
Choosing the right medical genetics residency is critical for your career, wellbeing, and visa status—especially as an international medical graduate (IMG). A strong program can launch you into a sustainable, fulfilling career; a malignant residency program can drain your mental health, put your immigration status at risk, and limit your future opportunities.
This IMG residency guide focuses on identifying malignant programs in medical genetics, with practical tools you can apply before ranking programs and during interview season. While examples are genetics-specific, the core concepts apply across specialties.
Understanding “Malignant” vs. “Demanding” Programs
Not every tough or high-expectation program is malignant. Medical genetics is naturally complex and intellectually demanding. The danger is when systemic toxicity replaces high standards plus support.
What is a “malignant residency program”?
A malignant program is one where patterns of behavior and culture repeatedly:
- Disrespect or exploit residents
- Violate duty hours or basic safety
- Tolerate bullying, harassment, or discrimination
- Undermine education in favor of cheap labor
- Retaliate against those who speak up
- Create a climate of fear, burnout, or mental health crises
In the context of medical genetics, this might look like:
- Being left alone to manage complex genetic consults without appropriate supervision
- Unrealistic expectations for research productivity without protected time
- No support for developing counseling skills, yet residents are still expected to manage emotionally heavy conversations with families
Demanding but healthy vs. malignant
Demanding but healthy program:
- High expectations, but:
- Faculty are approachable and provide feedback
- Workload is heavy at times, but duty hours are generally respected
- Residents feel tired, but also growing and supported
- Concerns can be raised without fear
Malignant program:
- High expectations plus:
- Chronic understaffing and unsafe patient loads
- Public shaming, intimidation, or punitive responses
- Gaslighting about workload or wellness (“You just need to toughen up”)
- Systematic neglect of education and supervision
For IMGs, malignant features are magnified: visa vulnerability, lack of local support networks, and unfamiliarity with U.S. or Canadian training norms make a toxic environment far more dangerous.
Unique Vulnerabilities of IMGs in Medical Genetics
Before identifying residency red flags, you need to understand why IMGs are especially at risk.
1. Visa dependence and power imbalance
As an international medical graduate, your:
- Visa sponsorship (J-1, H-1B, etc.)
- Income
- Path to board eligibility and future employment
all depend on staying in good standing in your residency. Malignant programs may exploit this:
- Threatening non-renewal of contracts if residents “complain”
- Pressuring IMGs to work beyond duty hours or take extra call
- Discouraging reporting of harassment or discrimination
In a field like medical genetics, where programs are fewer and more concentrated, transferring out may be harder, increasing your vulnerability.
2. Smaller specialty, fewer options
Medical genetics is a relatively small specialty with:
- Limited number of ACGME-accredited programs
- Highly variable structures (combined pediatrics-genetics, internal medicine-genetics, categorical genetics after other residencies, etc.)
This can make it harder to simply “switch programs” if your training environment becomes toxic. Some malignant programs rely on that reality.
3. Lack of local networks
U.S. or Canadian graduates often have:
- Alumni networks
- Faculty advocates
- Classmates at other institutions who can share intel about programs
IMGs may not. That’s why a structured approach to screening programs—using public data, resident contacts, and careful questioning—is essential.
Core Residency Red Flags: How Malignancy Shows Up
Below is a targeted framework for spotting toxic program signs, including specific examples relevant to the genetics match and IMGs.
