 and research options Premed students comparing [clinical volunteering](https://residencyadvisor.com/resources/clinical-volunteering/mcat-score-gpa](https://cdn.residencyadvisor.com/images/articles_v3/v3_CLINICAL_VOLUNTEERING_clinical_volunteering_vs_research_what_acceptance_-step1-premed-students-comparing-clinical-volun-5363.png)
The common belief that “more research equals higher med school acceptance” is statistically overstated—and clinical experience is often the more decisive differentiator.
The data from AAMC, MSAR profiles, and published admissions reports show a consistent pattern:
Strong applicants tend to have both research and clinical exposure, but when schools must choose between them, documented and sustained clinical engagement usually tracks more closely with interview and acceptance rates.
(See also: Hospital vs Community Clinic Volunteering: A Data-Driven Comparison for more insights.)
1. What the Numbers Actually Say
Most premeds ask the wrong question: “Is research more important than clinical volunteering?”
The more accurate, data-driven question is: “Among applicants with similar metrics, which pattern of experiences aligns with higher acceptance rates?”
Let us start with broad AAMC data trends (U.S. allopathic MD programs):
From recent AAMC “FACTS” tables (aggregated patterns from multiple cycles):
- Average accepted MD applicant:
- GPA: ~3.7–3.8
- MCAT: ~511–513
- Clinical experience: usually 100–300+ hours (often a mix of volunteering, shadowing, and paid clinical work)
- Research: 60–800+ hours, but with very wide variance
Compare that with the full applicant pool:
- Many rejected applicants have:
- Comparable or slightly lower GPA/MCAT
- Some research listed (especially at research universities)
- Sparse or fragmented clinical exposure (e.g., <50–75 hours, irregular, or late)
Admissions deans repeatedly emphasize in public forums and webinars:
“We do not admit future scientists. We admit future physicians. Research is valuable, but clinical experience is non-negotiable for most applicants.”
That statement is not just rhetoric—it is consistent with acceptance patterns when you look at applicant profiles on MSAR and self-reported data across hundreds of students.
A simple comparison pattern
Consider two simplified applicant profiles, controlling for GPA/MCAT:
- Applicant A: Heavy research, light clinical
- 1,000 research hours, 1 poster, 1 publication
- 30 shadowing hours, 20 clinical volunteering hours
- Applicant B: Heavy clinical, moderate research
- 400 clinical volunteering hours, 100 shadowing hours
- 200 research hours, no publications
Across real-world outcomes (from student-reported admissions data, school prehealth office summaries, and advisor surveys):
- Applicant A often performs better at:
- Top 10–20 research-intensive MD programs (e.g., Hopkins, UCSF, Penn, WashU), if the research is high-impact and the rest of the application is outstanding.
- Applicant B more consistently secures:
- Interviews and acceptances across a wider range of MD programs, including mid-tier and many state schools.
The acceptance-rate advantage at the population level skews toward the balanced but clinically strong profile, not the “research-heavy, clinically thin” profile.
2. Dissecting AAMC and School-Specific Data
AAMC does not publish a simple “acceptance rate vs hours” table for clinical and research, but several consistent patterns emerge when you triangulate:
- MSAR school profiles
- Publicly shared class profiles
- Prehealth office aggregate data
- National survey data (e.g., Matriculating Student Questionnaire highlights)
Clinical exposure as a “threshold” variable
Across dozens of schools:
- Shadowing:
- Typical range for matriculants: ~40–120 hours
- Below ~20–30 total hours, interview rates drop sharply unless compensated by substantial other clinical (scribing, EMT, MA, hospital volunteering).
- Clinical volunteering / paid clinical work:
- Many matriculants cluster around 100–300+ hours.
- Applicants with zero or minimal patient-facing experience are rarely admitted, even with strong metrics.
This suggests a threshold effect: once a minimal to solid level of clinical experience is reached, incremental hours produce diminishing returns, but falling below that threshold is strongly associated with lower acceptance rates.
Research as a “signal quality” variable
Research behaves differently in the data:
- Presence of research:
- Among applicants with GPA ≥3.7 and MCAT ≥510, those with some research are overrepresented in matriculant pools at research-heavy MD programs.
- Intensity and impact:
- Substantial research (≥500 hours, poster/presentation, strong PI letter) correlates with:
- Higher odds at top 20 MD programs
- Better chances at MD/PhD and research track programs
- But outside of very research-intensive environments, large differences in research hours (e.g., 300 vs 900) do not consistently produce proportional differences in acceptance rates.
