Identifying malignant residency programs is one of the most important – and least openly discussed – steps in the IMG residency guide process, especially for those interested in Emergency Medicine-Internal Medicine (EM IM combined) training. As an international medical graduate, your margin for error is often smaller: visas, limited interview numbers, and financial constraints mean that matching into a toxic program can be particularly damaging to your career and well-being.
This article focuses on how an IMG can recognize residency red flags specific to Emergency Medicine-Internal Medicine combined programs and avoid landing in a malignant residency program.
Understanding “Malignant” Residency Programs
In residency culture, a “malignant” program is shorthand for a toxic training environment that consistently harms resident well-being, education, or career prospects. It’s not about being “hard” or “demanding.” Many excellent EM IM combined programs are rigorous yet supportive. Malignancy is about chronic dysfunction.
What “Malignant” Usually Means in Practice
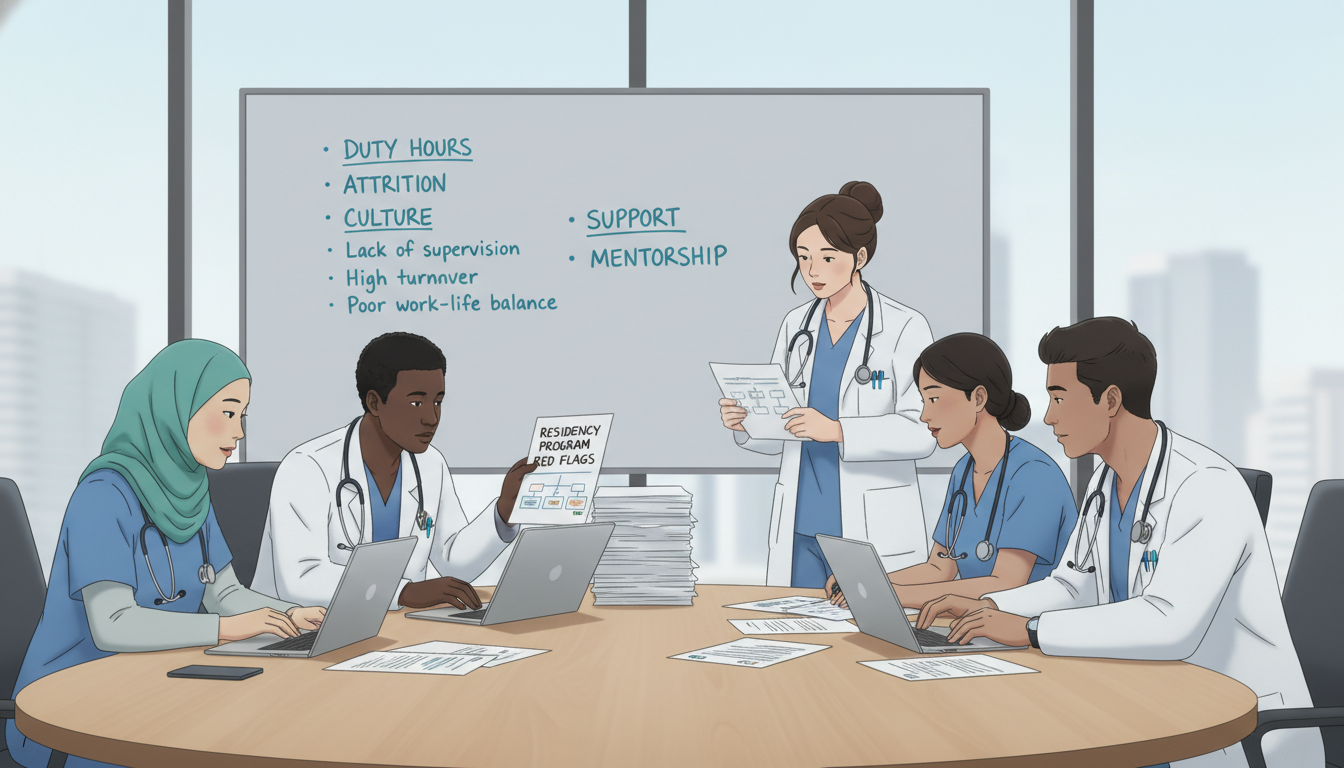
Characteristics commonly associated with a malignant residency program include:
- Chronic disregard for duty-hour rules or safe workloads
- Systemic bullying, intimidation, or humiliation
- Poor supervision leading to unsafe patient care
- Punitive culture: retaliation for raising concerns or calling in sick
- Lack of educational structure: residents functioning as cheap labor
- High burnout and attrition without meaningful changes
- Dishonesty in recruitment: what’s promised on interview day doesn’t match reality
For an international medical graduate, these problems can be amplified by:
- Visa dependence on the program (fear of speaking up)
- Limited local support system
- Unfamiliarity with U.S. workplace norms and resident rights
- Greater vulnerability to discrimination or bias
EM IM Combined: Why This Specialty Needs Extra Scrutiny
EM IM combined training is demanding even in the best settings:
- Split identity: you are both emergency medicine and internal medicine
- More rotations, more call variations, more expectations
- Requirements from two departments, two sets of leadership, and often two distinct cultures
- Pressure to cover high-acuity areas (ED resuscitations) and high-volume internal medicine services
Because of this complexity, malignant traits can appear in unique ways:
- EM and IM leadership not coordinated – residents fall through the cracks
- EM shifts plus IM call patterns create unsustainable schedules
- EM IM residents used as “floaters” to fill gaps in both departments
- Less protected teaching time than categorical EM or IM residents
