
Why Resident Turnover Matters So Much in Vascular Surgery
Resident turnover is more than a minor inconvenience—it is one of the most telling indicators of deeper program problems. For a DO graduate pursuing a vascular surgery residency or integrated vascular program, understanding resident turnover red flags can protect your training, board eligibility, and long‑term career.
Vascular surgery is a small, high‑intensity specialty. Each resident’s presence (or absence) significantly affects case volume, call burden, and culture. When residents are leaving the program, you need to understand why—and whether those reasons could harm your experience.
In this article, we’ll focus on:
- How to interpret resident turnover in vascular surgery programs
- Specific warning signs to watch for as a DO graduate
- How to ask the right questions on interview day
- What’s normal vs. truly worrisome resident turnover
- Concrete strategies if you suspect a program has serious issues
The goal is to help you tactically and confidently evaluate osteopathic residency match options in vascular surgery—so you don’t discover major problems after you’ve already committed.
Understanding Resident Turnover in Vascular Surgery Programs
Resident turnover refers to residents who leave the program before graduation, including:
- Transfers to another vascular surgery residency
- Switching specialties
- Dismissals or non‑renewal of contracts
- Residents taking extended leaves and not returning
In a vascular surgery residency or integrated vascular program, turnover is particularly impactful because:
- Cohorts are small (often 1–3 per year)
- Call and case coverage rely on every slot being filled
- Subspecialty skills require continuity of training and mentorship
Losing even one resident can:
- Double the call burden for others
- Reduce individual case volumes
- Shift rotations or delay operative autonomy
- Increase stress and burnout for remaining residents
Normal vs. Concerning Turnover
Not all turnover is a resident turnover red flag. You should distinguish between isolated, explained events and patterns that suggest systemic program problems.
Potentially normal or understandable scenarios:
- One resident in 10 years changed to another specialty for personal reasons
- A transfer after a family relocation or spouse’s job move
- A resident taking a year off for research and returning
- A resident with documented health or personal issues leaving training
Concerning patterns:
- Multiple residents leaving the same year or in close succession
- Vacant or “frozen” positions not being filled year after year
- A history of dismissals or non‑renewed contracts with vague explanations
- Residents leaving without clear information from the program
Your goal as a DO graduate entering the osteopathic residency match or NRMP is to interpret what the turnover means about program culture, support, and stability.
Major Resident Turnover Red Flags in Vascular Surgery
Below are specific warning signs tied to resident turnover that you should look for when evaluating any vascular surgery residency or integrated vascular program.
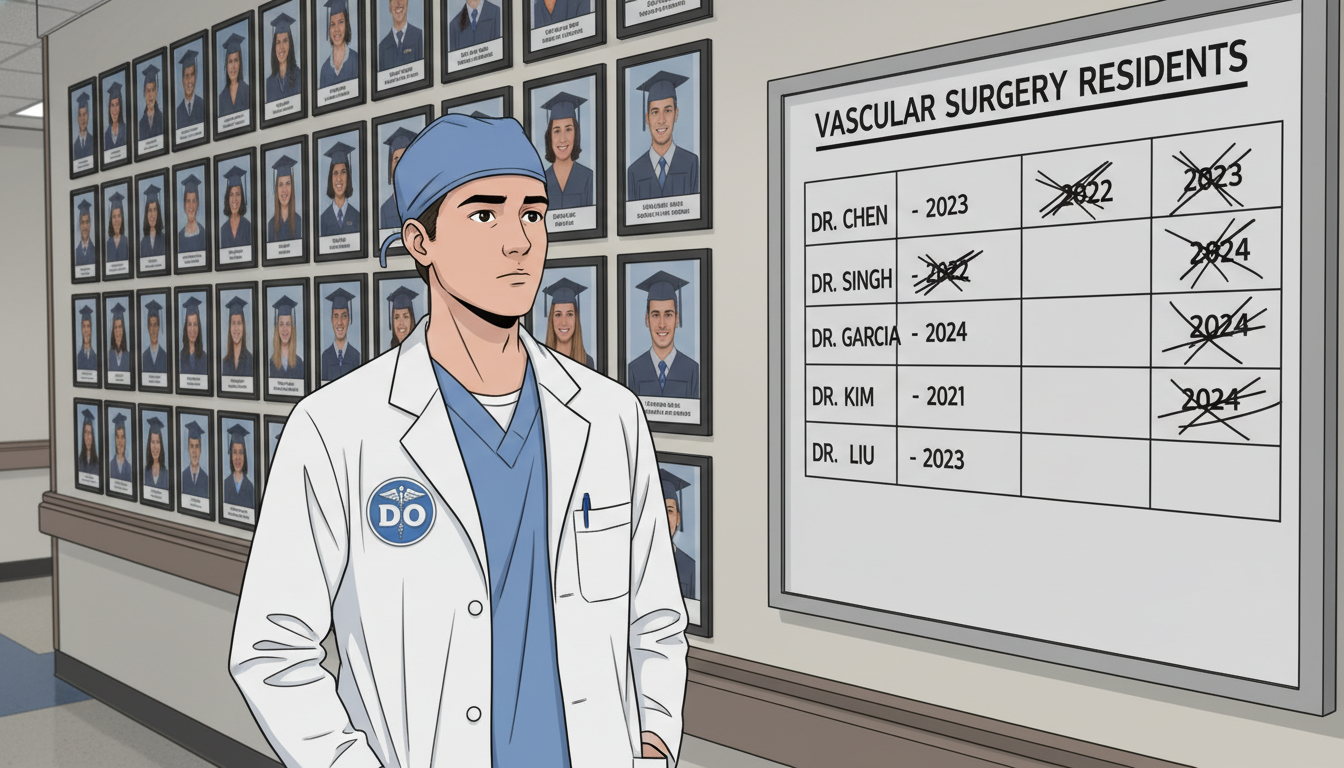
1. Repeated Gaps in Resident Classes
In a stable 5+2 or integrated 0+5 vascular surgery residency, you should see relatively consistent numbers of residents per year.
Red flags:
- One or more PGY years with unfilled or “missing” residents
- Faculty casually saying, “We only have one PGY‑3 this year; the other one left” without explanation
