
Understanding Resident Turnover in Psychiatry
Resident turnover is one of the most important—yet often under-discussed—indicators of a residency program’s health. For psychiatry residency applicants in particular, watching for signs of resident instability can help you avoid landing in a program with serious underlying problems.
In psychiatry, where wellness, supervision, and a stable training environment are crucial to developing into a competent and resilient clinician, high resident turnover can be especially concerning. When you hear phrases like “a couple of residents left last year” or “we’ve had some transitions,” your radar should go up—not necessarily to walk away immediately, but to start asking very focused questions.
This guide walks you through:
- Why resident turnover matters in psychiatry
- Specific warning signs to watch for during the psych match process
- How to interpret “residents leaving program” explanations
- What’s a normal transition vs. a resident turnover red flag
- How to ask residents and faculty about program problems without sounding confrontational
Throughout, the focus is on psychiatry residency programs—but most principles apply broadly to other specialties as well.
Why Resident Turnover Matters So Much in Psychiatry
Psychiatry training depends heavily on continuity: of supervision, therapy cases, team relationships, and institutional culture. Turnover disrupts all of this.
Impact on Training Quality
Lost teaching bandwidth
When residents leave a program, the remaining trainees often absorb extra call, more notes, additional admissions, and even informal teaching duties. Teaching conferences may be cut, clinics consolidated, or supervision diluted while the program “stabilizes.”Fragmented longitudinal experiences
Long-term psychotherapy clinics and continuity clinics are central to psychiatry residency. If residents in your cohort or above you leave:- Patient panels get redistributed abruptly
- Therapy cases may end prematurely
- Learning arcs get cut off
Fewer peer mentors
Stable, satisfied senior residents are key informal teachers in psychiatry. High turnover often means:- Fewer role models you’d actually want to emulate
- Less diverse supervision styles
- A culture of “survival mode” rather than growth
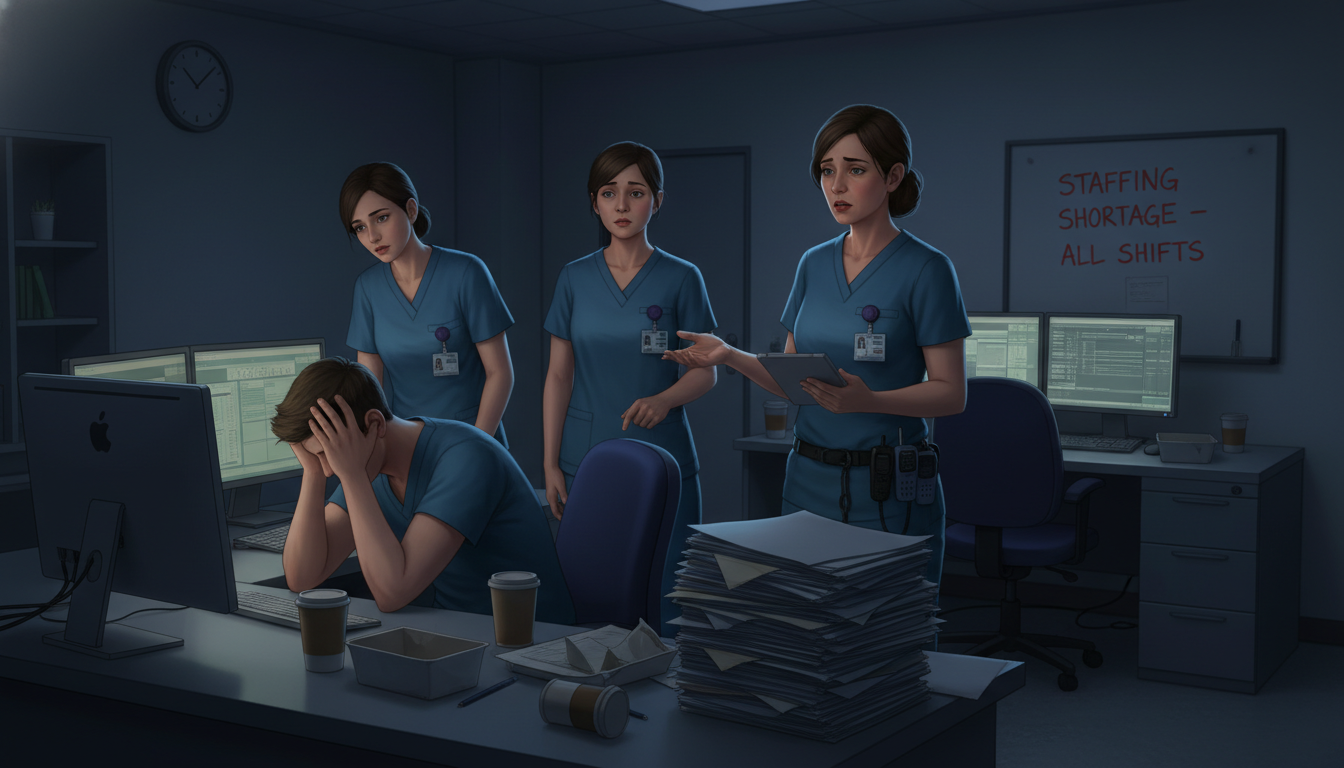
Impact on Resident Wellness and Culture
Psychiatry residency should model emotionally intelligent, compassionate workplaces. When multiple residents leave a program:
- It may signal chronic burnout, stigma around help-seeking, or punitive responses when trainees struggle.
