
Understanding “Malignant” Transitional Year Programs as an IMG
For many international medical graduates (IMGs), the transitional year (TY) is a critical stepping stone toward advanced specialties such as radiology, anesthesiology, dermatology, PM&R, neurology, or ophthalmology. A well-run TY program can be a supportive, balanced year that builds your clinical skills and prepares you for the next step. A malignant residency program, on the other hand, can leave you burned out, under-supported, and at risk of delays or failures in your training.
This IMG residency guide focuses specifically on how to identify malignant programs and toxic program signs in transitional year residency. Because IMGs may have less in-person exposure to U.S. training environments, recognizing residency red flags early—before you submit your rank list—is essential to protect your education, mental health, and long-term career.
In this article, we will cover:
- What “malignant” means in the context of residency
- Why IMGs in transitional year programs are uniquely vulnerable
- Concrete red flags to watch for during your research, interviews, and post-interview communications
- How to evaluate program culture, wellness, and educational value from a distance
- Practical steps if you suspect a program is toxic
What Does “Malignant” Mean in a Transitional Year Residency?
In everyday residency language, “malignant” describes a residency program with a systematically harmful culture—one that prioritizes service over education, tolerates or promotes mistreatment, and disregards resident well-being. While any specialty can have malignant programs, transitional year residencies can be especially variable: some are outstanding and cushioned; others are essentially “cheap labor” with minimal learning.
Core Features of a Malignant Program
A malignant transitional year residency program often shows several of the following features:
- Chronic Disrespect or Abuse: Yelling, public humiliation, shaming for questions, or ridicule of residents.
- Excessive Service With Minimal Education: Residents mainly “doing scut” (discharges, notes, paperwork) with minimal teaching, bedside learning, or feedback.
- Punitive Environment: Retaliation or threats for reporting concerns, speaking up, or requesting help.
- Ignored Duty Hours: Systematic underreporting of hours, pressure to falsify logs, and normalization of 80+ hour weeks.
- Lack of Support: Poor supervision, unsafe patient loads, or being “thrown in” without guidance.
- Fear-Based Culture: Residents are constantly afraid of “getting in trouble,” not matching into advanced positions, or having visas jeopardized.
Why It Matters Even for “Just One Year”
Some IMGs may be tempted to think: “It’s only 12 months; I can survive anything.” That perspective is risky:
- Burnout in this year can affect performance in Step 3 exams, applications for advanced residency spots, or your ability to network.
- Bad reputations travel. Program leadership in advanced specialties may know which TY programs are malignant.
- High stress increases risk of medical errors and jeopardizes patient safety—and your license.
- Visa-dependent IMGs face higher stakes if issues arise regarding performance or contract renewal.
Choosing a healthy TY program is not a luxury; it’s a critical strategic decision.
Unique Vulnerabilities of IMGs in Transitional Year Programs
As an international medical graduate, you bring valuable skills and perspectives, but you may also face structural vulnerabilities that malignant programs exploit, intentionally or not.
Visa and Contract Dependence
Many IMGs in a transitional year residency depend on:
- J‑1 or H‑1B visas tied to a single institution
- Future offers from advanced PGY‑2 or PGY‑3 positions
This can make it harder to speak up about toxic program signs or to exit a bad environment. Malignant programs may implicitly leverage this:
- Suggesting that “complainers” risk poor evaluations
- Hinting that “we can always find another IMG”
- Using your dependence to push extra shifts or unpaid work
A healthy program will:
- Be transparent about visa support and policies
- Encourage you to raise concerns without fear
- Emphasize that resident well-being is a shared responsibility
Power Imbalance and Cultural Barriers
IMGs may be less familiar with:
- U.S. norms around duty hours, mental health supports, and reporting mechanisms
- Institutional resources (GME office, ombudsman, ACGME complaint process)
- Subtle cultural cues (sarcasm, “joking” about abuse, or coded language)
Malignant environments sometimes hide behind cultural excuses:
- “We are just straightforward here; don’t be sensitive.”
- “In my day we worked 120 hours a week and survived.”
- “This is how we create strong doctors.”
You should not need to accept harassment or unsafe workloads to be considered “strong.” A good TY program helps IMGs adjust, not break.
Information Gaps When Applying from Abroad
IMGs usually:
- Have fewer chances to do U.S. clinical rotations at target programs
- May not have upperclassmen or alumni to provide direct, honest feedback
- Rely more heavily on websites, interview impressions, and official statements
This makes it easier for malignant programs to appear polished on paper while hiding deep cultural problems. Therefore, learning how to interpret indirect clues and residency red flags is especially important.
Clear Red Flags: Toxic Program Signs You Can Spot Early
When evaluating transitional year residencies, particularly as an IMG, look for these warning signs at each phase: before applying, during interviews, and after interviews.