- A long history of staggered class sizes not explained by program expansion/contraction
Why it matters:
- Gaps often mean residents left due to dissatisfaction, culture issues, or unsupportive leadership
- Fewer residents per class can lead to heavier workload, decreased time for conferences, and more frequent call
- It can signal a program with limited applicant interest or a damaged reputation
Questions to ask:
- “Have there been any residents leaving the program in the last 5–7 years? What were the circumstances?”
- “I noticed the current PGY‑3 class has only one resident. Was that intentional or the result of a change?”
A transparent program will give concrete, straightforward explanations (e.g., “A resident left for family relocation; we chose not to backfill that year.”). Evasive or vague answers are a strong warning sign.
2. Frequent Transfers or Residents Switching Specialties
In vascular surgery, transferring out is more complex than in some other fields. It often reflects serious dissatisfaction or mismatch between resident and program.
Concerning signs:
- Multiple residents in recent years transferring to general surgery, cardiology, or other fields
- Faculty or residents casually saying, “We’ve had several people realize vascular wasn’t for them”
- An institutional pattern of residents leaving vascular while other specialties remain stable
Why it matters:
- High transfer rates suggest poor mentorship, unrealistic expectations, or toxic culture
- It may indicate inadequate pre‑recruitment screening or dishonest portrayal of the program during interviews
- You could be entering an environment where burnout and regret are common
As a DO graduate, you should also consider whether osteopathic residents are disproportionately leaving compared with MD counterparts. That can indicate subtle or overt bias, lack of support for DOs, or limited opportunities for osteopathic graduates.
Questions to ask residents:
- “Have any residents transferred out recently? What led to those decisions?”
- “How often do residents decide vascular isn’t for them and leave?”
- “Do DO graduates here tend to have similar outcomes and support compared to MDs?”
Listen both to what they say—and what they avoid saying.
3. Non‑Renewal of Resident Contracts or Dismissals
Dismissals or non‑renewed contracts are sometimes necessary, but when they happen repeatedly, they are a major resident turnover red flag.
What to watch for:
- Hints that residents were “asked to leave,” “did not advance,” or “didn’t get their contract renewed”
- Stories that emphasize punishment over remediation
- A culture of fear around evaluations and clinical competency committees
Why it matters:
- A punitive environment can make learning unsafe and discourage seeking help
- Residents may hide mistakes rather than disclose them, which is dangerous in a high‑stakes field like vascular surgery
- You may feel constantly at risk, especially as a DO graduate who might already feel pressure to “prove” your worth
Questions to explore:
- “How does your program handle residents who struggle technically or academically?”
- “Can you describe the remediation process here?”
- “Have there been any dismissals in the past several years? What support was offered before that point?”
Be cautious of answers like:
- “We have high standards. If you can’t keep up, this isn’t the place for you.”
- “We don’t really do remediation—people either make it or they don’t.”