- Remaining residents might adopt a “just get through it” mindset rather than thriving, learning, and enjoying the specialty.
- A culture of fear or silence can develop, especially if residents feel they must “keep the program’s image positive” for accreditation or recruitment.
Impact on Your Future Opportunities
Turnover doesn’t automatically mean you won’t get good training—but it may:
- Increase your risk of delays in graduation if schedules become chaotic
- Limit research or elective flexibility when staffing gaps must be filled
- Affect letters of recommendation if faculty are overextended or disengaged
- Create instability in clinical reputations of certain services, which can matter for early-career job referrals
In short: resident turnover is not just a statistic—it directly shapes your day-to-day life and long-term career development.
Normal vs. Concerning: Interpreting Resident Turnover in Psychiatry
Not all departures are a crisis. Some transitions are expected, healthy, or unrelated to program problems. The key is pattern recognition and context.
Examples of “Normal” or Low-Concern Turnover
A single resident leaving a psychiatry residency program can be understandable when:
Documented career change or specialty switch
- A PGY-1 leaves early to switch to neurology, family medicine, or internal medicine.
- Story is consistent across residents and faculty: “They realized they loved medicine more than psychiatry.”
Life events or personal reasons
- Family relocation (partner’s job, immigration issues, caregiving responsibilities).
- Medical leave followed by a decision not to return, with no suggestion of program conflict.
Pre-planned track changes
- Resident transfers to a research track or child & adolescent psychiatry fast-track at a different institution with strong support from current faculty.
In these scenarios:
- Other residents describe this as rare rather than frequent.
- Faculty and residents can openly explain what happened without tension.
- No one seems guarded or anxious when the topic comes up.
When Resident Turnover Becomes a Red Flag
Patterns that should trigger concern during the psych match process include:
Multiple residents leaving in a short span
- Example: 2–3 departures across PGY-1 to PGY-3 within 1–2 years.
- Frequent statements such as, “We’ve had some turnover recently, but things are improving,” without solid specifics.
Residents leaving at different training stages
- A PGY-1 leaves mid-year
- A PGY-3 transfers out
- A PGY-4 “takes a break” and doesn’t return
This suggests systemic, not just individual, issues.
Inconsistent or vague explanations
- “It wasn’t a good fit.”
- “They just had some personal stuff.”
- Different people give conflicting stories about the same departure.
Recent or ongoing probation or accreditation warnings
- Programs that have recently been on warning or citation for “duty hours” or “resident supervision” often show higher turnover.
Turnover especially concentrated among certain groups
- International medical graduates
- Residents of color or residents from underrepresented groups
- Residents who are parents or caregivers
This can hint at deeper issues related to inclusion, support, or discrimination.
Persistent unfilled spots
- A PGY-2 or PGY-3 position is open for months.
- They mention “we’re trying to backfill” repeatedly each year.
- NRMP or program website shows multiple off-cycle openings.
When these patterns line up, you may be seeing a resident turnover red flag that indicates serious program problems.
Specific Warning Signs to Watch for During the Psych Match Process
On interviews and second looks, your job is to gather data. Here are key warning signs related to resident turnover and program instability—and how they may show up in real time.
1. Strange Gaps in the Resident Roster
Actions to take:
- Before interviews, study the program’s resident list on their website.
- Note:
- How many residents per class?
- Are any classes smaller than others?
- Are there off-cycle entries (e.g., PGY-3 who started late)?
