
Understanding “Malignant” Preliminary Medicine Programs
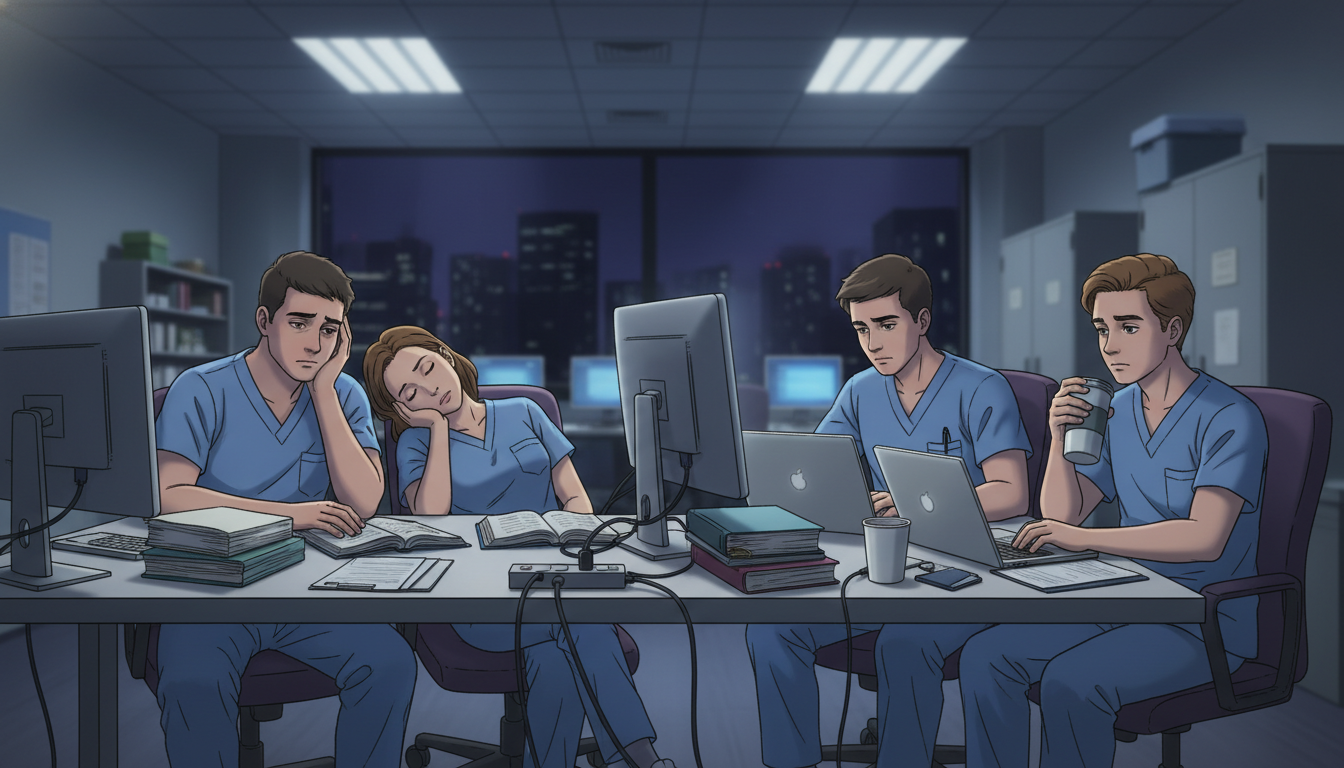
For an MD graduate pursuing a preliminary medicine year (prelim IM) before an advanced specialty (neurology, anesthesiology, radiology, dermatology, ophthalmology, etc.), choosing the right program is critical. A malignant residency program can turn an already demanding year into an unsafe, demoralizing experience that affects your mental health, career prospects, and even patient care.
In the context of a preliminary medicine year, a malignant environment can be especially problematic:
- You are there for only one year, so culture shock hits fast.
- You may have limited leverage, especially if your advanced position is already tied to completing that prelim year.
- Some categorical residents may be protected more than prelims, leaving prelims to absorb disproportionate workload.
This article will help you systematically identify toxic program signs, distinguish between normal residency difficulty and genuine residency red flags, and make safer choices in your allopathic medical school match process.
We will focus specifically on the MD graduate residency applicant in preliminary internal medicine, but most principles apply across specialties.
What “Malignant” Really Means in Residency
The term “malignant” gets used loosely, so it’s important to define what we’re talking about.
A residency program can be:
- High-intensity but healthy: Busy, demanding, but supportive and fair.
- Benign but weak: Low workload, collegial, but poor teaching or weak fellowship placement.
- Malignant/toxic: Systematically harmful to residents’ well-being, education, and professional development.