A key skill in your IMG residency guide is learning to distinguish “hard but fair” from “truly toxic.”
Core Residency Red Flags: What to Watch for in Any Program
Some toxic program signs are universal, regardless of specialty. You should consider these non-negotiable warning signs, especially as an IMG.
1. Chronic Duty-Hour Violations and Unsafe Workloads
Every resident occasionally has a long day, but malignant programs have systematic problems:
- Residents regularly exceed 80 hours/week
- Frequent 28–30+ hour shifts with no real rest
- “Off days” that include expected chart work, teaching sessions, or “voluntary” tasks that are really mandatory
- Residents discouraged from logging hours accurately
Why this is dangerous for IMGs:
You may hesitate to complain due to visa concerns or fear of being labeled “weak.” But consistently unsafe workloads harm your health, your board preparation, and patient safety.
How to detect it:
- Ask on interview day or in follow-up emails:
- “How often do residents reach the 80-hour limit?”
- “What happens if residents report regular overages?”
- “Are there services known for constant duty-hour violations?”
- Look for vague or defensive answers: “We’re a hardworking program” without specifics; or “We don’t really track hours – we trust you.”
2. Culture of Fear, Shaming, or Humiliation
A malignant residency program often uses fear to control residents:
- Attendings or seniors yell, belittle, or humiliate residents in front of patients or staff
- “Teaching” is mostly public shaming for not knowing answers
- Mistakes are punished instead of debriefed and used for learning
- Residents are afraid to ask for help
For IMGs, this can feel especially isolating if language or cultural differences are used as a weapon (“Your accent is a problem”; “Maybe people in your country do that, but here we don’t.”).
Detection strategies:
- Ask directly in resident-only sessions:
- “How comfortable do you feel asking questions in front of attendings?”
- “When errors occur, how are they handled?”
- “Do you feel psychologically safe here?”
- Note body language and tone. If residents glance at each other, hesitate, or give rehearsed answers, that’s concerning.
3. High Attrition and Frequent Transfers
One of the clearest residency red flags: people keep leaving.
Patterns to watch for:
- Multiple residents per year leave, transfer, or “disappear” from class photos
- Long-term unfilled or “recycled” positions
- Leadership minimizes it: “They weren’t a good fit” without deeper explanation
For an IMG:
Transfers can be harder due to visa logistics. If many residents (especially U.S. grads) are still leaving despite easier transfer options, that’s a strong sign of malignancy.