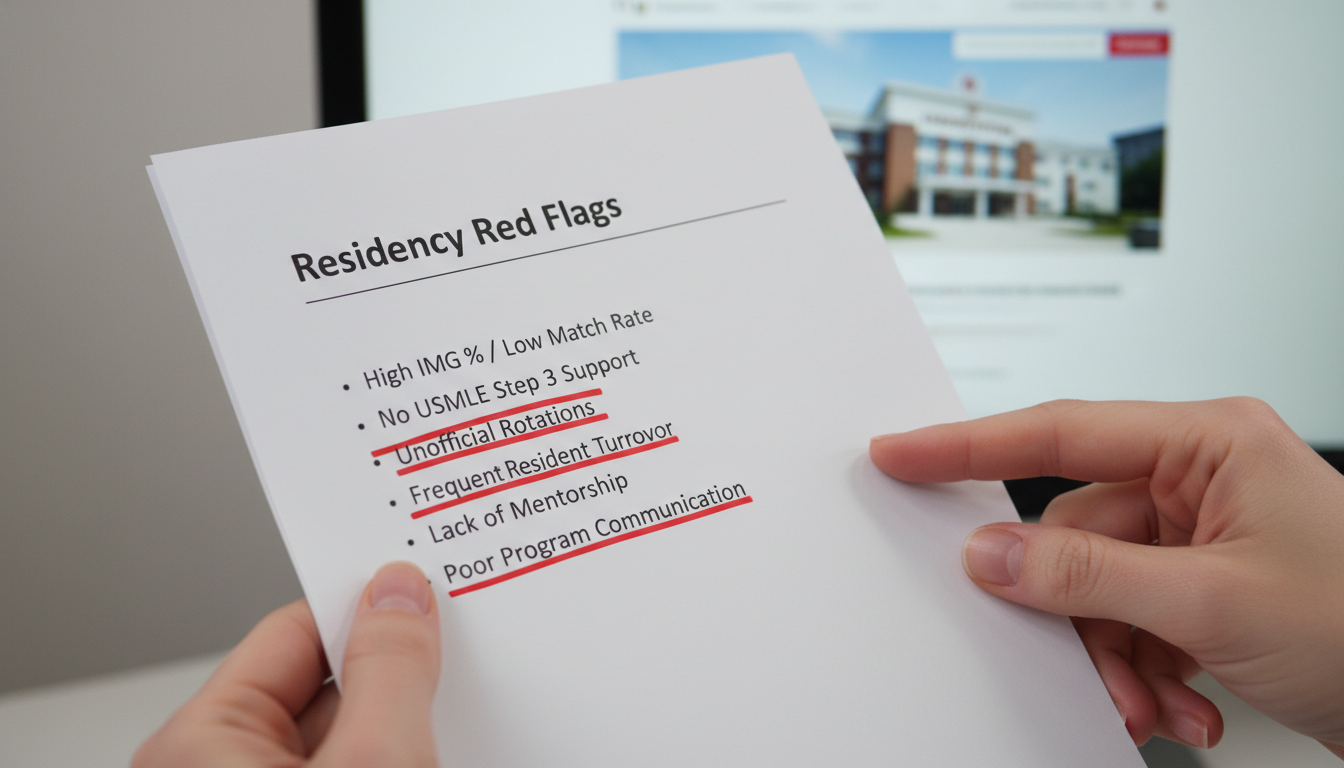
A. Red Flags in Program Websites, Public Data, and Reputation
Unusually High Attrition or Replacements
Ask or research:- Are there frequent mid-year replacements or “late positions” posted for the TY program?
- Is there a pattern of residents not completing the year or “moving on for personal reasons”?
High unexplained turnover is a classic malignant sign.
No Mention of Wellness or Resident Support
Most programs highlight wellness now. If a site:
- Never mentions mental health support, counseling, or wellness activities
- Has no description of mentoring or advising
- Barely describes educational structures (didactics, conferences)
…it may suggest a service-heavy, resident-unfriendly culture.
- Opaque Call Schedules and Workload Descriptions
A normal program can roughly explain:
- Typical weekly schedule
- Call frequency (e.g., q4, night float system)
- Average patient load and admitting caps
If information about call is vague (“we are busy, but you learn a lot”) or completely absent, treat that as a red flag.
- Poor Board Pass Rates or Inconsistent Outcomes
Some transitional year residents still sit for the USMLE Step 3 or other exams. Red flags include:
- Repeated failures of residents without clear remediation systems
- Lack of data about alumni outcomes (advanced matches, fellowships)
If a TY program cannot show you where graduates go, it may not prioritize your future.
- Negative Word-of-Mouth in Online Communities
Look for patterns in:
- Reddit (r/medicalschool, r/Residency)
- Specialty-specific forums (for radiology, anesthesia, derm, etc.)
