
Why Resident Turnover Matters So Much in a Preliminary Surgery Year
Choosing a preliminary surgery year can feel like stepping onto a moving train—you’re joining an established team, often with a limited guarantee of continuity beyond one year, and with less structural protection than categorical residents. In this environment, resident turnover becomes one of the most important indicators of whether a prelim surgery residency is healthy or struggling.
In surgery especially, you learn by doing—and you can only do that safely within a program that is stable, adequately staffed, and reasonably supportive. When residents are leaving the program, repeatedly transferring, forced out, or not renewed unexpectedly, it almost always points to deeper issues: culture, workload, education, or leadership.
This guide will help you:
- Understand how to recognize resident turnover red flags specific to preliminary surgery
- Interpret what different types of turnover actually mean
- Ask better questions on interview day and pre-interview communication
- Protect yourself from landing in a program with serious program problems that could derail your training or career plans
While no program is perfect, repeated resident departures—especially among prelims—are rarely random. Learning to read these signs early is one of the smartest things you can do as an applicant.
Understanding Resident Turnover in Preliminary Surgery
What “Resident Turnover” Really Means
Resident turnover is more than just “someone left.” It includes:
- Voluntary departures
- Resident transfers to another surgery program
- Resident leaves surgery entirely (switching to another specialty)
- Resident resigns from training for personal or health reasons
- Involuntary departures
- Non-renewal of contract
- Dismissal for performance, professionalism, or disciplinary issues
- Hidden forms of turnover
- Residents “asked to resign” quietly
- Residents technically renewed but pushed into “research years” they did not want
- Residents unintentionally forced out when positions quietly disappear
In a prelim surgery residency, you must distinguish between:
Planned, structural turnover
- Prelim-year residents who always knew they were doing one year then moving on (e.g., to anesthesia, radiology, urology, or re-applying to categorical surgery)
- These are normal and expected.
Unplanned, concerning turnover
- Residents leaving mid-year
- Preliminary residents not finishing the year
- Multiple residents “disappearing” from rosters without explanation
- Sudden shifts in the number of prelim positions offered
- Categorical residents leaving—this is especially concerning in a prelim-heavy program
Your goal isn’t to avoid any program with a single departure—that would be unrealistic. Instead, you’re looking for patterns that suggest systemic program problems.
Why Turnover Is Especially Important in Prelim Surgery
Prelim surgery slots are structurally more vulnerable:
- Prelims often carry heavy clinical workload (night float, ICU, floor coverage)
- Educational investment by the program can be lower than for categorical residents
- Prelim residents may feel replaceable, especially in large services dependent on them
- Contract renewal and promotion pathways can be less transparent
In this context, resident turnover red flags carry extra weight. A high-churn prelim program can:
- Put you at serious risk of burnout and mistakes
- Make it harder to get strong letters, procedural experience, or advocacy for your re-application
- Undermine your chances of matching into a categorical surgery spot or advanced position