- Substantial research (≥500 hours, poster/presentation, strong PI letter) correlates with:
In other words, having meaningful research matters for certain tiers and program types, but obsessive hour accumulation above a moderate threshold has sharply diminishing returns.
Institutional acceptance patterns
Data from several large universities’ prehealth offices (shared in advising reports and info sessions) show a repeating pattern over multiple cycles:
Students with:
- GPA ≥3.5
- MCAT ≥510
- 150–250+ hours of clinical exposure
- 100–400 research hours
→ Higher overall acceptance rates (often 60–80%+ depending on school selectivity).
Students with:
- Similar GPA/MCAT
500–1,000 research hours
- <50 clinical hours
→ Noticeably lower acceptance rates, often 20–40% lower, and highly concentrated in rejections from community-oriented schools.
The statistical takeaway: clinical experience appears more strongly predictive of broad-based acceptance than research volume, once we control for academic metrics.
3. Different School Types, Different Weighting
Not all medical schools weight these activities equally. The real question is: which schools are you targeting and what does their applicant pool look like?
Research-heavy MD programs (top 20–30)
Programs like UCSF, Harvard, Penn, Columbia, and Stanford publish high rates of matriculants with research backgrounds. Internal and advisor-collected data show:
- A large majority of matriculants have:
- 1+ substantial research experiences
- Evidence of scholarly output (posters, abstracts, sometimes publications)
- However, virtually all also have:
- Solid to strong clinical exposure
- Clear demonstration of patient-centered motivation
At these schools:
- No research = serious handicap
- No clinical = near automatic disqualification
- Strong both = highest acceptance probability
Research here is not a “nice bonus”—it is a core part of the profile—but clinical is still a gating factor.
Broad MD schools, including many state programs
Schools with a strong emphasis on primary care, community engagement, and their in-state pipeline (e.g., many state MD schools) often signal in their mission statements and info sessions:
- Heavy weight on:
- Clinical volunteering
- Service to underserved populations
- Longitudinal commitment in patient-facing roles
- Research:
- Valued, but not mandatory
- Often less predictive of acceptance than consistent clinical and service
Admissions trends from these schools’ public Q&A sessions repeat the same theme: a modest research record is fine; lack of real patient exposure is a problem.
DO schools
For osteopathic schools, aggregate applicant narratives and advisor data show:
- Clinical experience is often even more central:
- Scribing, MA work, CNA, EMT, hospice, or long-term hospital volunteering are heavily represented.
- Research:
- Common, but usually not a primary selection lever unless you target specific DO programs with research missions.
The net effect: In acceptance-rate terms, clinical gaps hurt you more than limited research at a large proportion of DO schools.

4. How Much Is “Enough”? Quantitative Benchmarks
Applicants want numbers, even though admissions is holistic. Based on combined trends from AAMC data, MSAR, school reports, and advising experience, these are reasonable data-informed ranges for competitive MD applicants (not guarantees, but statistically safer zones):
Clinical experience (volunteering + paid)
For applicants targeting a broad mix of MD schools:
- Shadowing:
- Baseline: 40–60 hours total
- Competitive: 60–120 hours, across at least 2–3 specialties with some primary care exposure.
- Hands-on clinical volunteering or paid work:
- Baseline for being taken seriously: ~80–100 hours
- Safer, more typical range for matriculants: 150–300+ hours
- Highly competitive for service-focused schools: 300–500+ hours, especially if longitudinal at the same site.
Incrementally, an extra 500 hours on top of 300 is not linearly better, but going from 0 → 100 → 250 clinical hours is associated with a meaningful shift from risky → reasonable → solid.
Research
For MD applicants not focused on MD/PhD or top 10 programs:
- Baseline:
- 100–200 hours of structured lab or clinical research under supervision.
- Comfortable range:
- 200–400 hours with:
- Clearly defined project
- Specific role
- Tangible outcome (poster, data analysis, presentation, strong PI letter).
- 200–400 hours with:
For highly research-intensive MD or MD/PhD:
- More common:
- 500–1,500 hours over multiple years
- 1–2 posters, abstracts, or publications
- Project ownership or clear intellectual contribution
However, acceptance data do not show that every applicant at top schools has a publication. Many have robust research commitment but no paper yet; the narrative and depth of involvement matter more than raw hours alone.