- Word of mouth from recent graduates or fellows
One angry post alone is not proof. But repeated, specific complaints about bullying, extreme hours, visa threats, or retaliation are major residency red flags.
B. Red Flags During Interview Day
Interview day is your best chance to assess culture. Ask about challenges directly and listen carefully to what is said—and what is not.
- Residents Seem Exhausted, Guarded, or Afraid to Speak
Ask residents:
- “How many hours do you realistically work per week?”
- “What is the hardest part about training here?”
- “If you could change one thing, what would it be?”
Red flags:
- Long pauses, nervous glances to faculty, vague answers like “we’re busy, but it’s ok.”
- Residents contradicting each other about duty hours or call.
- A resident emphasizing, “We survive” rather than “We learn” or “We feel supported.”
- Faculty or Leadership Dismisses Wellness Concerns
Notice how leadership responds if you ask:
- “How do you handle resident fatigue or burnout?”
- “What happens if someone is struggling clinically or personally?”
Red flags:
- Jokes about “weak” residents or “snowflakes.”
- Comments like “we don’t really have those problems here” (which suggests denial).
- Blaming residents exclusively when there are performance issues.
- Inappropriate Comments About IMGs
As an international medical graduate, be very alert to:
- Jokes implying IMGs are “cheap labor.”
- Comments like “we rely on IMGs because they work harder and complain less.”
- Program leadership implying that visa concerns are a tool to ensure compliance.
These are strong indicators of a malignant residency program culture where IMGs may be exploited.
- Over-Emphasis on Service Volume vs Education
When you ask about teaching, you should hear about:
- Structured didactics, morning reports, noon conferences
- Protected time for teaching or academics
- Faculty engagement and mentorship
Warning signs:
- The program is proud mostly of being “the busiest” hospital.
- Program leaders repeatedly stress “you will see everything,” but provide no details about how they support that learning.
- Residents report regularly missing conferences due to workload.
- No Private Time with Residents
A healthy program:
- Gives you protected, faculty-free time with current residents.
- Encourages you to ask candid questions.
If your only contact with residents is closely supervised, scripted, or limited, it may signal the program is worried about what residents might reveal.
C. Red Flags After Interview Day
Even after the visit, you can detect toxic program signs through follow-up communications.
- Pressure Tactics About Ranking
Unethical patterns include:
- Strong hints that “you should rank us highly, or you might not match.”
- Email or phone contact that feels coercive rather than supportive.
- Implied promises of ranking you highly in exchange for verbal commitments.
This behavior reflects poor professionalism and may correlate with other malignant traits.
- Inconsistent or Defensive Answers to Follow-Up Questions
If you email follow-up questions about:
- Call structure
- Moonlighting
- Remediation and support
…and replies are vague, delayed, or defensive (“Why are you so worried about this?”), that’s concerning.
- Reports From Recently Matched or Graduated Residents
If you can, reach out on LinkedIn or via mutual contacts:
- Ask IMGs who trained there about their real experiences.
- See whether comments differ between current vs past residents.
If graduates say, “It’s improved a bit, but many issues remain,” treat it as a caution flag.
Subtle Cultural Red Flags: Reading Between the Lines
Some residency red flags are subtle but still important when deciding whether a program might be malignant or just a poor fit for your needs.

Misalignment Between Mission Statement and Reality
Many transitional year programs advertise:
- “Resident-centered education”
- “Strong wellness focus”
- “Collaborative team-based culture”
But on interview day, you notice:
- Residents constantly interrupted by pages during “protected” time
- Leadership describing residents primarily as “coverage”
- Little discussion about what residents want after TY year
This mismatch suggests the mission statement may be more marketing than reality.
Extreme Hierarchy and Lack of Psychological Safety
Ask about:
- How residents give feedback about rotations or faculty
- Whether residents serve on key committees (GME, wellness, quality)
Red flags:
- All decisions made top-down with minimal resident input
- Residents punished socially or academically for voicing concerns
- Stories about residents being “blacklisted” or “in trouble” for minor mistakes
Psychological safety—feeling able to speak up without punishment—is essential to both education and patient safety.
Unclear Policies on Harassment and Discrimination
Even in 2025, harassment still occurs in training. IMGs, especially women and other underrepresented groups, are at higher risk.
Ask directly:
- “How do you handle discrimination or harassment from staff, faculty, or patients?”
- “What resources are there if the issue involves someone in leadership?”
Red flags:
- Vague answers like “we deal with it case by case” without describing formal processes.
- No mention of institutional offices (Title IX, HR, ombuds services, GME office).
- Minimizing or joking about such scenarios.
How IMGs Can Proactively Evaluate TY Programs and Protect Themselves
Recognizing a malignant transitional year program is only half the battle. The other half is building a deliberate strategy to choose supportive programs and protect your well-being.