This philosophy is particularly risky in a small, high‑acuity specialty.
4. Silent or Evasive Explanations for Residents Leaving Program
Sometimes what’s most telling isn’t turnover itself, but how the program talks about it.
Red flags in communication:
- Evasive answers: “Things just didn’t work out,” “Personal issues,” repeated without detail
- Faculty and residents giving different versions of why someone left
- A visible discomfort or “we’re not supposed to talk about that” reaction
Why it matters:
- Lack of transparency typically means there’s something negative the program doesn’t want to expose
- It may reflect poor psychological safety and a culture that avoids honest feedback or self‑reflection
- Programs that can’t openly acknowledge past issues are less likely to have truly improved
You’re not asking for confidential personal details, but you are entitled to understand if residents leaving program was due to systemic problems like:
- Chronic overwork and unsafe workloads
- Unaddressed bullying or harassment
- Lack of operative exposure
- Major conflicts between residents and leadership
Healthy programs can say something like:
“We had a resident leave 3 years ago due to conflicts with leadership and concerns about workload. We did an internal review, changed call schedules, and now have a wellness committee and formal grievance process.”
5. High Resident Turnover Plus Negative Culture Signals
Turnover is rarely isolated. Combine it with other clear signs of trouble, and you may be seeing a truly toxic environment.
Watch for these combined patterns:
- High turnover + resident burnout: Residents look exhausted, speak cynically, or warn you indirectly
- Turnover + lack of faculty engagement: Few mentors, little career guidance, minimal teaching in the OR
- Turnover + poor case distribution: Complaints that junior residents don’t get cases because fellows or seniors take them all
- Turnover + chaotic scheduling: Constant last‑minute call changes due to missing residents
For a DO graduate, there’s an additional layer:
- Is there a pattern of DO residents leaving while MDs remain?
- Do DOs receive fewer complex cases, leadership roles, or research opportunities?
- Has the program only recently begun accepting DO applicants, and is still figuring out how to support them?
If your osteopathic residency match choices include programs with such patterns, weigh them very carefully against more stable options, even if the unstable program is at a “big‑name” institution.

How to Detect Turnover Problems During Interviews and Rotations
You will rarely see “resident turnover” openly discussed on a website. You have to actively observe and ask questions.
1. Use Away Rotations Strategically
If you rotate at a vascular surgery residency, treat it as both an audition and a reconnaissance mission.
What to observe:
- Are there fewer residents than expected on the schedule?
- Do people mention “we’re short because…” and then trail off?
- Is call coverage consistently chaotic or overloaded?
- Do residents seem fearful of leadership or openly complain about the program?
Ask residents privately (ideally one‑on‑one):
- “Have many people left the program early?”
- “If you could choose again, would you still come here?”
- “How honest was the program about lifestyle and culture during your interview?”
As an osteopathic graduate, you might also add:
- “Have previous DO residents here generally finished successfully?”
- “Are DO residents treated any differently—in subtle ways—than MDs?”
2. Ask Direct but Professional Questions on Interview Day
You can absolutely ask about turnover—just phrase it professionally.
To program leadership:
- “Could you walk me through your resident graduation history over the last 5–7 years? Have most residents completed the program?”
- “Have there been residents who left the program early, and how did the program respond or adapt?”
- “How does the program monitor burnout and resident satisfaction?”
To current residents:
- “Has anyone in your cohort or recent classes transferred or left?”
- “How transparent is leadership when there are problems?”
- “What changes has the program made in response to resident feedback?”
Pay attention to their tone, pauses, and consistency. If multiple people seem uneasy discussing the past, that itself is information.
3. Review Public Data Where Available
Though data can be limited, some sources provide clues:
- Program websites: Check resident alumni/graduation lists
- FREIDA / ERAS / NRMP reports: Look for major changes in positions offered over time
- Word of mouth: Speak with senior residents or fellows in vascular or general surgery at your home institution
Pattern to note:
- A program that used to have 3 residents per year suddenly listing only 1 or skipping an entire class
- Recent rapid reduction in integrated vascular program size with no clear explanation
All of these warrant follow‑up questions.
Interpreting Turnover as a DO Graduate: Risk‑Benefit Decisions
As a DO graduate looking at an osteopathic residency match or categorical vascular surgery residency, you’ll have to make trade‑offs. Some programs with minor turnover may still be outstanding training environments. Others with repeated residents leaving program are not worth the risk, even if they appear prestigious.