When the two conflict due to limited time
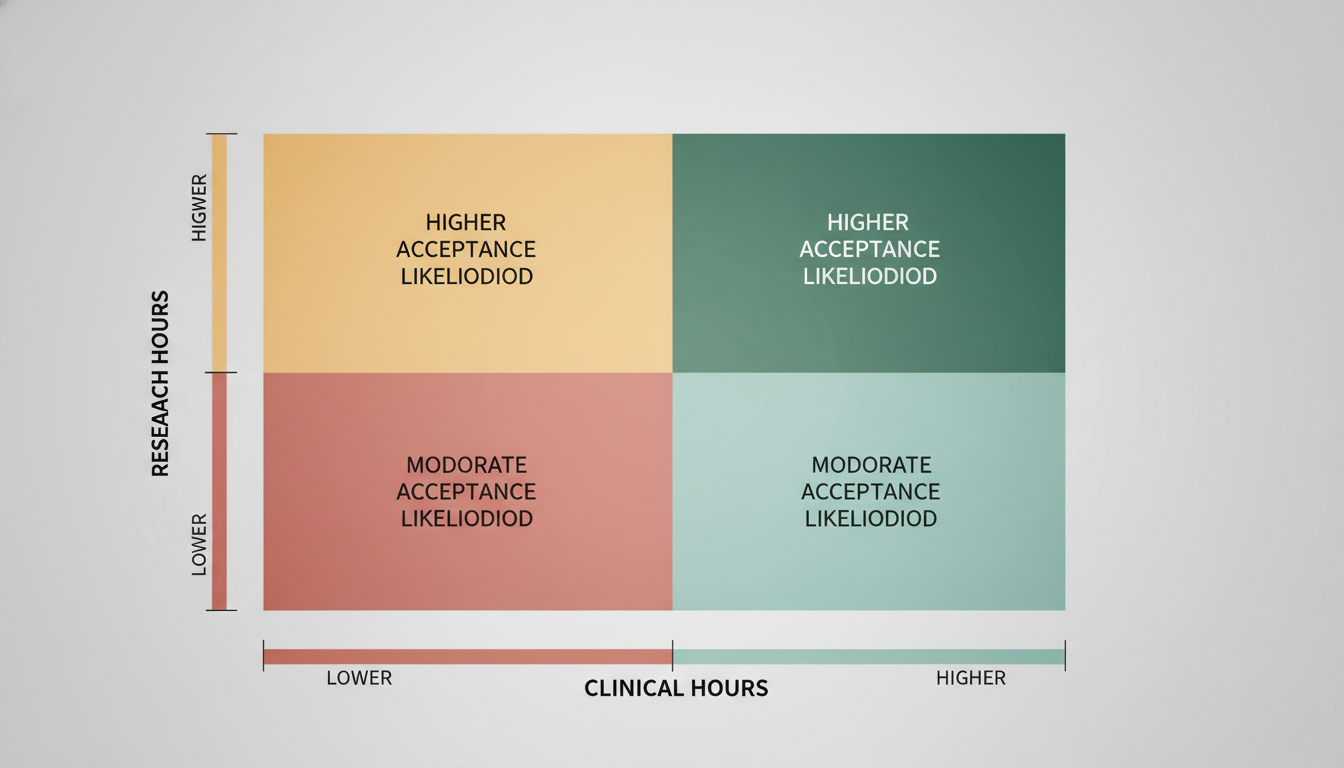
If you are forced to choose due to time constraints (work, family, late start), and your target list includes a wide range of MD schools rather than only top 10:
- The acceptance-rate-optimized allocation generally looks like:
- Secure 150–250+ hours of clinical first
- Then build 100–300 hours of research around that
- The reverse (1,000 research, 30 clinical) statistically produces more uneven outcomes outside of the ultra-research-heavy tier.
5. What Acceptance Rates Actually Reward: Patterns, Not Boxes
Admissions committees do not calculate a formula like “X hours clinical + Y hours research = Z% acceptance.” They favor coherent patterns that align with physician training.
From a data analyst viewpoint, three recurring acceptance-associated patterns emerge.