Step 1: Build a Structured Comparison Tool
Create a spreadsheet for each TY program on your list with sections like:
Workload & Structure:
- Average hours/week
- Call frequency and type
- Patient caps
- Night float vs 24-hour calls
Education:
- Number of weekly conferences
- Protected didactic time (is it truly protected?)
- Simulation opportunities, bootcamps, case conferences
Culture & Wellness:
- Residents’ description of camaraderie
- Leadership’s focus on wellness vs productivity
- Availability of mental health services
IMG-Specific Factors:
- Visa sponsorship type and reliability
- History of IMGs in the program
- Support with cultural acclimation and communication skills
As you gather data from websites, interviews, and conversations, you’ll see patterns emerge—and red flags will stand out more clearly.
Step 2: Ask Hard, Specific Questions
You are not being difficult by asking about potential toxicity; you are being professional. Examples tailored to transitional year:
- “How do you balance service needs with education, especially for TY residents who will enter various specialties?”
- “Can you share how you handled a recent situation where a resident struggled—what support did they receive?”
- “How are duty hours monitored and enforced?”
- “What percentage of your TY residents are IMGs, and how have you supported them historically?”
Watch not only for the content of the answer, but also for the tone: defensive vs collaborative.
Step 3: Prioritize Programs That Treat TY Residents as True Learners
Some institutions view TY residents as extra labor compared to categorical residents. Positive signs include:
- TY residents invited to the same wellness initiatives, research meetings, and mentorship as categorical residents
- TY-specific advising to align the year with your long-term career plans (e.g., radiology electives, anesthesia exposure)
- A track record of TY graduates successfully matching into competitive advanced programs
If TY residents appear invisible or unintegrated, that’s a concern.
Step 4: Weigh Safety Over Prestige
For many IMGs, the temptation is to rank the most “famous” or high-volume academic centers highest. But:
- A mid-tier program with a strong, humane culture may prepare you better than a “prestige” institution with a malignant environment.
- Your performance, letters of recommendation, and Step 3 scores matter more than the brand name of your TY in most specialties.
If your gut tells you a program is toxic, trust that instinct—even if the hospital logo is impressive.
Step 5: Know Your Options if Things Go Wrong
Despite best efforts, some IMGs may still land in a problematic program. You are not powerless.
- Document Issues: Keep a professional record of duty hour violations, unsafe assignments, or abusive incidents (dates, times, witnesses).
- Use Internal Channels: Talk to chief residents, program director, or GME office as appropriate.
- External Resources:
- ACGME has confidential complaint mechanisms.
- ECFMG and visa sponsors can provide guidance for IMGs.
- Self-Care and Safety: Your physical and mental safety always come first. Seek counseling when needed and involve supportive faculty when possible.
FAQs: Malignant Transitional Year Programs for IMGs
1. How can I tell the difference between a “busy but good” program and a truly malignant residency program?
A busy but healthy program will acknowledge workload openly, emphasize education, and describe supports (extra coverage when residents are overwhelmed, wellness resources, responsive leadership). Residents may say, “We work hard, but we’re supported.” A malignant program tends to minimize concerns, blame residents who struggle, and lack concrete systems for wellness or remediation. Residents may say, “We survive,” “Don’t get on their bad side,” or give vague, nervous answers when you ask about challenges.
2. Are community transitional year programs safer than academic ones for IMGs?
Not necessarily. Many community TY programs are excellent, with strong teaching and supportive cultures, and many academic centers are superb as well. Malignancy is about culture and leadership, not the label “community” vs “academic.” Evaluate each TY program on its own merits: transparency, resident satisfaction, support for IMGs, and attention to wellness and education.
3. What specific questions should IMGs ask about visa issues to detect red flags?
Ask: “How many current residents are on J‑1 or H‑1B visas?” “Have there been any recent issues with visa renewal or sponsorship?” “If a resident faces performance concerns, how do you handle this in the context of visa timelines?” Red flags include dismissive answers (“You don’t need to worry about that”), lack of experience with IMGs, or hints that visa status is used as leverage for extra work.
4. If I realize my program is malignant after starting, is it possible to transfer to another TY or preliminary spot?
Transfers are challenging but not impossible. Options depend on timing, performance, and available positions. Start by discussing issues with trusted faculty or the GME office. They may help modify rotations, provide extra support, or—if necessary—facilitate a transfer. Simultaneously, document serious issues and be aware of ACGME complaint channels. For IMGs, visa implications must be carefully managed in coordination with ECFMG or your visa sponsor.
Choosing a transitional year program as an international medical graduate is one of the most important early decisions in your career. By learning to recognize malignant residency program patterns and toxic program signs, you can prioritize environments that respect you as both a physician and a human being—giving you a strong, healthy launch into your advanced specialty.






