Core Features of a Malignant Program
While no program is perfect, malignant programs tend to share several consistent characteristics:
Chronic violation of duty hours and basic standards
- Persistent 90–100+ hour weeks.
- Pressure not to log hours honestly.
- No meaningful response when violations are raised.
Punitive or abusive culture
- Public shaming, yelling, belittling residents.
- Threats over honest mistakes.
- Retaliation for raising concerns.
Exploitation of vulnerable groups
- Prelims getting the worst schedules and least support.
- Different rules for categorical vs preliminary residents.
- Disproportionate scut work assigned to specific groups (prelims, IMGs, or certain genders).
Lack of educational value
- Little to no teaching.
- Attendings who are rarely present or uninterested in supervision.
- Service needs consistently prioritized over learning.
High resident burnout, attrition, or failures
- Multiple resignations, dismissals, or transfers.
- Residents failing boards regularly.
- A pervasive “survival” mindset rather than growth.
Dishonesty in recruitment or communication
- Promises on interview day that are routinely broken.
- Gaslighting residents about real issues (“Everyone else is fine; you’re the problem”).
A high-acuity tertiary-care prelim IM program may still be good if the culture supports residents. Malignancy is about how the work and people are managed, not only how hard the year is.
Unique Vulnerabilities of MD Graduates in a Prelim IM Year
As an MD graduate heading into a preliminary medicine year, your situation is distinct from a categorical internal medicine resident:
- You often already have an advanced position (e.g., Radiology PGY-2) contingent on completing PGY-1.
- You may be seen as “temporary labor,” not an investment.
- Your primary mentor network is often in your future specialty, not in medicine.
- Program leadership may prioritize categorical residents’ needs and careers over prelims.
Recognizing this, you need to be especially attuned to residency red flags that signal you could become the “dumping ground” for undesirable work without support.
Common Prelim-Specific Risks
Disproportionate Workload on Prelims
- Prelims doing more nights/floats than categoricals.
- Being pulled frequently from education (noon conference, didactics) to handle admissions or cross-cover.
Minimal Career Support
- No formal advising or feedback for prelims.
- No interest in your future specialty or letters of recommendation.
Limited Protection and Advocacy
- When conflicts arise with nurses, consultants, or attendings, prelims are blamed or left unsupported.
- Prelims not invited to wellness or career development resources that categoricals receive.
Ambiguous Expectations
- No clear orientation about your role.
- Being held to contradictory standards (e.g., “act like a categorical” but without the same rights or resources).
You want a prelim program that views you as a true intern, with full access to teaching, mentorship, and fair scheduling, not as a disposable one-year worker.
Pre-Application Research: Spotting Red Flags Before You Apply
Your first line of defense is careful screening before you even submit your ERAS application. While no single data point is definitive, a pattern of issues can indicate a toxic program.
1. Analyze the Program’s Public Profile
Use the program’s website, social media, and official data.
Positive signs:
- Transparent schedule details (call frequency, night float, ICU rotations).
- Clear, updated information about prelim-specific curricula and resources.
- Evidence that prelim grads go on to strong advanced programs or fellowships.
- Photos and bios that explicitly include preliminary medicine residents.
Red flags:
- Prelims barely mentioned or not listed among residents.
- No details on prelim education, only service descriptions.
- Outdated websites (e.g., current year missing, last update several years ago).
- Overemphasis on “hard-working” and “resilient” without mention of learning or support.
2. Look at ACGME and Board Data
For accredited U.S. programs, investigate:
- ACGME accreditation status: Any warnings or citations?
- Board pass rates for internal medicine, if reported.
Serious concerns:
- Multiple recent citations, especially related to duty hours, supervision, or resident well-being.
- Board pass rates consistently far below national averages without transparent explanation.
3. Use Word-of-Mouth and Online Reports Wisely
Sources include:
- Recent graduates from your allopathic medical school match network.
- Residents/fellows you meet on rotations.
- Online forums (e.g., Reddit, specialty-specific boards).
Approach these with a critical mindset:
- Patterns matter more than one angry post.
- Pay attention when multiple independent people describe:
- Chronic understaffing.
- Prelims being treated poorly.
- High resident turnover or multiple resignations.
4. Carefully Read the Program’s Mission and Culture Language
Sometimes the way a program describes itself hints at trouble:
Watch out for phrases like:
- “Our residents learn to be tough; this is not a program for everyone.”
- “We take pride in our old-school, rigorous training.”
- “We expect our interns to put work above all else.”
These may indicate a culture that romanticizes suffering and normalizes burnout.

