
Why “Malignant” Programs Matter So Much for Non‑US Citizen IMGs in OB/GYN
Choosing an obstetrics & gynecology residency is never easy, but for a non-US citizen IMG the stakes are even higher. Visa dependence, limited interview opportunities, and unfamiliarity with US hospital culture can make you more vulnerable to landing in a malignant residency program.
In this context, “malignant” does not mean clinically incompetent—it refers to a toxic training environment where residents are mistreated, chronically overworked, unsupported, or threatened with retaliation if they speak up. These programs may still graduate board‑eligible physicians, but the personal and professional damage to trainees—especially to foreign national medical graduates—can be severe.
This article focuses on how a non-US citizen IMG applying to OB GYN residency can identify malignant programs and residency red flags during the application, interview, and ranking process. You will learn how to:
- Understand what “malignant” and “toxic” really look like in OB/GYN training
- Recognize specific toxic program signs that disproportionately affect IMGs
- Use concrete strategies to gather reliable information before ranking
- Ask targeted questions on interview day that uncover hidden issues
- Protect yourself during the obstetrics match if you are visa-dependent
What Makes an OB/GYN Program “Malignant”?
A malignant residency program is more than just “busy” or “demanding.” OB/GYN is intense everywhere—call nights, emergencies, and high‑risk deliveries are inherent to the specialty. The difference between a rigorous program and a malignant one lies in culture, support, and safety.
Core Features of a Malignant OB/GYN Residency
Across specialties, malignant programs tend to share several core elements:
Chronic Disrespect and Humiliation
- Regular public shaming of residents in ORs, L&D, or conferences
- Attending physicians yelling, insulting intelligence, or using discriminatory language
- “Teaching by intimidation” accepted as normal or even praised
Systemic Violations of Duty Hours and Safety
- Residents routinely work far beyond ACGME limits without logging hours honestly
- Residents “strongly encouraged” to under-report hours
- No protected time to rest, eat, or recover, leading to burnout and safety concerns
Lack of Educational Focus
- Residents used mainly as cheap labor: endless scut work, minimal operative autonomy
- Didactics canceled frequently for service demands
- Few opportunities to do clinics, research, or subspecialty exposure
Retaliation Against Concerns
- Residents punished for speaking up (worse rotations, bad evaluations, blocked fellowships)
- Culture of fear—people say, “Keep your head down if you want to graduate”
- Anonymous feedback mechanisms exist on paper but are not trusted
Abuse of Power
- Threats about promotion or contract renewal used to control behavior
- Unfair remediation or probation used selectively or without clear criteria
- Favoritism toward certain residents; others marginalized or targeted
Why Non‑US Citizen IMGs Are Especially Vulnerable
As a foreign national medical graduate, you may face additional vulnerabilities:
- Visa dependency: Losing your position may mean losing your visa status.
- Limited program mobility: Transferring to another OB/GYN residency is hard, especially as a non-US citizen IMG.
- Cultural unfamiliarity: You may misinterpret inappropriate behavior as “normal US training” or assume you have no right to object.
- Fear of consequences: You might worry that speaking up could lead to non-renewal of contract, jeopardizing your immigration prospects and future career.
Malignant programs sometimes prefer IMGs for exactly these reasons—they assume you will tolerate more and complain less. Recognizing this dynamic is crucial to protecting yourself.
