent, team-based, and educationally oriented.
This IMG residency guide will help you identify toxic program signs and residency red flags specifically relevant to general surgery residency and especially important for IMGs, who are often more vulnerable because of visa status, unfamiliar systems, and limited local support.
Understanding “Malignancy” in General Surgery Programs
What Makes a Surgery Residency “Malignant”?
A malignant residency program is not simply “hard” or “rigorous.” General surgery is demanding everywhere: early mornings, long cases, emergencies, and high expectations are normal. Malignancy comes from how the program handles these demands:
- Systemic disrespect or abuse
- Chronic disregard for duty hour rules and safety
- Unfair treatment, especially of IMGs or minority trainees
- Power imbalance used to intimidate, not to teach
- Institutional denial when problems are reported
Think of malignancy as a pattern of behavior and policies, not a single bad rotation or strict attending.
Why IMGs Are at Higher Risk
For an international medical graduate, certain factors amplify the risk:
Visa dependence
Loss of position can mean loss of visa, jeopardizing your ability to stay in the country. Malignant programs may use this leverage implicitly or explicitly.Limited local support network
Without family or mentors nearby, it can be harder to seek help or transfer.Less familiarity with US systems
You may not know your rights, ACGME requirements, or norms of speaking up.Bias and discrimination
Some programs may favor US graduates and treat IMGs as less capable or more “expendable.”
Recognizing residency red flags early—before the rank list—is crucial to avoiding a program that could derail your surgical career.

Core Red Flags: Culture, Education, and Workload
1. Culture of Fear, Humiliation, or Bullying
Surgery is traditionally hierarchical, but chronic humiliation is not “just how surgery is.”
Watch for:
Public shaming as routine teaching method
Attendings regularly yell, insult, or curse at residents in front of the team, nurses, or patients.Scapegoating behavior
When there’s a complication or delay, residents are always blamed, even if it’s a systems issue.Retaliation for speaking up
Residents who question unsafe practices or unfair policies later lose OR time, get poor evaluations, or have visa threats hinted.Disrespectful comments about IMGs
Jokes about accents, medical schools, or “IMGs needing to prove themselves more” are normalized.
During interviews or away rotations, observe:
- How do attendings talk to junior residents and interns?
- Do senior residents show basic respect when they’re stressed?
- If a resident makes a mistake, is the response corrective or punitive?
Example (red flag scenario):
On interview day, a faculty member “jokes” that the program is “not for weak people” and that “we ride interns hard until only the strong survive.” The residents nervously laugh but don’t contradict him. This suggests normalization of intimidation rather than supportive teaching.
2. Poor Educational Environment and Operative Experience
A malignant program often treats residents like cheap labor rather than surgeons-in-training.
Key warning signs:
Minimal structured teaching
Didactics, M&M conferences, grand rounds, simulation labs either don’t exist, often get canceled, or are poorly attended by faculty.Residents chronically stuck in scut work
Interns and juniors do mostly floor work, notes, and calls, with little involvement in actual procedures, even basic ones (central lines, chest tubes, bedside procedures).Opaque or unfair case distribution
OR experience depends on “favorites” rather than PGY level or educational needs. IMGs or “quiet” residents get fewer cases.No clear progression of responsibility
A PGY-4 resident still doesn’t feel prepared to do bread-and-butter cases independently (e.g., lap chole, hernia repair) because attendings don’t trust or teach them.
As an IMG, ask targeted questions:
- “How many major cases does a typical graduating chief log?”
- “How early do interns get to scrub and perform parts of operations?”
- “How are cases assigned—by rotation, PGY level, or something else?”
Vague or defensive answers, or chiefs who look uncomfortable answering, are strong residency red flags.
3. Excessive Workload With Systematic Duty Hour Violations
General surgery is always busy, but malignant programs normalize chronic overwork with little support.
Concerning patterns:
Frequent true 100-hour weeks
Everyone occasionally has a brutal week, but if residents say they “always work 80–100 hours” and just “fix the logs,” that’s a systemic problem.Pressure to falsify duty hours
Residents are instructed “not to log every call” or “adjust hours so ACGME doesn’t bother us.”No time for basic human needs
Residents report going 12–16 hours without eating, or having no breaks to use the restroom on most days.Inadequate backup coverage
When someone is sick or on leave, the team simply “absorbs it” without adjustment.
On interview day, be specific:
- “How often do you feel you are near or above 80 hours per week?”
- “Does the program respond constructively if residents report duty hour concerns—can you give an example?”
If answers include, “We just do what needs to get done; surgery is not for complainers,” you are hearing malignant thinking.
IMG-Specific Malignancy Traps: Visa, Evaluations, and Discrimination
4. Visa and Contract Vulnerabilities
For many IMGs, visa status is the single biggest vulnerability.
Critical questions:
Which visas are sponsored?
Does the program support J-1 only, or both J-1 and H-1B?
Are there hidden preferences (e.g., “We’ll rank J-1s, but H-1Bs are rare”)?What happens if performance concerns arise?