Interview Day: Questions and Behaviors That Reveal Malignancy
Interview day is your best opportunity to probe whether a program is simply busy or truly malignant. You will not get a direct “we’re toxic” statement, so you need to ask targeted, concrete questions and observe subtle cues.
1. Smart Questions to Ask Residents
As a prelim IM applicant, ask specifically about how prelims are treated.
About Workload and Fairness
- “How are call and night shifts distributed between categorical and prelim residents?”
- “On a typical ward month, about how many patients are you carrying?”
- “Are duty hours ever violated? If so, how is that handled?”
- “Can you log your hours honestly without pushback?”
Warning signs:
- Residents laugh nervously or look at each other before answering.
- Answers are vague: “It’s busy, but you get used to it.”
- Statements like: “Technically we’re supposed to log accurately, but…”
About Culture and Support
- “How does the program respond when a resident struggles or has a bad outcome?”
- “Has a resident ever had to take medical leave or time off for personal reasons? How was that handled?”
- “If you raise a concern about an attending or workload, do you feel heard?”
Warning signs:
- Residents say they would never talk to leadership about problems.
- Someone hints, “You don’t want to be labeled a complainer.”
- Stories of residents being punished after raising legitimate concerns.
About Prelim-Specific Experience
- “Do prelims attend the same didactics and conferences as categoricals?”
- “Are prelims included in social events, retreats, and wellness initiatives?”
- “Do prelims get any formal mentorship or career advising?”
- “If a prelim has a problem on rotation, who advocates for them?”
Warning signs:
- Residents don’t know how prelims’ schedules are structured.
- Prelims or seniors state, “You’re just here for a year, so…”
2. Questions for Faculty and Program Leadership
Faculty and leadership may paint a rosier picture, but specific questions can still be revealing.
Ask:
- “What changes have you made in response to resident feedback over the last 2–3 years?”
- “How do you monitor for burnout among residents?”
- “Can you describe any recent challenges the program faced and how you addressed them?”
- “How do you ensure prelims receive an educational experience comparable to categoricals?”
Red flags:
- Leaders cannot name any changes made in response to feedback.
- Dismissive attitude toward wellness: “Residency is supposed to be hard.”
- Vague or absent answers about prelims’ role.
3. Nonverbal and Environmental Cues
Observe carefully:
- Do residents appear exhausted, withdrawn, or fearful around leadership?
- Are residents candid when leadership is not present?
- Do they complain only after asking you to “keep this off the record”?
- Are there signs of disorganization—chaotic schedules, confusion about rotations?
One or two tired-looking residents is normal; a roomful of people who appear defeated is not.
Concrete Red Flags vs. Acceptable Challenges
Not every difficult aspect of a program means it’s malignant. You should distinguish between hard but healthy and truly toxic program signs.
Acceptable (But Tough) Features
These may represent a challenging but valuable prelim year:
High patient volume with heavy floor months, but:
- Reasonable caps.
- Consistent attending supervision.
- Protected time for teaching (and you mostly get to attend).
Frequent nights or ICU blocks, but:
- Compliant duty hours overall.
- Clear backup system when volume is unsafe.
- Equitable distribution among interns, including categoricals.
Limited resources (community hospital setting), but:
- Strong clinical autonomy.
- Faculty engaged in bedside teaching.
- Warm, collaborative culture among residents and nurses.
Strong Red Flags Suggesting Malignancy
When you see several of the following, be cautious about ranking that program:
Systematic Duty Hour Abuse
- Regular 28–30 hour calls without valid justification.
- Consistent logging of 80 hours when everyone admits working 100.
- Implicit or explicit threats for honest logging.
Pattern of Prelim Exploitation
- Prelims disproportionately assigned undesirable rotations (e.g., endless night float, cross-cover).
- Prelims regularly miss conferences due to “service needs.”
- Prelims not allowed vacation during key periods while categoricals are.
Lack of Supervision and Unsafe Practices
- Interns cross-covering enormous numbers of patients alone.
- Night shifts with no in-house attending for high-acuity services.
- Culture of discouraging escalation (“Don’t bother the attending”).
Hostile, Shaming Behavior
- Attendings or seniors yelling, insulting, or humiliating residents.
- Morbidity and mortality conferences conducted as blame sessions, not learning opportunities.
- People brag about “weeding out the weak.”
High Attrition and Turnover
- Multiple residents leaving or being dismissed in recent years.
- Graduates who speak about “just surviving” rather than learning.
- Faculty turnover that destabilizes the program.
Minimal Interest in Resident Education
- Didactics routinely canceled for service needs.
- No protected board review or curriculum.
- Evaluations and feedback rarely provided.
These behaviors don’t just make your year unpleasant; they can put your license, your future advanced position, and patient safety at risk.