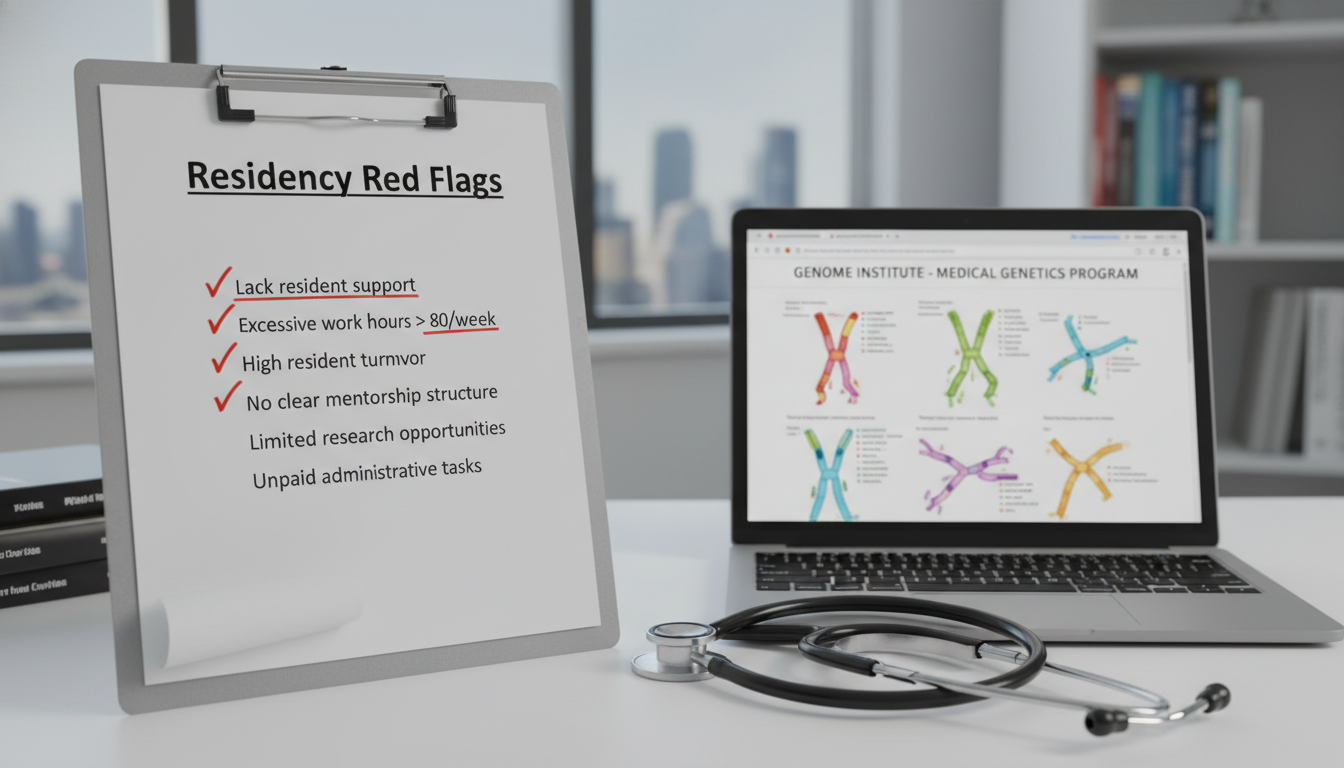
1. Resident turnover, attrition, and silence
Red flags:
- Multiple residents have left, transferred, or did not renew contracts in recent years
- Former residents are unreachable or only give vague, defensive answers
- No current residents available to speak with you, or conversations are tightly controlled by leadership
In medical genetics (often small cohorts):
- Losing even one resident out of a class of 2–3 is a major signal
- Ask specifically if any residents have left the program and why
Questions to ask:
- “How many residents have left the program in the last 5 years?”
- “Have any residents needed to repeat a year, and what were the main reasons?”
- “Could I speak with a few recent graduates, including at least one IMG if possible?”
If they deflect, minimize, or become defensive, treat that as a significant concern.
2. Culture of fear, disrespect, or bullying
Toxic program signs:
- Residents describe faculty as “unapproachable,” “angry,” or “vindictive”
- Public shaming during conferences or feedback (especially in front of families on genetics consults)
- Repeated stories about yelling, humiliation, or intimidation
- Gaslighting behavior: “You’re too sensitive,” “That’s just how training is”
In genetics specifically:
- Insensitive handling of complex cases (e.g., fetal anomalies, new cancer predisposition diagnoses) with no emotional support for the resident
- Faculty mocking residents for not immediately recalling obscure variant classifications
- Genetic counselors or other team members undermining residents rather than teaching
Questions to ask:
- “How does the program handle mistakes made by residents?”
