 project Medical students collaborating on a [clinical case series](https://residencyadvisor.com/resources/medical-research/meded-rese](https://cdn.residencyadvisor.com/images/articles_v3/v3_RESEARCH_IN_MEDICINE_creating_a_clinical_case_series_inclusion_criteria-step1-medical-students-collaborating-on-a-clin-5860.png)
You are a second-year medical student sitting in a quiet corner of the hospital library. Your mentor just said, “You know, we have seen three patients with this exact rare complication in the last year. That could be a nice little case series.” You nod, but your mind is racing:
What exactly turns “a few interesting patients” into a clinical case series? What counts as inclusion criteria? How do you go from scattered charts to something ready for journal submission—especially when you are still early in your training?
Let me walk you through this step by step, from defining the cases to hitting “submit” on your manuscript.
(See also: Basic Biostatistics for Student Researchers for essential statistical concepts.)
Understanding What a Case Series Really Is (and Is Not)
A clinical case series sits in a specific niche on the evidence hierarchy. You need to understand that niche clearly or you will design the wrong project from the start.
A case series is:
- A descriptive study
- Usually retrospective (though it can be prospective)
- Focused on patients with the same condition, exposure, procedure, or outcome
- Without a formal control group
It is not:
- A randomized trial
- A cohort study with formal comparison groups
- Just a “pile of case reports” with no structure
You are typically doing one of three things with a case series:
Characterizing a rare condition or presentation
Example: “Clinical features of 11 patients with MIS-C presenting without fever.”Describing outcomes of a specific intervention or management strategy
Example: “Outcomes of 15 patients treated with off-label drug X for refractory vasculitis.”Identifying patterns in complications or adverse events
Example: “Perioperative complications in 9 patients undergoing a novel surgical technique.”
For premeds and early medical students, case series projects are often the first real step into clinical research. They are relatively feasible: no randomization, no complex statistics, often based on chart review.
But they are only publishable if your research question, case definition, and inclusion/exclusion criteria are thought through from the start.
Step 1: Defining a Focused Research Question
Before you even say “inclusion criteria,” you need a clear, narrow question that your mentor, IRB, and journal editor can all understand in one sentence.
Overly vague:
- “We want to describe patients with sepsis.”
- “We want to look at people who had surgery here.”
Sharpened and specific:
- “Among adult ICU patients with culture-proven sepsis due to ESBL-producing organisms, what clinical characteristics and initial management strategies were associated with survival to discharge?”
- “In patients undergoing laparoscopic cholecystectomy who developed bile duct injury, what were the presenting features, timing of recognition, and management outcomes?”
You want:
- A specific population (age group, setting, disease subtype)
- A specific phenomenon (presentation, intervention, complication, outcome)
- A specific time frame (e.g., 2018–2024)
- A specific purpose (describe, characterize, generate hypotheses)
Try framing your question in a PEO structure (Population–Exposure–Outcome) instead of full PICO, since you typically do not have a comparison group:
- Population: Who exactly are the patients?
- Exposure / Index feature: What unifies them? (a disease, procedure, complication)
- Outcome / Features: What are you describing? (clinical features, imaging, lab patterns, short-term outcomes)
Example for a student-level project:
- Population: Adults ≥18 years admitted to Hospital X
- Exposure: Severe COVID-19 treated with ECMO
- Outcome/Features: Complications, length of stay, in-hospital mortality
The subtle but critical point: your research question will directly dictate your inclusion and exclusion criteria. If the question is vague, the criteria will be vague, and your data will be messy.
Step 2: Designing Inclusion and Exclusion Criteria That Actually Work
This is where many student-driven projects derail. They have “interesting cases” but no rigorous definition of what counts as a case.
You want your inclusion criteria to be:
- Operationalized: Each criterion can be checked in the chart. No guesswork.
- Reproducible: Another researcher, given the same criteria, would select the same patients.
- Aligned with your question: Every criterion directly supports your focus.
Core Components of Inclusion Criteria
When you sit down with your mentor, you should explicitly define:
Clinical condition / index event
- ICD-10 codes (e.g., I63.x for ischemic stroke)
- Diagnostic criteria (e.g., Berlin criteria for ARDS, ACR criteria for SLE)
- Clear procedural codes if procedure-based (CPT, ICD-10-PCS)
Time frame
- Example: “January 1, 2016 to December 31, 2023.”
- Choose a period that gives enough cases but is still manageable for chart review.