Your preliminary year should set you up for your next step—not leave you recovering from a toxic environment.
Major Resident Turnover Warning Signs to Watch For
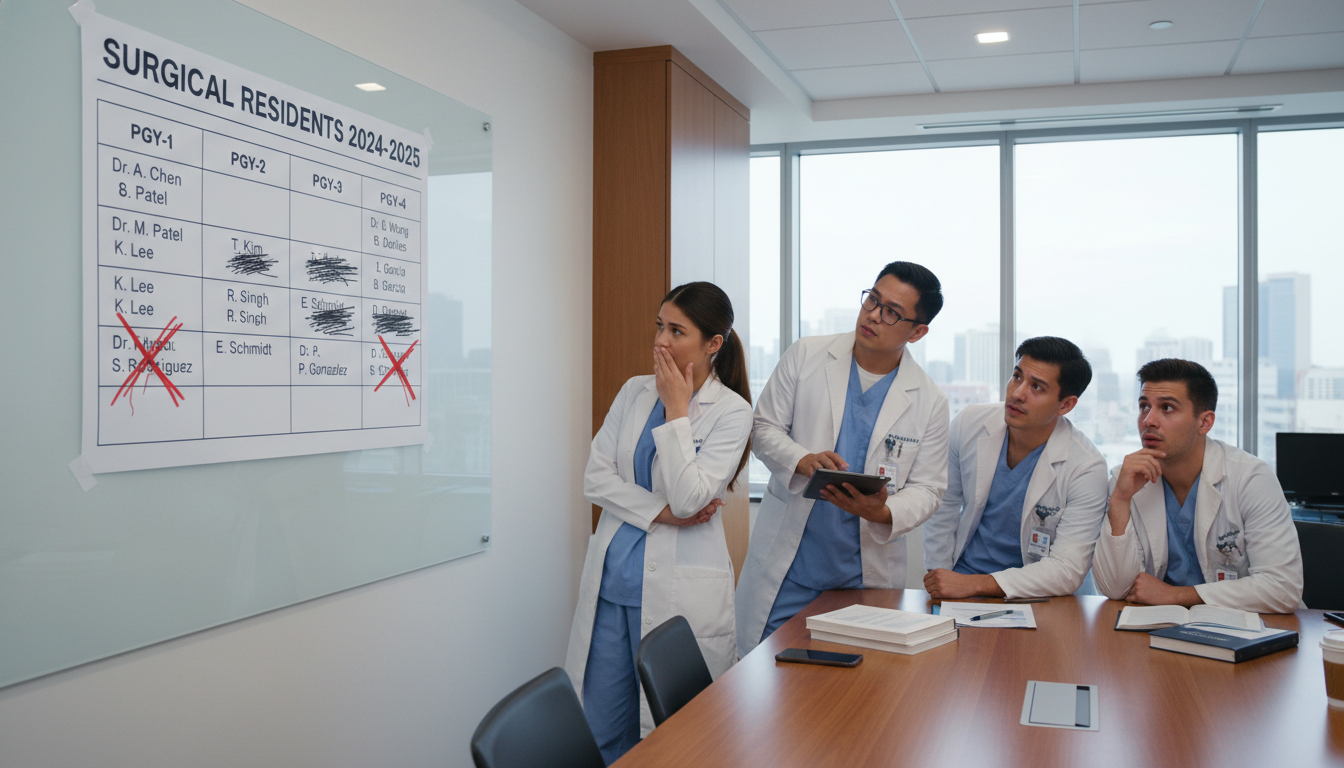
1. Frequent Mid-Year Departures or “Disappearing” Residents
Prelim residents sometimes leave surgery by choice—but multiple mid-year exits strongly suggest trouble.
Warning signs:
- You ask how many residents began the year and the number now is significantly lower
- Residents say things like, “We started with 7 prelims, but… we’re down to 4”
- The program director admits there were “a few transitions” but gives vague explanations
- Senior residents refer obliquely to people who “didn’t make it” without clarity
What this might indicate:
- Unsafe workload driving residents to leave
- Poor remediation process—failing residents rather than supporting them
- Toxic or hostile culture where people feel they have no choice but to resign
- Lack of transparency or poor communication from leadership
How to explore this diplomatically on interview day:
- “How many prelim surgery residents started last year and how many completed the year?”
- “Can you walk me through what happens if a resident is struggling—how do you support them?”
- Ask multiple levels: junior residents, chiefs, and PD/APDs. Inconsistent answers = red flag.
2. Repeated Non-Renewal of Preliminary Contracts
It is possible for a prelim not to be renewed—but if this is common, be cautious.
Warning signs:
- Residents tell you, “We usually lose a few prelims each year at contract renewal”
- Program leaders emphasize how “not everyone is cut out for this place”
- No clear, written criteria for renewal or promotion are offered
- Sudden changes in the number of PGY-2 prelim or categorical spots without explanation
Why this matters:
Your prelim surgery residency is short by design. You have limited time to prove yourself to future programs. A place where:
- Expectations are poorly defined
- Feedback is late or inconsistent
- Decisions are arbitrary
…can ruin your chances of moving forward—not because you lack ability, but because the environment is unstable.
Questions to ask:
- “In the last 3 years, roughly what proportion of preliminary surgery interns completed their full year?”
- “How often are prelim contracts not renewed, and what usually leads to that?”
- “Are there written criteria for successful completion of the prelim year that residents can review?”
If they dodge specifics, consider that a serious resident turnover red flag.
3. High Turnover Among Categorical Residents
Even though your focus is a preliminary surgery year, categorical residents are crucial to your experience.
Concerning signs:
- Multiple categorical residents have left or transferred in the last few years
- Third- or fourth-year classes are noticeably smaller than the PGY-1 class size
- Residents mention “a rough period” when “several seniors left”
- The program has had recent ACGME citations or probation related to resident complement or supervision
Why this is a bigger red flag than prelim turnover:
- Categorical residents have a long-term contract and strong incentive to stay
- When they leave, it usually reflects serious program problems:
- Unmanageable workload
- Chronic under-staffing
- Unprofessional leadership
- Safety concerns or lack of educational value
As a prelim, you are even less protected than categorical residents. If the people with long-term stakes are leaving, you should question how safe and sustainable the environment would be for you.
Questions to ask:
- “Have any categorical residents transferred out in the last few years? What have been the usual reasons?”