Questions to ask:
- “How many residents have left the program in the past 3–5 years?”
- “Did they transfer to other programs or leave medicine entirely?”
- “What changes has the program made in response?”
Evasive or defensive responses are not a good sign.
4. Poor Transparency and Dishonesty
Toxic programs often hide critical information:
- No resident handbook or rotation schedule available
- Inconsistent answers from faculty and residents about call, vacation, or evaluation
- Negative online reviews dismissed as “disgruntled former residents” without acknowledging any truth
How to explore this:
- Compare information from multiple sources: website, interview day, residents, unofficial chats.
- Ask residents to describe a sample month’s schedule in detail.
- Ask: “What surprised you after you started that didn’t match what you were told during interviews?”
If multiple residents quietly hint that “things were not as advertised,” be cautious.
5. Lack of Career Support and Board Preparation
A malignant residency program often fails to prepare residents for independent practice or fellowships:
- Low board pass rates, poorly tracked or undisclosed
- Minimal dedicated teaching, simulation, or didactics
- No structure for in-training exam review or remediation
- Little support for fellowship applications, letters, or research
For an international medical graduate, this is especially damaging – you may rely more heavily on strong letters, mentorship, and board success to stay competitive in the U.S. market.
EM IM Combined–Specific Toxic Program Signs
Because EM IM combined training spans two major departments, some malignant patterns are unique. These should be central in any IMG residency guide for this pathway.
1. EM and IM Departments Poorly Integrated
Healthy EM IM combined programs have coordinated leadership and a clear identity for combined residents. Red flags include:
- EM IM residents unsure who their “go-to” program director really is
- Conflicting expectations from EM and IM leadership
- Schedule conflicts where one department ignores the other’s requirements
- Lack of clear combined curriculum, no dedicated EM IM meetings
Example:
You’re scheduled for an overnight EM shift but also expected at an early morning IM conference – and no one in leadership sees a problem.
Questions to ask:
- “Who is the primary program director for EM IM residents?”
- “How often do EM and IM leadership meet to discuss the combined program?”
- “Do EM IM residents have dedicated meetings or check-ins separate from categorical EM or IM?”
Vague structures often translate into resident suffering.
2. EM IM Residents Used as Flexible Labor
In malignant combined programs, EM IM residents become “plug-and-play” fillers:
- Frequently pulled from educational rotations to cover service gaps
- Routinely assigned the toughest or least educational shifts because “you’re dual trained”
- Asked to stay late or come in extra because “you’re more versatile”
This can erode both education and well-being.
Red flags in conversation:
- Residents say, “We’re always the ones they call when someone is out.”
- EM IM residents have more night shifts or extra calls than either categorical group.
- Leadership focuses on your “value” to the system more than your educational needs.
Ask current EM IM residents:
- “Do you feel you’re treated more as workforce coverage or as learners?”
- “Are there times you’re pulled from scheduled rotations to cover gaps?”
- “How does your schedule compare to categorical EM and IM residents?”
3. Imbalanced Training: Strong in One, Weak in the Other
A malignant or poorly designed EM IM combined program may heavily favor one department:
- Strong EM, weak IM:
- Excellent ED teaching, but medicine wards are understaffed and chaotic
- Little exposure to chronic disease management or continuity clinic quality
- Strong IM, weak EM:
- Robust inpatient teaching, but ED shifts focused on “see more, learn less,” minimal feedback
- EM IM residents excluded from key experiences on one side (e.g., not included in EMS, ultrasound, critical care procedures) because spots go to categorical EM residents
As an IMG, you should protect your dual-identity training; otherwise, you risk graduating underprepared in one of your two specialties.
Ask:
- “Do EM IM residents get equal access to EM procedure opportunities and key rotations?”
- “Do you ever feel like an outsider in either department?”
- “Are there leadership champions in both EM and IM who specifically look out for EM IM residents?”