Red flags:
- A PGY-2 or PGY-3 class with fewer residents than advertised.
- Residents whose bios explicitly mention “previous residency training in X” without a clear path.
- A pattern where the program used to have, say, 8 residents per year but now has 5–6.
Interpretation:
- This may signal residents leaving program mid-training or unfilled spots due to reputation issues.
Questions to ask:
- “I noticed your PGY-2 class is smaller—was that by design, or did the class change over time?”
- “Has your class size changed in the last few years? What led to that?”
2. Resident Body Language When Turnover Is Mentioned
You will often get more truth from nonverbal cues than from words.
What to watch for:
- Awkward silence or glances between residents when someone asks about why a resident left.
- Rapid subject changes or joking deflections (“Oh yeah, that was… a thing.”).
- Residents sharing very different stories from faculty.
Example scenario:
- Applicant: “What happens if someone is struggling in the program or thinking about leaving?”
- Senior resident: “Um… We definitely have support resources. Anyway, the call schedule is pretty reasonable.”
Interpretation:
- The discomfort may signal fear of retaliation, poor program responsiveness, or unresolved conflict.
3. Overly Defensive or Polished Responses about Program Problems
Healthy programs acknowledge challenges honestly.
Potential concern:
- Every answer about prior residents leaving sounds like a rehearsed talking point:
- “They had personal reasons, and we fully supported them. We’re better than ever now.”
- “That was all due to one difficult personality; we’ve fixed that.”
Things to probe:
- “Can you share how the program changed things after that situation?”
- “What did the program learn from that experience with residents leaving?”
If they can’t identify concrete changes—e.g., new mentorship structures, adjusted rotations, or added wellness resources—it may just be damage control.
4. Chronic Schedule Instability or Last-Minute Changes
High turnover often manifests as chaotic scheduling.
Signs on interview day or second look:
- Residents mention frequent last-minute schedule shifts “because coverage changed.”
- Multiple comments like:
- “We just found out we’re moving to another unit next month.”
- “We sometimes find out our rotations pretty late.”
Common hidden causes:
- Residents leaving mid-year
- Over-reliance on a small pool of residents to cover essential rotations
- Poor administrative support
Ask directly:
- “How far in advance do you know your schedule for the year?”
- “Has resident turnover ever impacted your call schedule or rotation planning?”
5. Overloaded or Burned-Out Senior Residents
Resident turnover downstream often shows up as PGY-3 and PGY-4 residents who appear exhausted or detached.
Possible signs:
- Seniors express that they are constantly covering for someone:
- “We’ve had to pick up extra calls because of some transitions.”
- “We’re stretched pretty thin on night float.”
- Little enthusiasm about the program:
- Compliments are lukewarm and generic
- They emphasize “it’s doable” instead of “I’m really growing here”
Follow-up questions:
- “Has resident turnover ever affected your ability to get therapy cases or electives you wanted?”
- “If someone leaves the program, how does the program protect the remaining residents from burnout?”
6. Hidden or Downplayed Program Problems
Psychiatry residency applicants should also listen for what isn’t said.
Potential subtle warning signs:
- Very little detail about therapy training or supervision despite psychiatry’s psychotherapeutic core.
- Evasive responses around:
- Duty-hour violations
- Supervision availability overnight
- Trainee involvement in high-risk cases
Connection to turnover:
- Programs with chronic overwork, limited supervision, or emotional toxicity often see residents leave, especially in psychiatry where self-awareness and boundaries are essential.

How to Ask About Resident Turnover Tactfully
It’s possible—and wise—to ask direct questions about resident turnover without sounding accusatory. In the psych match process, your job is to assess mutual fit, not just to impress.
General Principles
- Aim for curiosity, not confrontation.
- Ask about process, not individuals.
- Use open-ended questions that invite detail.
- Compare answers across multiple residents and faculty.
Sample Questions to Ask Residents
About overall stability
- “How stable has your resident class been since you started?”
- “Have many people left or transferred during your time here?”
About what happens when people struggle
- “Have there been residents who struggled here? How did the program support them?”
- “Do you feel comfortable speaking up if a rotation is unsustainable?”
About real experiences with turnover
- “If someone does leave the program, what usually happens to the workload or call for everyone else?”
- “Has resident turnover ever impacted your education or wellness?”
Conceptual tip: The actual words matter less than how comfortable and consistent the residents’ answers seem.
Sample Questions to Ask Faculty or Program Leadership
Framed as interest in mentorship and support
- “What structures are in place to support residents who are having difficulty—academically, clinically, or personally?”