Setting
- Single center vs multi-center
- Inpatient vs outpatient vs emergency department
- Specific unit if relevant (e.g., NICU, burn unit)
Age range and basic demographics
- Adults vs pediatric vs neonatal
- Sex, if relevant to condition (e.g., OB/Gyn series)
Diagnostic confirmation
- Pathology-confirmed diagnosis?
- Radiology-confirmed?
- Clinical criteria + lab markers?
Example: Good vs Weak Inclusion Criteria
Weak:
“Patients with complicated appendicitis at our hospital over five years.”
Better:
“All patients aged 5–18 years who underwent appendectomy at [Hospital Name] between January 1, 2017 and December 31, 2021, with intraoperative documentation of perforated or gangrenous appendicitis in the operative note or pathology report, and available complete inpatient records up to discharge.”
Notice what changed:
- Age range is explicit.
- Time frame is specific.
- “Complicated” is defined by intraoperative or pathology findings.
- “Complete records” becomes a criterion. You will thank yourself later.
Exclusion Criteria: Be Intentional, Not Random
Exclusion criteria should not be a dumping ground for patients who “make the data messy.” They should be:
- Pre-specified
- Justified
- Non-overlapping with inclusion criteria
Common exclusion examples:
- Incomplete medical records (missing key outcome data)
- Transferred patients where initial management data are unavailable
- Patients who declined consent (in prospective series or where consent is required)
- Co-existing conditions that fundamentally change the disease process being studied
(e.g., excluding patients with HIV from a case series of classic Kaposi sarcoma if you are focusing on HIV-negative cases)
What you should avoid:
- Excluding patients because their outcome “does not fit the pattern you expected.” That is selection bias, and reviewers will pick up on it quickly.
Step 3: Identifying and Assembling the Cohort
Once your criteria are defined, you need a systematic way to actually find the cases.
For a premed or early medical student, this is often the first encounter with hospital data systems.
Practical Strategies for Case Identification
ICD/CPT Code Searches
- Ask a resident or data analyst for help querying the EMR.
- Example: ICD-10 K35.2 for acute appendicitis with generalized peritonitis.
- Combine diagnosis and procedure codes if needed.
Departmental Logs
- Surgical logbooks
- ICU admission lists
- Specialty service lists (e.g., transplant, ECMO, interventional radiology)
Pathology or Radiology Databases
- Pathology: to identify rare tumors or histologic diagnoses
- Radiology: to find specific imaging patterns (e.g., cerebral venous sinus thrombosis)
Existing Registry or Quality-Improvement Databases
- Stroke registry, sepsis registry, trauma registry, etc.
- These can speed up case identification significantly.
Example Workflow
Let us say you are doing a case series of “spontaneous spinal epidural hematoma” presentations at a tertiary care center.
Your workflow might be:
- Identify relevant ICD-10 diagnosis codes (e.g., G95.2, plus related).
- Request a list from hospital data services of all patients with those codes over a 10-year period.
- Review the radiology reports to confirm spinal epidural hematoma.
- Exclude patients with traumatic etiologies if your series is “spontaneous” only.