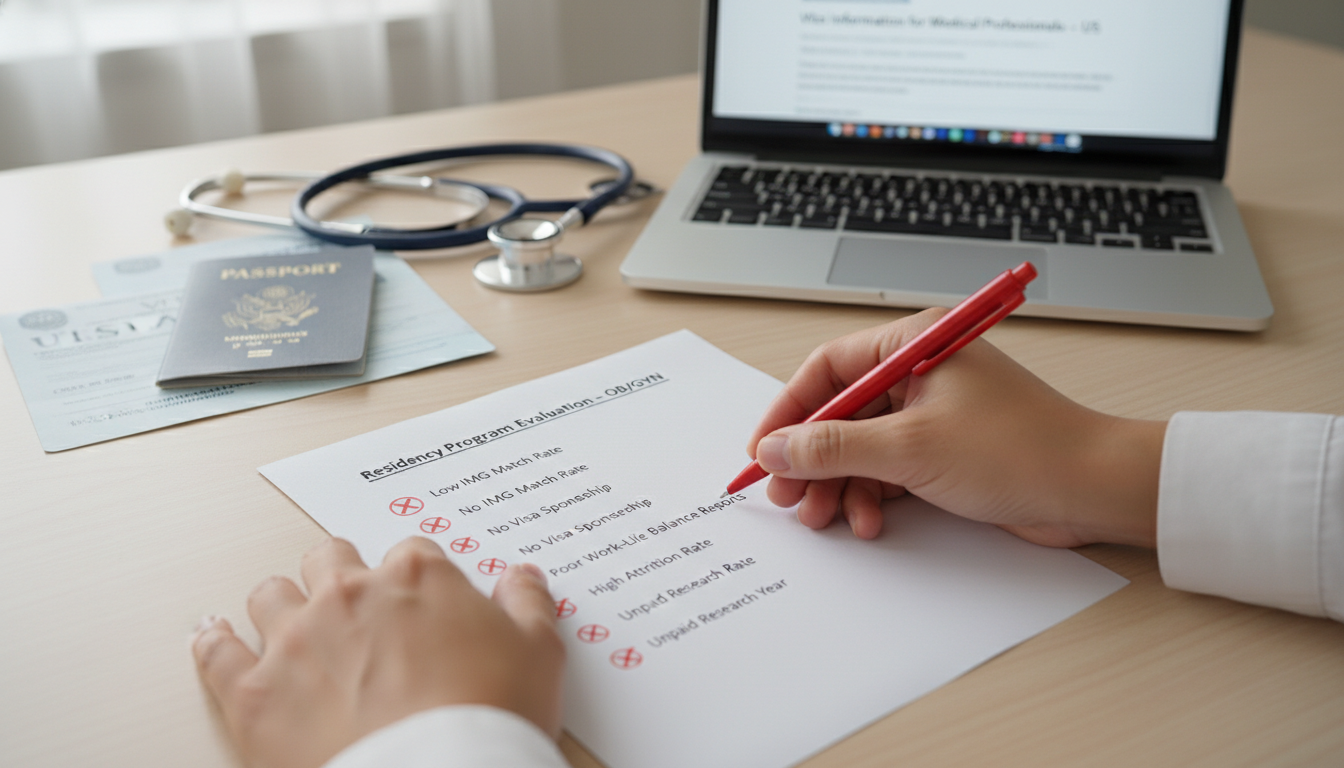
Concrete Residency Red Flags: From “Concerning” to “Danger Zone”
The following sections organize residency red flags into moderate concerns and major danger signs, with special attention to OB/GYN and obstetrics match realities.
1. Red Flags in Program Culture and Communication
Moderate Concerns:
- Residents describe the culture as “intense” or “old-school” without elaborating.
- You see minimal interaction (or awkwardness) between residents and faculty during interview day.
- PD or faculty repeatedly emphasize “resilience” and “thick skin,” but say little about wellness or support.
Major Danger Signs (Malignant/Toxic Program Signs):
- Residents hint that “what’s said here stays here” or that they “can’t say too much.”
- People repeatedly say “This is not a program for everyone” in a way that feels threatening, not aspirational.
- PD or senior faculty make dismissive comments about work‑life balance, wellness, or mental health.
- There is visible tension or fear around certain attendings or leadership.
For a non-US citizen IMG, phrases like “we demand absolute dedication above everything else”—without mentioning support, mentorship, or safety—should be interpreted as potential toxicity, not just “high expectations.”
2. Duty Hours, Workload, and Support
OB/GYN is high-acuity, so you will work hard everywhere. The issue is whether systems exist to protect you from harm.
Questions to Ask Residents:
- “Do you routinely work beyond 80 hours/week? Are those hours honestly logged?”
