
Only 18–22% of U.S. MD matriculants report zero physician shadowing hours, yet nearly 90% still gain some form of clinical exposure through other volunteering or work. The data show that the real differentiator is not whether you volunteer, but how your clinical hours are distributed relative to your peers.
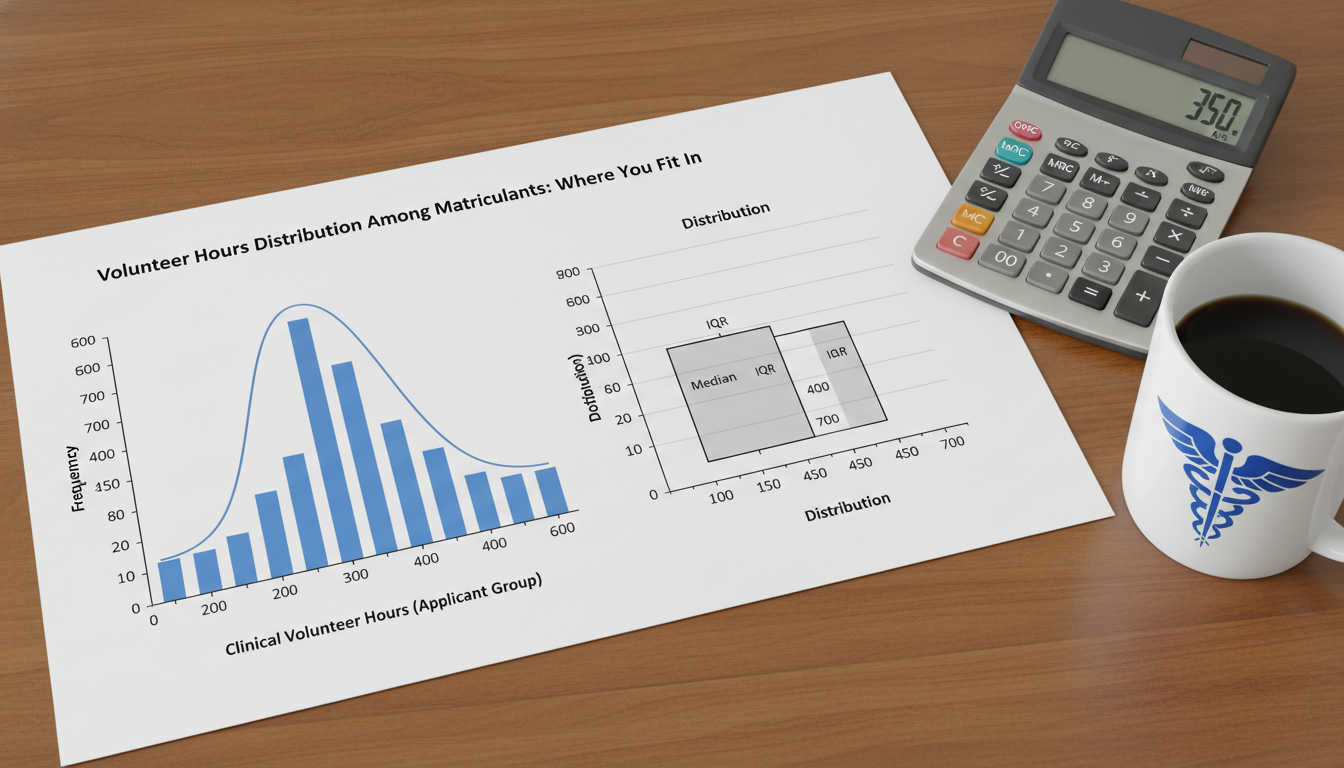
Below is a data-driven breakdown of where your volunteer hours likely place you among accepted students, using the most recent AAMC and national applicant trends, plus common ranges reported by admissions offices and advising centers.
Understanding the Landscape: How Many Hours Do Matriculants Actually Have?
Before asking “Do I have enough hours?” you have to define “enough” relative to the applicant pool. The data show several clear patterns when you aggregate AAMC data, institutional advising info (e.g., UCSF, UMich, Vanderbilt), and self-reported ranges from accepted applicants.
Across recent cycles for U.S. MD matriculants:
Clinical volunteering (non-paid)
- Median range: 100–150 hours
- Middle 50% (interquartile range): 60–250 hours
- Top quartile: >250–300 hours
Physician shadowing
- Median: 40–60 hours
- Common range: 20–100 hours
Clinical employment (scribing, EMT, CNA, MA, etc.)