- “Has your resident complement changed recently? What led to those changes?”
You’re not judging a program for a single transfer; you’re watching for repeated patterns and evasive explanations.
4. Constantly Changing Program Structure or Resident Numbers
Some evolution is normal, especially with new leadership or changing service lines. But chronic instability is not.
Red flags:
- The number of prelim spots fluctuates widely year-to-year
- Rotations are repeatedly described as “in flux” or “being rebuilt”
- No one seems sure how many call nights, conferences, or rotations you’ll actually have
- Current residents say, “We’re still figuring things out” about core elements of the schedule
This can indicate:
- A program reacting to repeated residents leaving the program
- Persistent difficulty recruiting or retaining residents
- Inadequate planning, weak leadership, or unstable institutional support
For your prelim surgery residency, instability means:
- You may not get promised operative exposure
- You could be pulled into service-heavy, education-light roles to plug staffing holes
- Your letters, mentorship, or research may be disrupted by constant changes
Questions to ask:
- “Have there been major changes to the prelim program structure in the last 3–5 years? What drove those changes?”
- “Is the number of prelim positions stable from year to year?”
- “If other residents leave mid-year, how is workload redistributed?”
5. A Culture That Normalizes Burnout and Attrition
Sometimes turnover is almost worn as a badge of honor—this is especially dangerous.
Culture red flags related to turnover:
- Chiefs joke about “survival of the fittest” or “if you make it through intern year, you can do anything”
- Faculty or residents speak dismissively of those who left: “They just weren’t tough enough”
- No one mentions mental health resources, employee assistance programs, or structured wellness initiatives
- Asking about burnout gets you a shrug or a joke, rather than a clear answer
These attitudes are tightly linked to:
- Higher rates of residents leaving the program
- Underreported mental health crises and professionalism issues
- Lack of genuine support when you are struggling
In a prelim year where you are already under pressure to perform and position yourself for your next step, this is a serious warning.
Questions to ask plainly:
- “When residents are overwhelmed or burnt out, what real supports exist for them?”
- “How common is it for residents to take leave for health or personal reasons, and how is that handled?”
- “Would you feel comfortable telling your PD if you were struggling?”
Listen carefully to how residents answer, not just the content.
How to Recognize Turnover Red Flags Before and During Interviews

Pre-Interview Research: Reading Between the Lines
You can catch many turnover warning signs before you ever step on campus.
What to review:
Program website resident lists
- Compare current year vs archived versions (Wayback Machine or old PDFs)
- Look for:
- Residents who appear for 1 year then vanish
- Classes that shrink as you go up in PGY level
- Title changes like “research fellow” or “clinical fellow” where former residents are now cycling
Case logs and ACGME reports (if discussed publicly)
- Sudden drops in case volume per resident can drive people away
- Programs may quietly adjust resident numbers to compensate
Online forums and word-of-mouth
- Be cautious but attentive—repeated comments about residents leaving or toxic culture may have some truth
- Look for patterns, not single angry posts
Board pass rate and accreditation history
- Repeated board failures or recent ACGME concerns about resident well-being or supervision are red flags
- While these aren’t purely turnover metrics, they often correlate with deeper issues
Questions to Ask on Interview Day (with Sample Phrasing)
You need to gather information without sounding accusatory. Focus on curiosity and professionalism.
To program leadership (PD/APDs):
- “For the last few years, what proportion of prelims completed the full preliminary surgery year?”
- “How often have residents transferred out, and how do you support them when that happens?”
- “Have there been any recent changes in resident complement or structure? What led to those changes?”
- “If a resident is struggling clinically or personally, what does your support and remediation process look like?”
To junior residents (especially current prelims):
- “How many prelims started with you this year? Is everyone still here?”
- “How do you feel the program responds when residents are overwhelmed?”
- “Would you choose this prelim surgery residency again if you had to reapply?”
- “Have you seen residents leave mid-year? What happened with workload afterwards?”
To senior or chief residents:
- “Have you noticed changes in retention or turnover over the course of your training?”
- “What do you think keeps people here—and what leads some to leave?”
- “Do you feel leadership is honest and proactive when problems arise?”
Look for consistency across answers. Mixed or evasive responses usually signal underlying instability.
Observational Clues During Interview Day
Beyond answers to your questions, pay attention to:
- Body language when you ask about turnover
- Do residents exchange glances before answering?
- Does the room go tense or quiet?
- How residents talk about each other
- Are missing residents mentioned without context?
- Is there a sense of loss, or just indifference?
- Schedule and call discussions
- Are you hearing about frequent “extra calls” or “unexpected coverage” due to short staffing?