4. No Clear Pathway for EM IM Graduate Outcomes
Healthy combined programs can show you what happens to their graduates. Red flags:
- Program cannot or will not describe where recent EM IM grads went
- No data on fellowships, academic positions, or community jobs
- Alumni outcomes are vague: “They’re doing fine somewhere”
For an international medical graduate, you need to know:
- Are EM IM grads getting visas sponsored for fellowships or jobs?
- Do EM IM alumni from this program face hiring bias due to their training?
Ask targeted questions:
- “Where have your recent EM IM graduates matched for fellowship or obtained jobs?”
- “Do you track graduate positions and board pass rates specifically for EM IM?”
- “How do employers view graduates from your EM IM program?”
IMG-Specific Vulnerabilities: What Makes a Program Especially Dangerous for You
Not all difficult programs are equally risky for an IMG. Some features pose disproportionate danger if you depend on visas and have less local support.
1. Weak or Unclear Visa Support
A program may seem supportive but be administratively unreliable:
- No clear statement on the website about J-1/H-1B sponsorship
- Leadership “hopes” to continue H-1B support but has no institutional backing
- Past examples of residents losing visa status or delayed applications
For an international medical graduate, this is more than an inconvenience; it can determine whether you can remain in the U.S.
Ask:
- “How many current residents are on J-1 or H-1B?”
- “Have you ever had a visa application denied or delayed for a resident?”
- “Does the GME office have dedicated staff for visa processing?”
Programs with frequent “visa surprises” are high-risk.
2. Poor Support for Cultural and Communication Adaptation
EM and IM both require complex communication with patients, consultants, and team members. A malignant residency program may blame an IMG’s background for systemic problems:
- Little support for accent, communication style, or documentation training
- Criticism framed around where you’re from instead of objective performance
- No structured feedback; problems only appear during annual evaluations
Look for:
- Mentorship systems that include IMGs
- Simulation or teaching about communication with consultants and difficult patients
- A pattern of IMGs struggling or being placed on remediation disproportionately
Ask current IMGs:
- “How did the program support your transition into U.S. clinical practice?”
- “Have you ever felt unfairly judged because of your background?”
- “Do you feel comfortable raising concerns about bias?”
3. Lack of Wellness Infrastructure and Mental Health Support
Residency is stressful; EM IM combined especially so. A malignant program often:
- Claims to support wellness but has no protected time or resources