Has the program ever non-renewed an IMG’s contract? How did they handle visa transition or assistance?Transparency about contract renewal
Is renewal essentially automatic if you are meeting expectations, or are residents re-interviewed yearly?
Residency red flags:
- No clear answers about visa processes, or PD “doesn’t know the details.”
- History of sudden non-renewals or dismissals of IMGs with vague explanations (“not a good fit” without due process).
- Residents hint that “you need to be careful; if they don’t like you, it can get bad fast,” especially directed at IMGs.
5. Unfair Evaluation, Remediation, and Promotion Practices
In malignant programs, formal evaluations may be weaponized rather than used to foster growth.
Watch for:
Subjective, personality-based evaluations
Phrases like “not a culture fit,” “too quiet,” or “too assertive” used more often for IMGs or women.Unequal standards
US graduates excused for similar mistakes that get IMGs put on remediation.Opaque remediation processes
Residents don’t understand what remediation entails, how long it lasts, or what success looks like.Threat-based feedback
Feedback sessions focus on “if this happens again, we will not renew your contract” rather than clear coaching.
When speaking to residents:
- “Have any residents needed remediation in the past few years? How was it handled?”
- “Do you feel evaluations fairly reflect performance, or do certain residents seem targeted?”
If residents say, “You just don’t want to get on the wrong side of certain attendings,” consider that a major toxic program sign.
6. Microaggressions and Overt Bias Against IMGs
Subtle discrimination can be as damaging as open hostility.
Examples:
Constantly questioning your training background
“Do they even do surgery in your country?” said as a “joke” more than once.Excluding IMGs from informal opportunities
Social events, research projects, or special OR days are regularly shared in informal networks that IMGs are not part of.Diminished expectations
IMGs get assigned simpler cases or fewer independent responsibilities even when performance is strong.Blaming language barriers for every issue
Communication problems automatically attributed to “accent” or “culture” without looking at systems.
Ask yourself during the interview day and social:
- Do residents with foreign accents speak during conferences, or do they appear hesitant and shut down?
- Are IMGs represented among chief residents, academic leaders, or recent fellowship matches?
If IMGs are mostly clustered in early years and “disappear” later (transfers, non-renewals), this is a serious warning.
How to Detect Malignant Programs Before You Rank
7. Reading Between the Lines on Websites and Program Materials
Even before interviewing, you can often spot patterns:
High resident turnover
“Recent graduates” page shows many residents who “transferred” or “left for personal reasons,” especially mid-program.Missing or vague operative case data
No mention of case numbers, or “we exceed ACGME minimums” without specifics.Very few IMGs in current or past classes
If you’re the only IMG in the list of residents in a historically US-IMG mixed market, consider why.No mention of well-being or support resources
Most modern programs highlight wellness efforts; an absence may indicate low priority.
Use this initial screen to decide how cautiously to approach the program and what questions to ask.
8. Using Interviews and Pre-/Post-Interview Communications Strategically
Interviews are your best chance to probe residency red flags directly, especially around malignant residency programs in surgery.
Ask residents (ideally without faculty around):
- “If you could change one thing about this program, what would it be?”
- “How does the program respond when residents are overwhelmed or burning out?”
- “Have any residents left the program in the last 3–5 years? Why?”
- “Do you feel safe raising concerns to the PD or GME office?”
Listen for:
Hesitation or forced positivity
If a resident takes a long pause and says, “We’re a very strong, rigorous program,” but never uses the words “supportive,” “fair,” or “teaching,” that’s informative.Lack of alignment between junior and senior residents
Interns say everything is great; chiefs look fatigued or guarded. Chiefs often have the clearest long-term view.
With faculty and the program director:
- “What are three things you’re working to improve in the program now?”
- “How do you support residents who are struggling academically or personally?”
- “How is feedback from residents incorporated into program changes?”
A healthy program can openly discuss weaknesses and improvement efforts. A malignant one becomes defensive or blames “lazy residents” or “ACGME rules.”
9. Interpreting Resident Body Language and Interactions
What you see can matter more than what you hear:
- Do residents laugh and talk with each other, or do they seem isolated and tense?
- Do they speak respectfully about nurses, APPs, and other services—or is there constant conflict?
- At the pre-interview dinner, do they freely discuss challenges, or are they careful and guarded?
Practical tip:
Right after each interview, write down your impressions while they’re fresh:
- “How did residents talk about call?”
- “Did anyone mention retaliation or fear?”
- “Would I trust this group to have my back at 3 a.m. in a trauma case?”
These notes will be invaluable during your surgery residency match ranking decisions.
10. Cross-Checking Reputation and Anonymous Feedback
Use multiple sources:
Current and recent alumni
Ask to speak with a graduating or recent chief (not just the ones selected by the program). Find alumni via LinkedIn or hospital websites.Online forums
Platforms like Reddit, SDN, specialty Discords, or country-specific IMG networks can reveal patterns. Don’t take a single comment as truth—look for repeated themes.Fellowship and job placement
Malignant programs with poor training often have weaker fellowship matches or graduates who struggle to secure good jobs.