Pattern 1: Longitudinal engagement
Applicants with higher success rates typically show:
- ≥1 year in a core clinical role (e.g., weekly volunteering, scribing, MA)
- ≥6–12 months in at least one research environment
This longitudinal pattern predicts:
- Better letters (faculty and supervisors know you)
- Clearer essays and interviews (you have authentic stories, not one-off anecdotes)
- Evidence that you tested your interest in medicine over time
Pattern 2: Balanced but clinically anchored portfolio
Among accepted applicants with median or slightly above median GPA/MCAT, the modal pattern is:
- 150–300+ clinical hours
- 80–300 research hours
- Observable service or leadership roles
- Some shadowing across specialties
The data suggest that balance is rewarded, but “balance” is usually anchored by adequate clinical depth, not equal hours in all categories.
Pattern 3: Program-aligned emphasis
Where acceptance rates spike is when your portfolio lines up with institutional priorities:
- Heavy research + strong clinical → higher acceptance at research-intensive MDs.
- Heavy clinical + strong service → higher acceptance at primary care/community-focused MDs and DO programs.
- Heavy research + little clinical → concentrated acceptances at a few top labs or niche MD/PhD programs; broad rejection elsewhere.
From a pure probability standpoint, the balanced, clinically strong profile maximizes your surface area across the entire medical school landscape.
6. Strategic Recommendations Based on the Data
Translating the acceptance patterns into action:
If you have little or no clinical experience
Your primary goal should be to reach a minimum safe threshold:
- Aim for:
- 100–150 hours of direct patient-facing work over 6–12+ months.
- Common roles with strong acceptance signal:
- Hospital volunteer (patient transporter, ED volunteer, floor assistant)
- Hospice volunteer
- MA, CNA, EMT, scribe (paid roles count equally from an admissions standpoint)
From a statistical lens, moving from 0 to even 120 hours over a year has more impact on your file’s credibility than adding another 300 research hours to an already research-heavy profile.
If you already have moderate clinical but no research
- You are still viable for many MD and most DO schools, especially if your clinical and service experiences are strong.
- To improve odds, especially at mid-tier and research-oriented MD programs:
- Secure a structured research semester or year:
- 5–10 hours/week over 6–12 months
- Total 150–300 hours
- Focus on one lab where you can actually contribute, not 3 superficial stints.
- Secure a structured research semester or year:
Acceptance data indicate that going from “no research” to “one solid research experience” has a meaningful impact on your competitiveness at a significant subset of MD schools.
If you are research-heavy and clinically light
This is the most common misalignment among high-GPA, high-MCAT applicants from R1 universities.
- The data show:
- Strong outcomes at a small number of elite schools.
- Surprising rejections elsewhere due to perceived lack of tested clinical motivation.
Action:
- Rapidly strengthen your clinical profile before you apply or during a gap year:
- Commit to 4–8 hours/week of hands-on clinical for 9–12 months.
- Target at least 150–250+ meaningful clinical hours by the time secondaries and interviews occur.
From an acceptance-rate perspective, modestly rebalancing your portfolio often yields a higher probability of at least one acceptance, rather than an “all or nothing” shot at top-10 programs.
Summary: What Acceptance Rates Really Reveal
Clinical experience functions as a gatekeeper, especially outside the top research tier. Falling below ~100–150 hands-on hours is strongly associated with lower acceptance rates, regardless of research strength.
Research increases competitiveness selectively, most notably at research-intensive MD and MD/PhD programs, but beyond a moderate threshold, incremental hours show diminishing returns compared with stronger clinical engagement.
The highest overall acceptance probability usually comes from a balanced profile anchored in sustained clinical work, then complemented by structured, meaningful research aligned with your target programs.
FAQ
1. Can I get into medical school with strong clinical volunteering but no research at all?
Yes, especially at community-focused MD schools and DO programs. Many matriculants at these institutions have minimal research. However, for mid- to upper-tier MD schools, at least one structured research experience (even ~150–200 hours) modestly improves your competitive profile and signals academic curiosity.
2. How do gap years affect the clinical vs research balance and acceptance rates?
Gap years that significantly increase clinical exposure (scribing, MA, EMT, hospice, full-time volunteer coordinator) commonly correlate with improved acceptance outcomes for reapplicants. Gap years spent only adding more research to an already research-heavy, clinically thin profile show less consistent improvement unless paired with enhanced patient contact.
3. Is one publication enough to compensate for minimal clinical experience?
No. A publication is valuable, especially for research-focused schools, but it does not substitute for demonstrated clinical engagement. Data from advisors and acceptance patterns show that applicants with publications but weak clinical exposure are frequently rejected at a wide range of schools, because lack of true patient interaction raises doubts about their commitment to the practice of medicine.






