- Discourages using mental health services (“Will this affect my evaluations?”)
- Frowns upon sick calls; residents feel guilty or punished for being ill
For IMGs away from family and familiar support networks, this is particularly dangerous.
Ask:
- “Are residents able to access mental health services confidentially?”
- “What happens if a resident needs a leave of absence?”
- “How does the program handle pregnancy, family emergencies, or burnout?”
Look for concrete structures – not just inspirational words.
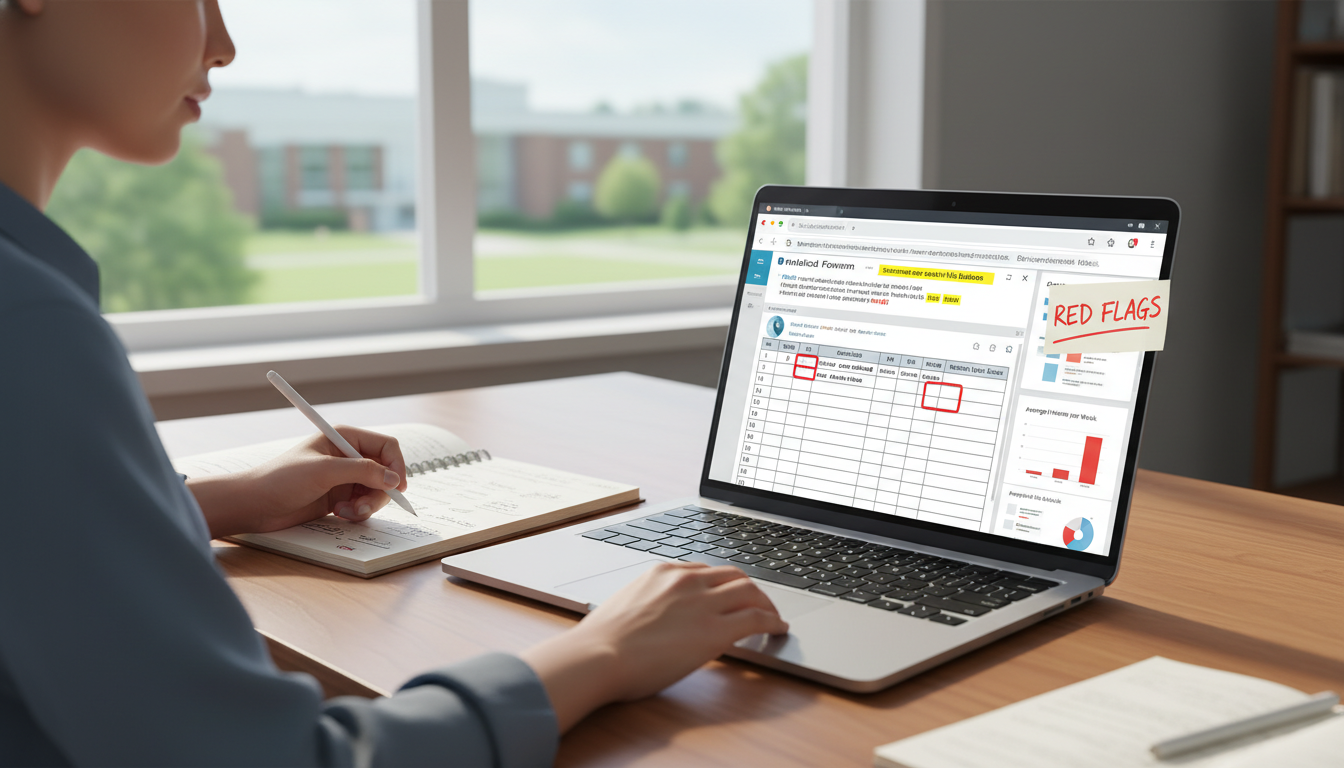
How to Investigate Programs: Practical Strategies for IMGs
Identifying a malignant residency program requires more than reading the official website. Use a structured, multi-step approach.
Step 1: Pre-Interview Research
Before you apply or accept interviews:
Review official data:
- ACGME accreditation history (any warnings or citations?)
- Board pass rates (if available)
- Number of EM IM positions vs. categorical EM and IM
Search beyond the website:
- Forums (e.g., Reddit, Student Doctor Network) – read patterns, not single posts
- Alumni LinkedIn profiles to see where graduates end up
- Hospital reviews focused on staff satisfaction and ED culture
Build a “red-flag checklist”:
- High attrition?
- Mixed or negative online sentiment?
- Very vague description of EM IM training structure?
Step 2: Targeted Interview Questions
Use interview day to test specific concerns. Ask different people the same questions and look for consistency.
Sample questions for EM IM combined applicants (especially IMGs):
Regarding integration:
- “How are EM IM residents represented in program leadership and committees?”
- “Who advocates specifically for EM IM when conflicts arise between EM and IM?”
Regarding workload and duty hours:
- “On which services do residents most commonly approach or exceed duty hours?”
- “Can you describe any recent changes made to improve workload or wellness?”
Regarding culture:
- “If a resident feels mistreated or bullied, what concrete steps can they take, and what typically happens?”
- “Can you share an example of feedback from residents that led to an actual program change?”
Regarding IMG experience:
- “How many current or recent EM IM residents are IMGs?”
- “What specific support systems are available for international graduates?”
Step 3: Resident-Only Sessions – Read Between the Lines
Resident-only Q&A is where you’ll often glimpse the program’s reality.
Pay attention to:
- Nonverbal cues: Are residents relaxed, or do they seem cautious and scripted?
- Consistency: Do stories from different residents align?
- Language used:
- “We work hard, but we’re supported” → often okay
- “It’s survivable” or “You just have to keep your head down” → concerning
Try questions like:
- “Is there anything you wish you had known about the program before ranking it?”