- “How often do you get a true post‑call day?”
- “Does the program support coverage if someone is sick or experiencing a crisis?”
Red Flags:
- Residents laugh nervously and say, “We work a lot, but we don’t really talk about hours.”
- They tell you, “We just under-report to keep ACGME off our backs.”
- There’s no backup system for illness or family emergencies; residents feel forced to work regardless of health.
For a foreign national medical graduate, overwork combined with no voice significantly increases your risk of burnout and mental health issues, with limited ability to step away or transfer.
3. Surgical and Obstetric Training Quality
You want strong procedural training, but malignant programs may trade off training quality for service needs.
Concerning Signs:
- Junior residents get minimal OR time because attendings or fellows “keep the cases.”
- Residents say they “graduate competent” but seem unsure or hesitant when describing operative experience.
- Gaps in exposure to essential OB/GYN areas (e.g., limited L&D autonomy, very few gynecologic surgeries for certain PGY levels).
Major Danger Signs:
- Residents cannot give clear approximations of case numbers or say things like, “Our numbers look fine on paper, but a lot of cases are double‑counted or supervisory only.”
- Residents regularly operate unsupervised beyond their comfort level without reliable backup, due to staffing issues.
- Residents tell you, even indirectly, “You will be exhausted, but you won’t feel well-trained.”
Malignant programs may exploit residents as service providers while neglecting your development as an independent OB GYN physician.
4. Turnover, Morale, and Resident Outcomes
Key Data Points:
- Resident attrition over the last 5–7 years
- Board pass rates
- Fellowship match (MFM, REI, Gyn Onc, FPMRS, MIGS, etc.)
- Alumni placement (academia vs community; visas vs green cards)
Red Flags:
- Multiple residents have left recently, but explanations are vague or inconsistent.
- Board pass rates are significantly lower than the national average.
- Residents seem exhausted, guarded, or pessimistic when you speak with them.
OB/GYN-Specific Concerns:
- Residents report frequent maternity/paternity leave being discouraged or punished.
- Pregnant residents or those with chronic health conditions tell you they felt unsupported.
For non-US citizen IMGs, ask specifically:
- “Have recent IMGs here successfully gone to fellowship or academic jobs?”
- “Have any IMG residents transferred to other programs—and why?”
A pattern of high attrition, especially among IMGs, is a major sign of a problematic environment.
5. Red Flags Specific to Visa and Non-US Citizen IMG Status
This is where malignant programs can do the greatest harm to a non-US citizen IMG.
Critical Questions:
- “Which visas do you sponsor (J‑1, H‑1B)? For all residents or only selectively?”
- “Have you successfully sponsored H‑1B for OB/GYN residents in the past 3–5 years?”
- “Who handles visa paperwork and how experienced are they?”
- “If there are delays or issues with visas, how does the program support affected residents?”
Serious Red Flags:
- Program leadership uncertain or inconsistent about visa policies (“It depends… we’ll see what GME says”).
- “We’ve never sponsored an H‑1B before, but we might be able to figure it out” (for OB GYN, this is risky).
- Past incidents of residents not starting on time or losing positions due to visa mismanagement.
- Comments implying that IMGs are “easily replaceable” or that the program doesn’t want to “get involved in immigration complications.”
For a non-US citizen IMG, a malignant residency program may:
- Use visa status as leverage to enforce silence or acceptance of mistreatment.
- Apply different rules for IMGs vs US grads (e.g., less flexibility, fewer electives, denied vacations to “handle visa issues”).
These are major residency red flags and you should factor them heavily into your ranking.
How to Research Malignancy Before You Interview
You can start assessing programs long before interview invitations arrive.

1. Use Public Information Strategically
Program Websites:
- Look for evidence of transparency: duty hours, wellness initiatives, mentorship programs, diversity/DEI efforts, and visa information.
- Check how they present residents—does the class include other IMGs or foreign national medical graduates? Are they thriving?
ACGME and FREIDA:
- See if the program has been on ACGME probation or received citations (if publicly available).