- Transparency of leadership
- Does the PD acknowledge past challenges and explain how they’ve been addressed?
- Or do they insist “everything is perfect here” despite other clues?
A solid program will be able to candidly acknowledge past rough patches while demonstrating concrete improvements and stable current function.
Putting It All Together: Interpreting Turnover in Context
Not all turnover is equal. You’re trying to distinguish between:
- Acceptable / understandable turnover
- Concerning patterns that indicate genuine program problems
When Turnover Might Be Less Concerning
Some scenarios are not automatically red flags:
- One resident left after discovering they truly wanted another specialty, and the program helped them transition
- A single prelim did not complete the year due to a major personal or health crisis, handled with compassion
- A few residents transferred years ago during a leadership transition that has since stabilized, with clear improvements described
In these cases, what matters is:
- Honesty – Are explanations consistent and plausible?
- Support – Did the program help the resident land on their feet?
- Trajectory – Are things clearly improving, with data to back that up?
When You Should Be Seriously Concerned
A pattern becomes a resident turnover red flag when you see:
- Multiple residents leaving mid-year over several classes
- Categorical residents departing or transferring repeatedly
- Vague, contradictory, or defensive explanations from leadership
- Residents who seem anxious or guarded when you ask about people who left
- Constant schedule changes, chronic short-staffing, or “emergency” coverage
For a preliminary surgery year, specific high-risk scenarios include:
- Programs that openly state, “Most prelims don’t make it to the end of the year”
- Places where prelims consistently carry disproportionate service work with minimal operative or educational benefit
- Programs with a reputation (locally or online) for “chewing up prelims and spitting them out”
- Institutions where prelims rarely match into categorical positions or advanced PGY-2/3 roles, despite strong individual performance
In these cases, even if the program is prestigious or high-volume, you should ask whether it will advance your long-term goals or merely consume a year of your life.
Strategic Takeaways for Applicants
- Prioritize stability over prestige. A solid, communicative mid-tier program with good support is often better than a famous name with chronic turnover.
- Protect your future self. You need:
- Reliable completion of your prelim year
- Strong letters of recommendation
- Enough clinical and operative experience to be competitive for the next step
- Document and compare. After interviews, write down:
- How many residents started vs remain (as reported)
- Any mention of transfers or non-renewals
- Your sense of transparency and culture
- Ask mentors for perspective. Share your impressions with trusted faculty who know these programs or their reputations.
You can’t eliminate all risk, but you can avoid the most obvious traps.
FAQs: Resident Turnover Warning Signs in Preliminary Surgery
1. Is any turnover acceptable, or should I avoid programs where anyone has left?
Some turnover is unavoidable and normal. People change career goals, develop health or family issues, or find that surgery truly isn’t for them. A single departure—especially with a clear, honest explanation—is not a reason to dismiss a program.
What you should avoid is repeated, poorly explained turnover and cultures that blame former residents or minimize their struggles.
2. How can I distinguish normal prelim year “churn” from true red flags?
Normal prelim “churn” looks like:
- Prelims completing the year and moving into their intended specialties or reapplying
- Programs clearly explaining where prelims went and celebrating their next steps
- Mostly stable numbers of residents from start to end of the academic year
True red flags look like:
- Several prelims not finishing the year
- Residents vanishing from rosters without explanation
- Defensive or vague answers when you ask about people who left
- A pattern over multiple years, not just one unusual class
3. Should I ask directly, “Have you had residents leave the program?”
Yes—but frame it professionally and open-ended. For example:
- “Over the last few years, have you had residents who decided to leave or transfer? How did the program support them through that process?”
This wording acknowledges that leaving can be a thoughtful decision and invites honesty about both the frequency and process.
4. What if a program seems otherwise great but I notice some concerning turnover?
Treat it as a yellow flag, not an automatic deal-breaker. Your next steps:
- Ask more targeted questions to PDs and residents.
- Look for patterns (over multiple years) rather than a single episode.
- Weigh the risk against potential benefits (case volume, reputation, mentorship).
- Discuss what you’ve learned with mentors who know your goals and risk tolerance.
If the program is transparent, shows evidence of improvement, and residents seem genuinely supported, it may still be a reasonable choice. If explanations feel evasive or dismissive, consider ranking it lower or not at all.
Resident turnover in preliminary surgery is not just a statistic—it is a vital indicator of how a program functions, treats its trainees, and responds to stress. By learning to recognize the resident turnover red flag patterns and asking direct, respectful questions, you greatly improve your chances of choosing a prelim surgery residency that will challenge you, support you, and prepare you for the next step in your surgical or specialty career.






