- For those who have it: 400–1,000+ hours is common
- Roughly 25–35% of matriculants have substantive paid clinical experience
These numbers vary by school type, region, and applicant background, but the distribution pattern is consistent: a minority of applicants have very high hours, a minority have almost none, and most cluster in a broad middle.
Two key statistical realities:
- There is no single “cutoff”. Programs look at distributions, not a magic number.
- Quality and recency modulate quantity. A compact 120 hours of direct, longitudinal patient contact often looks stronger than 500+ disparate, indirect hours.
Clinical Volunteer Hours Distribution: Where You Fit
Let us segment clinical volunteering hours into data-driven brackets. These are not rules, but they approximate how your hours compare to others in the pool.
0–50 Clinical Volunteer Hours: The Sparse Exposure Zone
Estimated position: Bottom 15–25% of MD matriculants for clinical volunteering.
What the data imply:
- You are functionally at or near the 10th–20th percentile for non-paid clinical exposure.
- You may still be competitive if:
- You have substantial paid clinical work (EMT, MA, scribe, etc.), or
- You are applying to schools that emphasize mission fit, research, or other strengths, or
- You are very early in your timeline (1–2 years before applying) and hours are rapidly increasing.
Risk indicators:
- If you are an applicant in the upcoming cycle with ≤25 clinical hours and no paid clinical work, you are falling well below typical matriculant exposure.
- Many admissions committees describe 50 hours as a rough lower boundary for understanding whether you actually like patient care.
Action implication: At this level, the data show you benefit more from adding depth and continuity (e.g., consistent weekly volunteering) than from chasing prestige. A straightforward hospital volunteer role for 3–4 hours per week can move you out of this bracket within a semester.
50–120 Clinical Volunteer Hours: Lower-Middle of the Pack
Estimated position: 25th–45th percentile of MD matriculants.
This is where a large segment of applicants land, especially traditional juniors applying immediately.
Typical profile:
- 1–2 activities, such as:
- Hospital volunteer (front desk / transport / outpatient clinic)
- Hospice or nursing home volunteer
- Free clinic assistant
- Volunteer pattern: 1–3 hours/week over 6–12 months.
How committees often interpret this zone:
- You have credible exposure to clinical environments and patients.
- You are not obviously deficient, but your clinical experiences may not distinguish you from the median candidate.
Compensating strengths that enhance this level:
- Strong MCAT (≥515) or GPA (>3.8)
- Significant research or leadership
- Clear narrative showing progression (e.g., starting from observation and moving toward more responsibility)
If you are targeting mid-tier MD programs, this range can be workable when paired with strong academics and at least modest shadowing. For highly selective research-heavy schools, you will be competing with peers whose clinical profiles often sit in higher brackets.
120–250 Clinical Volunteer Hours: The Statistical Comfort Zone
Estimated position: 45th–75th percentile of MD matriculants.
Most advising offices informally point to this range as “solid” for non-paid clinical volunteering.
Typical characteristics:
- At least one longitudinal commitment (6–18 months)
- Direct patient contact is present in some form:
- Escorting patients
- Checking vitals under supervision
- Assisting in clinics
- Engaging with patients in hospice or long-term care
Why this range is powerful:
- The data show matriculants in this band tend to:
- Report greater clarity about choosing medicine
- Write more specific personal statements and secondaries about patient care
- Have better interview stories tied to real patient interactions
From a distribution perspective, this is where many accepted students cluster. You are no longer explaining “Why so few hours?”. You are instead using your experiences to explain “What did you learn?” and “How did you grow?”.
250–500 Clinical Volunteer Hours: Upper Quartile Differentiation
Estimated position: 75th–90th percentile of MD matriculants for volunteering alone (excluding paid work).
This range usually comes from:
- Early start (sophomore year or earlier) + steady involvement, or
- High-intensity roles (free clinics, hospice, crisis lines with clinical components) over multiple years
Common patterns:
- Working in resource-limited settings, student-run clinics, or community health environments
- Progressing from basic roles to peer coordinator, trainer, or program leader
- Clear continuity with a specific population (e.g., homeless patients, refugees, oncology patients)
What the data suggest about impact:
- You are less likely to be screened out for “insufficient clinical exposure.”
- Interviewers often see such numbers and expect mature reflection on:
- Burnout risk
- Emotional resilience
- Boundaries
- Cultural humility with patients
However, moving from 250 to 500 hours generally produces diminishing returns unless those additional hours add new dimensions: different settings, increased responsibility, or deeper leadership.