- Use FREIDA to confirm visa sponsorship and compare board pass rates.
Social Media and Resident Life:
- Program Instagram/Twitter accounts can reveal a lot:
- Do residents appear genuinely engaged and supported, or is it mostly formal PR content?
- Are achievements, wellness events, and diversity initiatives visible, or are all posts purely clinical/academic?
2. Use Unofficial Sources Carefully
Anonymous forums (Reddit, Student Doctor Network, etc.) can highlight patterns, but individual comments may be biased or outdated.
Tips:
- Focus on repeated themes (e.g., “toxic culture,” “no support,” “everyone is leaving,”) rather than single angry posts.
- Check dates—COVID years were chaotic; separate temporary crisis‑related issues from chronic toxicity.
- Pay special attention to posts mentioning IMGs, visas, or foreign nationals.
If the same program is repeatedly mentioned in discussions of malignant residency program behavior across years and sources, take that seriously.
3. Reach Out to Trusted Contacts
For non-US citizen IMGs, networking is crucial:
- Ask alumni from your medical school who matched into OB/GYN about program reputations.
- Contact mentors or observership supervisors in the US who may know local program cultures.
- If possible, talk to current or recent residents at the program (ideally privately, not just on interview day).
When reaching out, you can say:
- “I’m a non-US citizen IMG very interested in OB/GYN. Could you share your honest perspective on resident support, culture, and how the program treats IMGs or visa-dependent residents?”
Their tone, hesitation, or enthusiasm can be as revealing as their specific words.
Interview Day: Questions and Strategies to Uncover the Truth
Interview day is your best chance to systematically evaluate whether an OB GYN residency is healthy or malignant.
1. What to Ask Residents (Group and One‑on‑One)
Ask open‑ended questions that invite nuance, not rehearsed “sales” answers.
Culture and Support
- “What qualities does someone need to thrive here specifically?”
- “How does leadership respond when residents make mistakes?”
- “Can you share an example of when a resident faced a crisis—illness, family issue, mental health—and how the program responded?”
Workload and Autonomy
- “What is a typical week like on L&D? On Gyn Onc? On nights?”
- “Do you feel you have backup when the unit is extremely busy?”
- “Have there been major duty‑hour violations, and how were they handled?”
Feedback and Safety
- “Do you feel safe giving honest feedback about attendings or rotations?”
- “Is there someone in leadership you truly trust?”
For IMGs and Visa‑Dependent Residents If there are current IMGs:
- “As an IMG, how have you been treated here?”
- “Did you ever feel your visa status limited your opportunities or made it harder to speak up?”
- “Have there been any problems with visas for past residents?”
If there are no current IMGs:
- Ask why. This might be neutral (small applicant pool) or highly concerning (bias).
2. Subtle Cues to Observe
- Resident Interactions: Do they seem supportive of each other—or isolated, tense, and hyper‑competitive?
- Body Language: Do residents seem guarded when faculty are nearby, but more open in breakout/closed sessions?
- Consistency of Answers: Are residents’ answers consistent across different people and settings, or do you hear conflicting stories?
3. Questions for Program Leadership
Ask questions that reveal values and policies, not just statistics.
- “How do you see the program evolving over the next 3–5 years?” (Look for thoughtful, resident‑centered answers.)
- “What systems are in place to protect resident wellness and prevent burnout?”
- “How do you handle conflicts between residents and faculty?”
- “How many residents have left the program in the last 5 years, and why?”
For your status as a non-US citizen IMG:
- “Can you walk me through the process and timeline for visa sponsorship at your institution?”
- “Have any foreign national medical graduate residents here had challenges with visas, and how were those resolved?”
A transparent, confident answer suggests solid infrastructure; vague or evasive responses are major red flags.
Balancing Risk and Opportunity in Your Rank List
After interviews, you’ll likely see a spectrum: from clearly supportive programs to places with several warning signs. How should a non-US citizen IMG weigh these factors in the obstetrics match?