- “Can you describe how feedback is typically given—publicly or one-on-one?”
- “Has anyone ever felt uncomfortable with how they were spoken to or treated? How was that handled?”
Look for consistent patterns rather than one isolated incident.
3. Duty hours and workload violations
Classic residency red flags:
- Chronic violation of ACGME duty-hour rules
- Pressure to underreport hours or skip logging them
- “Pre-charting” or “stay-late-to-finish” culture, especially unpaid and unacknowledged
- No genuine post-call protection
Genetics often has:
- Variable consult volume, sometimes manageable—but beware when:
- You’re covering multiple hospitals with no backup
- Residents are expected to pick up extra non-genetics call regularly (e.g., pediatrics or internal medicine) with no schedule relief
Questions to ask:
- “How often are residents staying 2+ hours beyond scheduled sign-out?”
- “Have residents ever been told to adjust or 'correct' their logged duty hours?”
- “What happens when inpatient consult volume spikes or multiple complex cases come in at once?”
If residents say things like:
- “We just make it work”
- “We don’t really log those hours”
- “You get used to being here late every night”
assume there is a normalization of unhealthy expectations.
4. Poor supervision and unsafe autonomy
In medical genetics, adequate supervision is non-negotiable:
- Complex variant interpretation
- Counseling on reproductive risk, cancer predisposition syndromes, or untreatable conditions
- Prenatal counseling and coordination with multiple specialties
Malignant patterns:
- Residents sent to see consults alone with minimal or delayed attending input
- Attendings signing notes without truly reviewing or discussing cases
- Pressure to make counseling decisions outside your comfort or training level
- Fellows or senior residents acting as primary supervisors with no attending involvement
Questions to ask:
- “Are attendings consistently available for difficult counseling conversations with families?”
- “On a busy consult day, how often do you feel truly unsupervised?”
- “What is the process when you’re unsure about a genetic test or interpretation?”
If residents say they “learn by trial and error” in high-stakes genetic counseling situations, consider that a safety and ethics alarm.
5. Education vs. service: Is this a training program or cheap labor?
Signs of a malignant residency program that prioritizes cheap labor:
- Repeated cancellation of didactics, journal clubs, or case conferences for service needs
- You are always covering other services (e.g., NICU, PICU, adult medicine) for workforce gaps, at the expense of genetics exposure
- Genetics clinics are overbooked to the point that you cannot prepare or debrief
Medical genetics should offer:
- Structured teaching on variant interpretation, inheritance patterns, counseling techniques
- Exposure to different clinics (metabolic, cancer, prenatal, dysmorphology, adult genetics, etc.)
- Interactions with genetic counselors and laboratory genetics staff
Questions to ask:
- “How often are teaching sessions canceled for service?”
- “What percentage of your time is truly genetics-focused vs. covering other services?”
- “Do you feel your education in genetics is prioritized over filling service gaps?”
Repeated responses like “It depends on staffing; we often have to cover other units instead of genetics clinic” should raise alarms.
6. Lack of support for IMGs: visas, licensing, and adaptation
For an international medical graduate, a safe program must be proactive in supporting:
- Visa processing (J-1, H-1B, renewals, travel letters)
- State licensing and USMLE or other exam timelines
- Cultural adaptation and communication skills
Red flags:
- Vague or unclear answers about visa sponsorship and renewal years
- No one in GME or the program is specifically knowledgeable about IMG issues
- IMGs report feeling isolated, or “on their own” for navigating bureaucracy
- Past IMGs struggling to graduate on time due to administrative delays or lack of advocacy
Questions to ask:
- “How many current or recent residents were IMGs?”
- “Who specifically helps with visa and licensing documentation?”
- “Has any resident ever had visa issues that impacted their ability to continue training?”