500+ Clinical Volunteer Hours: Outlier Territory
Estimated position: Top 5–10% for volunteering among traditional applicants.
Here the distribution tails off. You might reach this level if you:
- Volunteer in a clinical setting 4–8 hours/week for 2–3 years, or
- Take a gap year centered on clinical volunteering (e.g., full-time service programs)
How admissions may view this:
- Strong evidence of sustained commitment to patient care.
- For some review committees, this begins to blend functionally with entry-level clinical employment, especially when responsibilities are advanced.
Caveats the data support:
- When applicants with 600–1,000+ volunteering hours show weak academics or no other significant pillars (research, leadership, service), outcomes are often less favorable than for balanced applicants with 150–300 hours.
- Over-concentration in a single type of low-responsibility work (e.g., 600 hours of only transporting patients with no progression) can raise questions about breadth and growth.
The optimal situation is a portfolio: high hours, increasing responsibility, and integration with other parts of your narrative (research with the same population, leadership in the same clinic, etc.).
Shadowing vs. Clinical Volunteering: Different Distributions, Different Signals
Many premeds conflate shadowing and clinical volunteering. The distributions show they play complementary, not interchangeable, roles.
Shadowing Hours Distribution
Among MD matriculants:
- 0 hours shadowing: ~18–22%
- 1–20 hours: Common among students with strong clinical employment
- 20–40 hours: Frequently cited as “minimum credible exposure”
- 40–80 hours: Common target recommended by advisors
- 80–150+ hours: Seen in applicants shadowing multiple specialties or over long intervals
Interpreting your position:
- 0–10 hours: Lower end; you will likely need strong other clinical experiences.
- 20–60 hours: Typical for a solid applicant, especially with diversity of specialties.
- 60–120 hours: Upper range; more is not inherently better unless it adds:
- Primary care vs specialty variety
- Inpatient vs outpatient exposure
- Community vs academic medicine perspective
Combined Clinical Exposure: Volunteering + Shadowing + Employment
Admissions committees tend to think in terms of a portfolio of clinical exposure, not isolated numbers.
For example, consider three applicants:
Applicant A
- 60 hours clinical volunteering
- 25 hours shadowing
- No clinical employment
- Total: ~85 hours direct exposure
Applicant B
- 150 hours clinical volunteering
- 50 hours shadowing
- No clinical employment
- Total: ~200 hours exposure
Applicant C
- 80 hours clinical volunteering
- 40 hours shadowing
- 900 hours scribing
- Total: 1,020+ hours, with >800 in high-contact, paid clinical roles
From a data perspective, Applicant C’s overall clinical exposure is vastly higher, even though their volunteering alone is similar to A and lower than B. Many committees will view C as having the strongest evidence that they understand day-to-day medicine.
DO vs. MD: Different Distributions, Different Expectations
Although comprehensive national distributions are less transparent for DO schools, multiple advising sources indicate:
- DO matriculants often match or exceed MD peers in hands-on clinical experience, especially paid work (scribes, EMTs, MAs).
- Osteopathic schools frequently emphasize demonstrated interest in osteopathic medicine through:
- Shadowing DO physicians (often 20–40+ hours recommended)
- Clinical settings aligned with DO values (primary care, community medicine, rural health)
For clinical volunteering hours specifically:
- 80–200 hours is a common, competitive range for DO applicants when combined with decent shadowing.
- Applicants who target both MD and DO programs often have:
- 150–300 clinical volunteering hours
- 40–80 shadowing hours, with at least some DO exposure
Data from accepted DO applicants on public trackers frequently show heavier total clinical hours (driven by employment) but not necessarily extremely high volunteer-only hours.
Strategically Building Hours Over Time: A Data-Backed Roadmap
The distribution of hours across your undergraduate years matters. Admissions indirectly “time-weight” your experiences:
- Recent, consistent experience often carries more interpretive weight than massive, old experience concentrated in one semester.

First Year / Early Stage
Targets (if you know you are premed early):
- Build to 2–3 hours/week of clinical volunteering by the end of the year.
- Focus on:
- Understanding the hospital/clinic environment
- Basic patient interaction comfort
- Reliability and commitment
End-of-year range: 40–80 hours is very achievable without overloading.
Second–Third Year
Data-based strategy:
- Maintain or increase to 3–4 hours/week if your schedule allows.
- Over 9–10 months, this yields an additional 100–160 hours, pushing you into the 120–250+ range.