When reading online reports of a malignant residency program, ask:
- Are complaints consistent across years and posters?
- Are issues specifically about abuse, retaliation, or poor training, not just “hard work” or “lots of trauma” (which may be educational positives)?
If multiple independent sources mention toxic program signs like bullying, falsified duty hours, or discrimination against IMGs, treat that very seriously.
Navigating the Match: Balancing Risk, Training Quality, and Visa Needs
11. Distinguishing Tough but Supportive vs. Truly Toxic
Not all strict or busy surgery programs are malignant. In fact, some of the best training environments are intense but fair.
Features of a tough but supportive general surgery residency:
- Clear expectations; attendings are demanding but teach.
- Residents are tired but proud, not fearful.
- Chiefs feel prepared for independent practice or fellowship.
- When something goes wrong, the program debriefs and improves systems, not just blames individuals.
Features of a truly toxic program:
- Residents are anxious, fearful, or planning exit strategies.
- IMGs worry about being targeted if they struggle.
- Problems repeat year after year; leadership minimizes concerns.
- Complaint channels exist on paper but are ignored or punished in practice.
When ranking programs, remember:
It is better to train at a slightly less “prestigious” but supportive program than a malignant one with a big-name hospital. Your skills, confidence, and references will ultimately matter more than the brand name.
12. Risk Management for IMGs: Practical Strategies
As an IMG in the surgery residency match, you may feel pressure to rank any program that offers a spot. Try to balance opportunity with safety:
Create tiers of safety
- Green: supportive culture, decent operative exposure, IMG-friendly track record.
- Yellow: some concerns (workload, limited IMGs), but residents seem functional and not fearful.
- Red: multiple serious residency red flags or repeated reports of malignancy.
Avoid ranking programs with major red flags above ones that are clearly safer, even if the malignant program seems more “prestigious.”
Have a back-up specialty or pathway if you feel forced to choose between only malignant options (e.g., prelim surgery plus later re-application, or another specialty you can accept).
Know your rights
Familiarize yourself with:- ACGME duty hour rules
- Anti-discrimination policies
- Internal grievance processes at teaching hospitals
Being informed reduces vulnerability, even in a challenging environment.
Frequently Asked Questions (FAQ)
1. How can I tell if a general surgery residency program is truly “malignant” or just very busy?
Look beyond workload to how the program responds to stress. Busy but healthy programs:
- Enforce duty hour rules as much as possible.
- Encourage residents to speak up when overwhelmed.
- Handle complications and errors with structured review, not humiliation.
- Have chiefs who feel prepared for independent practice and still recommend the program.
Malignant programs:
- Normalize chronic overwork and under-report hours.
- Retaliate against residents who raise concerns.
- Use fear and shame as primary teaching tools.
- Show patterns of resident transfer, dismissal, or non-renewal.
If multiple independent sources (residents, alumni, online forums) describe fear, bullying, or retaliation, treat the program as malignant regardless of case volume or prestige.
2. Are malignant programs more common in surgery than in other specialties?
Surgery has historically had a more hierarchical and intense culture, which can create fertile ground for toxic program signs. However, many modern surgery programs are actively reforming culture, focusing on education, safety, and well-being. Malignant programs are not the rule, but they still exist, particularly where leadership dismisses concerns as “residents being soft” or “this is how surgery has always been.”
3. As an IMG, should I still consider a program if it seems a bit malignant but offers H-1B sponsorship?
Visa sponsorship is critically important, but your professional survival matters too. A program that threatens your mental health, licenses, or reputation can harm you more than a missed match year. If a program clearly shows multiple residency red flags (bullying, discrimination, unsafe duty hours, unfair treatment of IMGs), think very carefully before ranking it—especially above safer options that may offer J-1 only. Whenever possible, prioritize reasonable safety and training quality alongside visa considerations.
4. What should I do if I realize my matched program is malignant after I start?
If you find yourself in a clearly malignant residency program:
Document everything
Keep a confidential record of incidents: dates, people involved, emails, and messages. This is critical if you need to escalate or transfer.Identify allies
Look for supportive faculty, chief residents, or GME staff who are willing to listen.Use formal channels when necessary
- Program leadership (PD, associate PD)
- Designated institutional official (DIO) / GME office
- Ombudsperson, wellness office, or HR where available
Explore transfer or alternative pathways
Quietly research openings in other general surgery programs, prelim-to-categorical transitions, or switches to related specialties. Talk to trusted mentors outside your institution.Prioritize safety
If psychological or physical safety is at risk, seek immediate mental health support and escalate appropriately. No residency position is worth your health or life.
By understanding and recognizing malignant residency program patterns—especially those that disproportionately affect the international medical graduate in general surgery residency—you can make more informed choices in the surgery residency match. Demanding training is expected; disrespect, danger, and exploitation are not.






