If the program has never had an IMG but is suddenly open to you, probe carefully. The absence of IMG experience isn’t automatically malignant, but it demands more cautious questioning.
Program-Specific Red Flags in Medical Genetics
Beyond general residency red flags, there are issues unique to medical genetics that can signal malignancy or at least a poor training environment.

1. Limited exposure across the genetics spectrum
A robust medical genetics residency should provide:
- Pediatric and adult genetics
- Cancer genetics
- Metabolic/genetic biochemical disorders
- Prenatal genetics
- Dysmorphology/teratology
- Genomic technologies and variant interpretation
Red flags:
- Training dominated by only one niche, e.g., almost exclusively pediatrics or metabolic, with minimal exposure to others
- Minimal or no cancer genetics, despite being advertised
- No structured exposure to genetic counseling practices
Ask residents:
- “Can you walk me through what a typical year’s rotations look like?”
- “Do you feel prepared to practice broad-based medical genetics after graduation, or only one area?”
- “Are there clinics or subspecialties advertised on the website that you actually rarely see?”
If the training seems narrow and service-heavy, it may not be malignant in the abusive sense, but it’s a career-limiting red flag.
2. No clear laboratory and genomics training
Modern medical genetics is deeply integrated with:
- Next-generation sequencing
- CNV and structural variant analysis
- Variant interpretation frameworks (ACMG/AMP guidelines)
- Interaction with molecular pathology and cytogenetics
A concerning program:
- Offers little to no structured lab exposure
- Does not collaborate meaningfully with molecular genetics labs
- Leaves residents to figure out lab reports independently
Ask:
- “How is laboratory and genomics training structured?”
- “Do residents routinely interact with lab directors or molecular geneticists?”
- “Are there dedicated rotations in cytogenetics, molecular genetics, or biochemical genetics labs?”
A malignant pattern is where you are still expected to confidently interpret complex reports without sufficient training.
3. Minimal interaction with genetic counselors
An excellent genetics residency fosters a team-based approach with genetic counselors (GCs). Red flags include:
- GCs and residents working in silos without collaboration
- Tension or distrust between GCs and physicians
- No opportunity to learn counseling styles, session structure, or documentation approaches from GCs
Ask:
- “How do residents and genetic counselors collaborate in clinics and inpatient consults?”
- “Are there opportunities to observe and co-lead counseling sessions with GCs?”
- “Do GCs participate in teaching or case conferences?”
If the environment seems territorial or non-collaborative, you may be entering a dysfunctional culture.
4. Poor graduate outcomes: boards, jobs, and fellowships
Look closely at outcomes:
- Board exam pass rates in clinical genetics (and any combined specialty)
- Placement in fellowships, academic positions, or reputable clinical roles
- Performance of IMGs specifically (if data available)
Red flags:
- Multiple residents failing boards, especially without clear remediation or support
- Graduates working in roles far below expected level or outside genetics by necessity, not choice
- Vague answers such as “Most people do fine after graduation” with no specifics
Ask:
- “What is your 5-year board pass rate in medical genetics?”
- “Where have recent graduates gone—especially IMGs? Could I speak with one or two?”
- “How does the program support residents preparing for boards?”
If they cannot provide concrete examples of successful graduates, reconsider.
How to Investigate Programs: A Stepwise IMG Strategy
Knowing the signs is only half the work. You need a strategy for gathering reliable data without burning bridges or jeopardizing your candidacy.
Step 1: Pre-interview research
Use:
- FREIDA, program websites, NRMP data, and review sites (with caution)
- Social media (Twitter/X, LinkedIn) where some residents and faculty are active
- PubMed and institutional pages to see faculty stability and scholarship
Look for:
- Sudden disappearance of multiple faculty or leaders
- Gaps in program directors’ tenure (frequent changes can signal deeper problems)
- Missing or outdated information about residents
Step 2: During interviews: read verbal and non-verbal cues
You will typically meet:
- Program leadership
- Faculty
- Current residents (sometimes fellows and GCs)
Pay attention to:
- Are residents ever alone with you without faculty on screen or in the room?