- “How has the program learned from residents who have left or transferred in the past?”
Framed as curiosity about program evolution
- “How has your residency program changed over the last 5–7 years? Were those changes shaped by resident feedback or challenges?”
- “What have been your biggest growing pains as a program, and how did you address them?”
Red-flag leadership responses:
- Blaming residents entirely (“We just had a couple of people who weren’t cut out for this”).
- Refusal to acknowledge any program-level learning from past difficulties.
Decision-Making: When Resident Turnover Should Change Your Rank List
You will likely encounter at least one program where “residents leaving program” has clearly been an issue. The decision isn’t always binary—stay or walk away—but you should integrate this data thoughtfully into your psych match strategy.
When Turnover Is a Mild Concern but Not a Deal-Breaker
You might consider still ranking the program if:
- There was one cluster of departures during a major external stressor (e.g., COVID-19 surges, hospital merger), and both residents and leadership can clearly describe the steps they took afterward.
- Remaining residents appear well-supported, honest, and hopeful about program direction.
- Concrete improvements are evident:
- More faculty hires
- Reduced call or improved schedules
- Clear wellness initiatives with protected time
In this case, you might:
- Rank the program, but lower than similarly strong, more stable options.
- Consider your own risk tolerance and need for a predictable environment.
When Turnover Should Strongly Lower a Program on Your List
You should be very cautious when:
- Multiple classes show clear shrinkage or off-cycle residents.
- Stories about why residents left are vague, inconsistent, or secretive.
- Residents seem anxious, guarded, or exhausted when speaking about the program.
- Faculty responses are defensive, dismissive, or blame-heavy.
In psychiatry, training in a chronically unstable or emotionally toxic environment can:
- Shape how you handle countertransference, boundary issues, and team conflict.
- Put you at higher risk for burnout and compassion fatigue.
- Complicate your own mental health, especially if you already manage depression, anxiety, or trauma.
For most applicants, such a program should move significantly down or off your rank list, especially if you have other viable options.
Balancing Prestige vs. Stability
A common dilemma:
“This is a well-known academic psychiatry residency with great research but clear turnover issues. Should I still rank it highly?”
Consider:
- In psychiatry, your clinical competence, emotional resilience, and professional network often matter more than the brand name alone.
- A mid-tier but supportive, stable program can produce excellent psychiatrists who match into competitive fellowships and leadership roles.
- No prestige is worth a training environment that erodes your well-being or professional identity.
When in doubt, talk to:
- Trusted mentors who know you personally.
- Residents or alumni at that program who have recently graduated (not only those currently there).
- Advisors who understand the nuances of psychiatry training.
FAQs: Resident Turnover and Red Flags in Psychiatry Residency
1. Is any resident turnover automatically a red flag?
No. Some turnover is expected in every specialty, including psychiatry. Single, clearly explained departures for personal reasons, medical issues, or thoughtful career changes are not inherently concerning. Focus on patterns (multiple classes, recurring themes, secrecy, blame) rather than any individual case.
2. How can I verify what I hear on interview day?
You can:
- Check the program’s website for changes in class size over time.
- Look at NRMP and program announcements for off-cycle or backfill positions.
- Reach out (tactfully) to recent alumni via email or professional networks to ask about their experiences.
- Compare what multiple residents, faculty, and coordinators say independently—consistency is key.
3. What if a program with some turnover is my only realistic psych match option?
If your application profile limits your options, you may decide to rank a program with known turnover. In that case:
- Go in eyes open about potential stressors.
- Identify early:
- Mentors and allies among faculty
- Wellness resources (therapy, coaching, peer support)
- Boundaries around work hours and non-clinical tasks
- Reassess periodically whether the program truly supports your growth. Transfer is difficult but not impossible if needed.
4. Is high resident turnover always due to program problems?
Not always, but often there is at least some program-level contribution. External circumstances (pandemic, family crises, geographic shifts) do play a role. However, if multiple residents repeatedly decide they are better off leaving than staying, it’s rarely only about individual circumstances. Healthy programs examine these events critically and implement meaningful changes.
Recognizing resident turnover warning signs in psychiatry is not about paranoia—it’s about making an informed, self-respecting choice. You are training to become a physician who understands systems, patterns, and human behavior. Apply those same skills to evaluating programs during the psych match process, and you’ll be far more likely to land where you can truly grow into the psychiatrist you hope to become.






