When Turnover Might Be Acceptable
Turnover may be tolerable if:
- It’s infrequent and clearly explained (e.g., a single resident with family relocation)
- The program has a clear, documented response (schedule adjustments, wellness initiatives, stronger mentorship)
- Remaining residents sound genuinely supported and satisfied
- There is strong DO representation with good outcomes (board pass rates, fellowships, jobs)
In such programs, you may still receive excellent operative experience and mentorship.
When Turnover Should Be a Hard Stop
Strongly consider ranking other options higher if you see:
- Multiple residents leaving program in recent years with vague explanations
- Significant resident turnover red flag patterns combined with visible burnout, fear, or cynicism
- A track record of DO graduates struggling, transferring, or failing to complete
- Leadership who dismiss concerns or emphasize “survival of the fittest” over education
In vascular surgery, your early training is foundational. Choosing a program with clear, unresolved program problems can:
- Limit your case experience and operative autonomy
- Increase your risk of burnout or mental health crises
- Put your board eligibility or completion at risk
Your long‑term career is far more important than chasing prestige or name recognition.
Action Plan: What to Do If You Suspect a Problem
If you think a vascular surgery residency or integrated vascular program has serious turnover issues, here’s a stepwise approach:
Clarify the Facts
- Ask direct questions of multiple people (faculty, junior and senior residents).
- Look for patterns and consistency in their answers.
Seek Outside Perspectives
- Talk to general surgery residents, fellows, or attendings at the same institution—they often know the vascular program’s reputation.
- Consult mentors at your home institution or DO advisors who know national program reputations.
Weigh Against Other Programs
- Create a simple table: case volume, culture, stability, DO‑friendliness, location, and turnover history.
- Notice whether one or two factors (like location) are tempting you to overlook major red flags.
Prioritize Safety and Education
- Rank safer, stable programs higher—even if they’re “less famous.”
- Remember: strong operative training, supportive culture, and high completion rates matter more for your future than brand name.
Protect Your Own Well‑Being
- Recognize that even highly resilient residents can be worn down by a dysfunctional environment.
- You’re not “weak” for avoiding a program known for residents leaving and high turnover; you’re being strategically wise.
FAQs: Resident Turnover Warning Signs for DO Graduates in Vascular Surgery
1. As a DO graduate, should I be more cautious about programs with turnover than an MD applicant?
Yes. DO graduates can face additional hurdles, including implicit bias and fewer mentorship networks in some academic centers. If a vascular surgery program already has resident turnover problems, a DO resident may be at higher risk of being under‑supported or unfairly blamed when systemic issues arise. You should especially look for:
- Prior successful DO graduates from the same program
- Faculty who explicitly welcome osteopathic training and board eligibility
- Clear, objective evaluation systems rather than vague or subjective metrics
If a program has high turnover and limited experience training DOs, consider that a significant risk factor.
2. How much resident turnover is “too much” in a vascular surgery residency?
There’s no strict numeric cutoff, but in a small specialty like vascular surgery:
- Multiple residents leaving within 5 years is already concerning
- Any pattern of more than one resident per small cohort (1–3 residents/year) leaving is a serious warning
- Repeated vacancies or missing classes without transparent explanations should be viewed as a major red flag
It’s the pattern plus lack of transparency that should worry you most.
3. If a program admits it had high turnover but says it has “fixed” things, should I still be worried?
Not necessarily—but you should verify:
- Have changes been implemented and sustained, not just promised?
- Do current residents describe meaningful improvements (better schedules, more faculty, wellness initiatives)?
- Has turnover actually decreased in the last 2–3 classes?
Ask for examples: “What specific structural changes were made after those residents left?” Programs that openly acknowledge and clearly fix problems can become excellent training environments—but blind trust isn’t enough; look for evidence.
4. What should I do if I only notice turnover concerns after I’ve already matched?
If you discover resident turnover red flags once you’ve matched:
- Gather information carefully—talk to senior residents and mentors.
- Engage early with program leadership about expectations and supports.
- Develop a personal support plan: mentors, mental health resources, family/friend network.
- If problems are severe and persistent, discuss options with your GME office, trusted advisors, or national organizations—transfers are rare but possible.
Your priority is to protect your training, health, and professionalism. Early, proactive communication and strong mentorship are critical.
By learning to recognize resident turnover red flags—and understanding their implications specifically within vascular surgery—you put yourself in a much stronger position to choose a program where you can thrive. As a DO graduate, you bring valuable skills and perspective to any integrated vascular program or categorical training track. Your task now is to ensure that the program you join is equally committed to supporting you all the way to graduation.






