- Do they visibly hesitate before answering sensitive questions?
- Do multiple residents independently provide similar, reassuring details—or do answers feel rehearsed?
Useful open-ended questions:
- “What would you change about this program if you could?”
- “When people struggle (personally or academically), what happens?”
- “What kind of resident tends to be unhappy here and why?”
Malignant programs often cannot describe healthy, supportive responses to struggle.
Step 3: Post-interview, reach out to additional contacts
After interviews:
- Ask the coordinator or chief residents if you can contact recent graduates, ideally including IMGs
- Use LinkedIn or professional email to reach alumni (politely and briefly)
Example outreach:
“I’m an IMG applying to your former program in medical genetics and would love to hear about your experience—especially as an international graduate. Even 10–15 minutes would be very helpful. I’m particularly interested in the culture, supervision, and support for visas and boards.”
Former residents, especially those now at different institutions, may be more candid.
Step 4: Weighing red flags vs. green flags
No program is perfect. You must balance:
- Severity of the red flag
- Whether it affects personal safety, immigration, or educational integrity
- Your alternative options in the genetics match
Examples of non-negotiable red flags for IMGs:
- Pressure to falsify duty hours
- History of visa or contract threats against IMGs
- Tolerance of overt bullying or discrimination
- Consistent under-supervision with safety implications
Concerns like “not much cancer genetics exposure” or “we wish there were more research” may be acceptable if the core culture is healthy and supportive.
Frequently Asked Questions (FAQ)
1. As an IMG, should I avoid a program that has never trained an international graduate?
Not automatically. But you should:
- Ask detailed questions about visa sponsorship, prior experience with J-1 or H-1B, and who handles paperwork.
- Clarify whether the institution sponsors H-1B at all (many only support J-1).
- Seek evidence that GME has a solid infrastructure for international trainees (e.g., other specialties with IMGs).
If leadership seems uncertain, indifferent, or dismissive about visas, that’s a serious concern.
2. How can I tell if residents are being honest with me?
No method is perfect, but you can:
- Ask the same question in different ways to different residents and see if answers align.
- Request to speak with residents one-on-one or in a setting without faculty present.
- Look for non-verbal cues: hesitation, glances at faculty, nervous laughter when you ask about workload or culture.
- Compare what residents say with what the program advertises on the website and in presentations.
If everything sounds unrealistically perfect and no one can name a single weakness, that itself is a red flag.
3. Are all small or lower-profile genetics programs risky for IMGs?
No. Some of the most supportive, non-malignant programs are smaller or less famous. Consider:
- Do residents feel known and supported as individuals?
- Is there strong, accessible leadership and mentorship?
- Are educational goals clear and consistently pursued?
A smaller program can be an excellent choice, especially for an IMG, if it has a healthy culture, stable leadership, and a track record of advocating for trainees.
4. I suspect a program is malignant, but it’s my only likely option. What should I do?
This is a difficult position, particularly in a small specialty like medical genetics. Consider:
- Whether the red flags are about culture and safety (abuse, harassment, visa threats) versus limitations in exposure (less research, narrower clinic variety).
- Your long-term goals: Would another route (e.g., internal medicine or pediatrics first, then genetics fellowship later) offer a safer path?
- Whether you can create a support network outside the program—mentors at other institutions, IMG advocacy groups, mental health support.
If the program appears truly malignant, especially regarding visa safety and abuse, it may be better to reapply in a future cycle than to risk burnout, derailment, or immigration problems.
Choosing a medical genetics residency as an international medical graduate requires more than good scores and strong letters—it demands active, skeptical evaluation of program culture. By systematically looking for residency red flags, asking direct questions, and prioritizing your safety and growth, you can reduce your risk of landing in a malignant residency program and instead find a training environment that respects both your potential and your humanity.






