1. Create a Structured Scoring System
For each program, rate from 1–5 on:
- Culture / Respect for residents
- Educational quality (OB and GYN exposure, case volume, fellowships)
- Support for wellness and mental health
- Visa/IMG friendliness and track record
- Geographic/personal fit (family, cost of living, support network)
Then separately flag:
- Serious concerns about malignancy/toxicity
- Uncertainty about visa safety or institutional support
Even one “high‑risk” category (e.g., visa) may outweigh other positives.
2. When to Still Rank a “Concerning” Program
You might still rank a program with moderate concerns if:
- You have few total interviews
- The program is honest about its problems and actively working on improvement
- Current residents—especially IMGs—feel supported and say things are getting better, not worse
Document what you heard and compare across programs. Some “hard but fair” environments are not malignant; they are simply rigorous.
3. When You Should Strongly Consider Not Ranking a Program
Even with limited options, it can be safer not to rank a program if:
- Multiple credible sources describe it as a malignant residency program with sustained, systemic issues.
- IMGs report feeling exploited, threatened, or unsafe.
- There is a history of visa mishandling causing residents to lose status or positions.
- Residents consistently warn you (even indirectly) that they cannot recommend the program.
As a non-US citizen IMG, your immigration status, long‑term health, and career trajectory are on the line. An extra year of reapplying—while difficult—may still be less damaging than enduring years in a toxic program that may harm your mental health, limit your training, and jeopardize board certification or future fellowships.
Final Thoughts: Empowerment Through Information
OB/GYN is a deeply rewarding specialty, and many programs genuinely care about resident growth, wellness, and fairness—even when the workload is high. Your goal as a non-US citizen IMG is to distinguish between:
- High‑expectation, well‑supported programs that will challenge you but help you thrive
- Malignant, toxic environments where systemic disrespect, fear, and exploitation are normalized
By recognizing residency red flags early, asking targeted questions, and prioritizing programs with a strong track record of supporting foreign national medical graduates, you give yourself the best chance of a safe, meaningful training experience and a sustainable career in obstetrics and gynecology.
FAQs: Malignant OB/GYN Programs and Non‑US Citizen IMGs
1. Are all “busy” OB/GYN residencies malignant?
No. OB/GYN is inevitably busy, but in a healthy program, you see:
- Honest duty‑hour reporting
- Real backup when the service is overwhelmed
- Attendings who teach and supervise, not just criticize
- Leadership that responds to concerns without retaliation
“Busy but supported” is very different from “busy, unsafe, and silenced.”
2. Should a non‑US citizen IMG ever avoid all programs that are new or on probation?
Not automatically. New programs or those recently on ACGME probation may be:
- Improving, with young, motivated leadership and more attention to resident feedback
- Risky, if leadership is unstable or problems are institutional
Ask very specific questions:
- What caused the probation or challenges?
- What has changed?
- How do current residents feel now compared to 1–2 years ago?
Judge by current culture and transparency, not just status.
3. How can I verify a program’s visa friendliness beyond what they say on interview day?
- Ask to speak with current or recent IMGs at that institution.
- Contact the program’s GME office directly about institutional policies.
- Look up resident lists and alumni; see how many non-US citizen IMGs they’ve trained and where those graduates are now.
- Ask: “In the last 5 years, have any residents had visa delays or problems? How were those handled?”
Consistency between official answers and IMG experiences is key.
4. What if my only interviews are at programs with some red flags—should I still participate in the match?
Usually yes, but with caution. You can:
- Rank programs in order of least to most concerning, based on malignancy risk and visa safety.
- Reach out to mentors to help interpret what you heard.
- Be mentally prepared that reapplying is an option if you feel a program is truly unsafe or malignant and choose not to rank it.
Your decision should balance urgency to start training with realistic assessment of whether the environment could damage your health, career, or immigration status. When in doubt, seek advice from experienced faculty, IMG advisors, or trusted senior residents who understand both OB/GYN and the challenges of being a non-US citizen IMG.






