- Add shadowing in short, intense bursts (e.g., 1–2 weeks during breaks) to reach 40–60+ hours total.
By the time you apply:
- Clinical volunteering: 120–250 hours
- Shadowing: 40–80 hours
- Optional employment: as available
This positions you near the median or above for MD applicants and comfortably competitive for DO.
Gap Year / Later Stage Corrections
What if you are about to apply and your numbers fall in the sparse or lower-median zones?
Options supported by outcomes data:
- Postpone one cycle to build:
- 1 year of scribing / EMT / MA work (800–1,500 clinical hours).
- 50–150 hours of structured, direct clinical volunteering.
Applicants who take 1–2 gap years to solidify clinical exposure and maturity have been increasingly common among successful matriculants. AAMC data show more than 60% of MD matriculants now have at least one gap year, many of them for exactly this reason.
How Admissions Actually Read Your Hours
Committees do not just scan for a number and move on. They interpret your hours in context:
- Density: Did you accumulate 200 hours in 3 months or over 18 months?
- The latter signals sustained commitment.
- Trajectory: Do your hours and responsibilities increase over time?
- Moving from basic volunteer to coordinator or trainer suggests growth.
- Integration with narrative: Do your essays, activities, and interviews clearly connect your hours to:
- Understanding of physician roles
- Insight into patient experiences
- Awareness of healthcare system challenges
- Balance: A distribution like:
- 180 clinical volunteer hours
- 60 shadowing hours
- 400 research hours
- Some non-clinical service
often looks more compelling than: - 900 clinical volunteer hours
- Almost nothing else
When you ask, “Where do I fit in?”, the data-based answer must consider your whole distribution of experiences, not volunteer hours in isolation.
Quick Self-Classification Tool
Use this simplified framework to approximate your standing relative to MD applicants:
Clinical volunteering
- <50 hours → Below typical range; high risk without compensation
- 50–120 hours → Lower-middle; can work with strong portfolio
- 120–250 hours → Middle to upper-middle; generally solid
- 250–500 hours → Upper quartile; strong, especially with good reflection
500 hours → Outlier; powerful if balanced and with clear growth
Shadowing
- <20 hours → Weak unless compensated by heavy clinical employment
- 20–60 hours → Typical/solid
- 60–120 hours → Strong and well-distributed
Paid clinical work
- 0–200 hours → Minimal
- 200–600 hours → Moderate; noticeable strength
- 600–1,500+ hours → High; can anchor your clinical narrative
Place yourself in each category and ask:
- Is my clinical picture weak, average, or strong compared to likely matriculants?
- Does my academic profile allow a slightly weaker clinical profile, or do I need experience to offset metric vulnerabilities?
- Do my experiences show patterned growth, not just raw time?
Once you map your distributions, you can build a rational plan rather than guessing.
With a clear understanding of where your volunteer hours fall in the real distributions, you can now shift focus from “Do I have enough?” to “How do I make the experiences I have count in my story?” Those narrative and application strategy questions shape your secondaries, activity descriptions, and interviews—steps that sit just beyond the numerical analysis, and will define the next phase of your journey into medicine.
FAQ
1. Is there an exact minimum number of clinical volunteer hours I need for medical school?
No fixed national cutoff exists. The data show most MD matriculants fall between 60–250 clinical volunteering hours, but applicants below that range can still succeed if they have strong shadowing and paid clinical work. Many admissions offices informally reference 50–100 hours of clinical volunteering as a practical minimum to demonstrate you understand patient care settings, especially if you do not have clinical employment.
2. Do online or remote clinical experiences count toward my clinical volunteering hours?
Hybrid or telehealth roles can count if you are genuinely interacting with patients or supporting active clinical care teams. Examples include assisting with telehealth workflows or remote patient education. However, activities that are fully administrative or purely virtual without patient-facing elements are weighted less like clinical volunteering. The data from successful applicants suggest these hours function best as a supplement, not a replacement, for in-person patient exposure.
3. Is it better to have 300+ hours in one clinical site or 150 hours at two different places?
The distributions alone do not answer this; the pattern of engagement does. Matriculant data and committee feedback favor longitudinal depth with progression. One site with 300 hours where you move from basic tasks to more responsibility and leadership often reads stronger than two shorter, fragmented stints. However, two sites totaling 150–200 hours can be powerful if they show meaningful contrast (e.g., inner-city free clinic plus rural primary care) and you draw clear insights about different patient populations and systems.






