Strategies to Protect Yourself Before and During the Prelim Year
Once you’ve identified relative risk, you still need practical strategies to protect your well-being and career.
1. Creating a Smart Rank List
As an MD graduate, you may be applying broadly. To avoid a malignant residency program, use a structured approach:
Group programs by risk level:
- Green: Supportive culture, good supervision, prelims integrated fully.
- Yellow: Busy programs with some concerns but no major red flags.
- Red: Multiple signs of toxicity or unclear data.
Balance location and prestige against culture:
- A highly prestigious name is rarely worth a miserable, unsafe year.
- A solid community-based prelim with a healthy culture often beats a famous but malignant academic center.
If your advanced position allows flexibility, discuss with your future department (e.g., radiology, anesthesia) whether they have recommended prelim affiliates or programs to avoid.
2. Use Visiting Rotations Wisely
If you rotate at a potential prelim site:
- Pay attention to how interns interact with each other and with nursing staff.
- See whether prelims are integrated into the team or treated as outsiders.
- Ask interns privately: “If you had to choose again, would you come here?”
A month on the wards often reveals more than a polished interview day.
3. Set Boundaries and Document Issues
If you find yourself matched to a program that turns out worse than expected:
Know your rights:
- ACGME duty hour and supervision standards.
- Institutional GME office and ombuds services.
Document consistently:
- Keep a log of shifts, patient loads, unsafe situations.
- Save relevant emails or written communication.
Escalate strategically:
- Start with chief residents or a trusted faculty member.
- If needed, use anonymous feedback mechanisms or GME ombuds.
Your goal is not to wage war but to protect yourself and your license, especially with an advanced residency awaiting you.
4. Maintain External Support and Perspective
Because your long-term home is your advanced specialty, cultivate:
- Mentors in your advanced field who understand prelim dynamics.
- Peers from medical school or other prelims at nearby hospitals.
- Healthy routines outside work: exercise, sleep hygiene, small daily rituals.
If distress becomes significant:
- Access confidential institutional mental health resources.
- Do not hesitate to seek outside counseling or therapy.
A malignant environment can distort your sense of self-worth. Regular contact with people outside the toxic bubble helps you maintain perspective.
Summary: What an MD Graduate Should Look for in a Prelim IM Program
When evaluating preliminary medicine year options, your priority is an environment where you can:
- Work hard but safely.
- Learn internal medicine fundamentals.
- Preserve your health and motivation for your advanced specialty.
To avoid a malignant residency program, focus on these key questions:
- Are prelims treated as full members of the intern class, or as expendable labor?
- Are duty hours and supervision respected in practice, not just on paper?
- Do residents feel safe raising concerns without retaliation?
- Is there evidence of real teaching, not just nonstop service?
- Do current residents—especially prelims—seem tired but proud, or burnt out and hopeless?
By combining pre-application research, sharp interview-day observation, and ongoing self-advocacy, you can greatly reduce your risk of landing in a toxic training environment and ensure your prelim IM year becomes a strong foundation instead of a trauma to recover from.
FAQ: Malignant Programs and the Preliminary Medicine Year
1. Is it normal for a prelim IM year to feel harder than medical school?
Yes. Almost all residents experience a steep learning curve and fatigue during PGY-1. Long hours, responsibility for patient care, and night shifts are standard. What is not normal is chronic duty hour abuse, lack of supervision, or a culture of fear and humiliation. A hard but healthy program challenges you while still respecting your humanity, education, and safety.
2. Are community hospital prelim programs less malignant than academic centers?
Not necessarily. Both community and academic programs can be excellent or toxic. Community programs may be more clinically intense but collegial; some academic centers may be highly structured but impersonal. Evaluate each program individually using the residency red flags outlined above rather than assuming based on setting or prestige.
3. How much should I weigh a program’s reputation versus its culture?
For a preliminary medicine year, culture and safety should generally outweigh prestige. Your main goal is to become a competent internist, stay healthy, and preserve your trajectory into your advanced specialty. A well-run, mid-tier program often serves you better than a brand-name institution with a toxic program culture, especially when both will satisfy your advanced program’s PGY-1 requirement.
4. What if I match into a program that turns out to be malignant? Can I transfer?
Transfers are possible but difficult. If the environment is truly unsafe or abusive:
- Document issues carefully (duty hour violations, unsafe patient loads, lack of supervision).
- Seek help from chief residents, program leadership, and the GME office.
- If necessary, consult your future advanced program leadership—they have a vested interest in you completing a viable PGY-1. Your first priority is to protect your physical and mental health; if you can’t reasonably do that, exploring transfer options or formal grievances may be appropriate.






