- “Have any residents left or transferred during your time here? Why?”
- “When you’re on your hardest rotation, do you still feel like you’re learning?”
Step 4: Post-Interview Follow-Up and Networking
After interviews:
- Email a current resident (especially an IMG or EM IM resident) with a few specific follow-up questions.
- Reach out via LinkedIn to recent graduates if possible; ask about:
- Preparedness for independent practice
- Any major changes or turmoil during their time
- How the program handled crises (COVID surges, staffing issues)
If multiple, independent sources hint at the same problems, treat it seriously.
Step 5: Adjusting Your Rank List
No program will be perfect, but for EM IM combined and for IMGs, it’s wise to:
- Avoid programs with repeated reports of bullying, retaliation, or unsafe workloads, even if located in a desirable city.
- Prefer slightly less “prestigious” but stable and supportive programs over flashy but toxic ones.
- Consider how much risk you can tolerate: If your visa and entire career hinge on this match, leaning away from known-problem programs is usually wise.
Balancing Reality: Tough vs. Truly Malignant
Every residency – especially in acute specialties like emergency medicine internal medicine – will include:
- Long, exhausting shifts
- High-acuity situations with life-or-death decisions
- Stressful rotations and steep learning curves
You’re not trying to avoid hard work. You’re trying to avoid chronic, systemic harm.
A tough but healthy program will usually show:
- Honest acknowledgment of challenges
- Visible efforts to improve schedules and wellness
- Concrete examples of leadership responding to resident feedback
- Graduates who speak positively about training despite the difficulty
A malignant program tends to:
- Dismiss or minimize resident concerns (“This is just how residency is”)
- Blame individuals rather than address system issues
- Punish those who speak up
- Have a pattern of residents leaving, burning out, or failing boards
As an IMG applying to EM IM combined training, your best protection is structured skepticism: ask, verify, and compare.
FAQs: Malignant Programs in EM IM Combined for IMGs
1. How can I tell if a negative online review about a program is credible?
Look for patterns rather than isolated comments. If multiple reviews across different years and platforms describe similar issues (e.g., chronic duty-hour violations, bullying by specific leaders, EM IM residents used as service fillers), take it seriously. Balance this by asking current residents directly; if their answers are vague, overly guarded, or contradict those patterns without explanation, that’s a red flag.
2. As an IMG, should I avoid all programs with any red flags, or only the very worst ones?
Almost every residency has some weaknesses. Focus on severity and persistence:
- Deal-breakers: systemic bullying, retaliation for raising concerns, frequent unaddressed duty-hour violations, and high attrition without meaningful changes.
- Manageable concerns: heavy workload but responsive leadership; growing but honest programs; clear efforts to improve EM IM integration.
Your threshold may depend on your personal resilience, visa needs, and support system, but truly malignant traits are rarely worth the risk.
3. Are community-based EM IM combined programs safer or more malignant than academic ones for IMGs?
Neither setting is automatically better or worse. Academic centers may offer more resources and structured education but can sometimes have more hierarchy and bureaucracy. Community programs may provide more hands-on experience but can drift toward service-heavy models. Evaluate each individual program on:
- Culture toward IMGs
- EM/IM integration
- Educational structure
- Resident turnover and satisfaction
Use the same toxic program signs and residency red flags described above, regardless of setting.
4. If I realize my program is malignant after matching, what can I do as an IMG?
Options depend on your visa type, specialty, and personal situation, but possible steps include:
- Documenting issues clearly and professionally (dates, incidents, emails)
- Seeking confidential support from GME, ombudsman, or physician wellness services
- Reaching out to trusted faculty mentors for guidance
- Exploring transfer possibilities with extreme care to protect your visa status
- Consulting legal/immigration counsel if your visa is at risk
It’s far better to avoid malignant programs upfront than to escape them later, which is why learning these residency red flags is such a crucial part of the IMG residency guide for EM IM combined applicants.






