- Record basic identifiers in a secure, IRB-compliant spreadsheet.
At every step, you must apply your inclusion/exclusion criteria consistently. This is what separates a legitimate case series from an anecdotal collection.
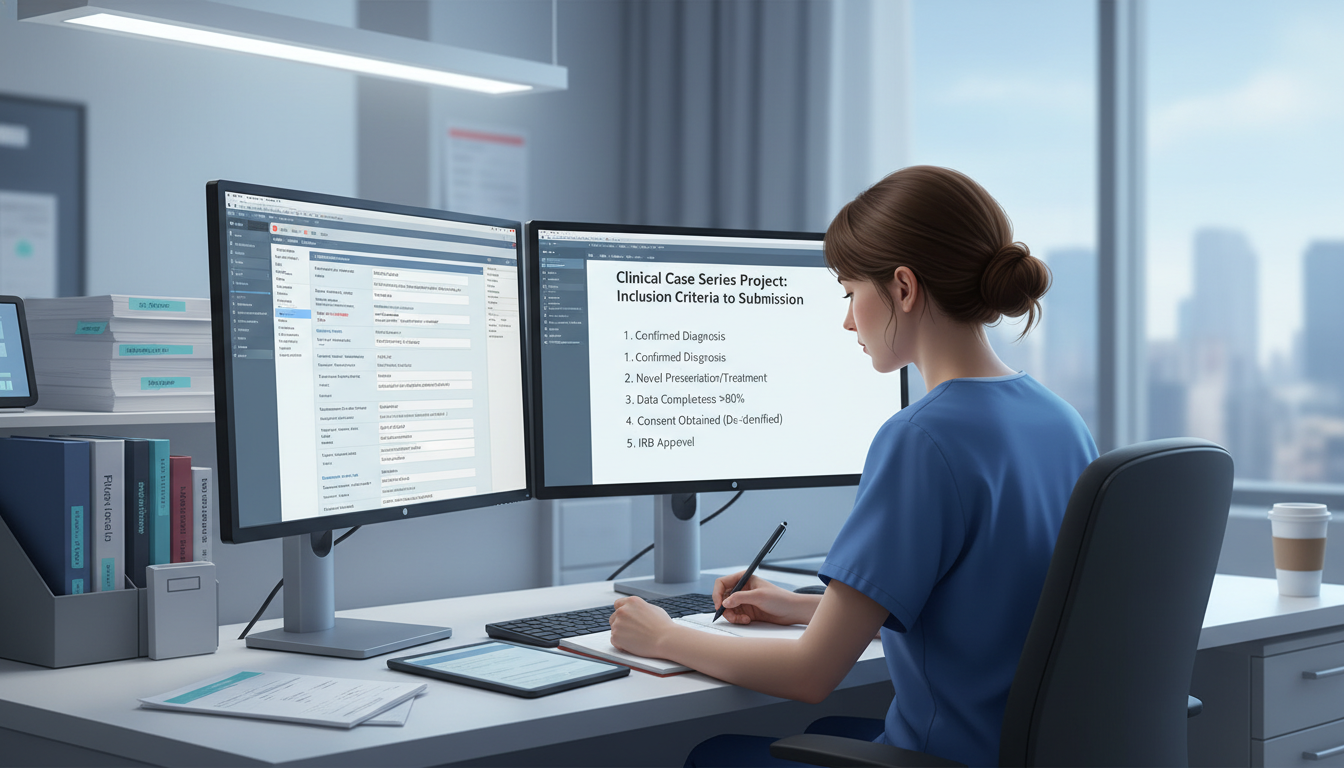
Step 4: IRB, Ethics, and Patient Privacy
Many students assume “case series” automatically means “no IRB needed.” That assumption can get you, and your mentor, into real trouble.
You must ask two questions:
Is this activity human subjects research?
- If you are intending to contribute to generalizable knowledge (i.e., publish), most institutions will treat it as research.
- Even retrospective chart reviews often require IRB review or exemption.
Does your institution have a specific policy on case reports vs case series?
- Some define a “case report” as ≤3 patients and exempt it from IRB, requiring only privacy safeguards.
- Once you cross that threshold (4+ patients), many IRBs expect at least an exempt or expedited review.
For a Case Series Specifically
- Retrospective series using de-identified data often qualify for exempt or expedited review, but you still need that determination in writing.
- Prospective series (you are enrolling patients now and following them) more often require full consent and formal IRB approval.
Your role as a student:
- Do not submit IRB protocols on your own without a faculty sponsor.
- Ask explicitly: “For this retrospective case series with X patients over Y years, do we need IRB approval, and what level?”
- Help your mentor draft the protocol sections you can handle:
- Study objectives
- Inclusion/exclusion criteria
- Data elements to be collected
- Plan for data storage and de-identification
Always plan to:
- Use study IDs instead of names or MRNs in your working dataset.
- Store the ID key in a secure, access-limited file, separate from your main data.
- Remove direct identifiers (name, DOB, address, MRN) from any materials that may leave the institution, including drafts shared by email.
HIPAA and local privacy rules are not “attending-only.” If you touch real patient data for research, you share the responsibility.
Step 5: Designing Your Data Collection Tool
Now you know who is in your series and that you are ethically covered. The next question is: what information will you actually extract from the charts?
A well-structured data collection tool (usually in REDCap or a spreadsheet) makes or breaks your project.
Core Data Elements
Most case series will include several broad categories:
Demographics
- Age at presentation
- Sex/gender
- Race/ethnicity (if relevant and available)
- BMI, if relevant
Clinical History
- Relevant comorbidities (e.g., diabetes, CKD, cancer)
- Duration of symptoms before presentation
- Prior treatments related to your condition (e.g., prior chemotherapy)
Presentation Details
- Key signs/symptoms
- Vital signs on presentation
- Laboratory values (you must define specific labs and time points)
- Imaging findings (structured fields, not just “CT abnormal”)
Interventions / Management
- Type of treatment (medical, surgical, procedural)
- Doses, timing, approaches (e.g., open vs laparoscopic)
- ICU admission, ventilator use, vasopressors if relevant
Outcomes
- In-hospital mortality
- Complications (you need to define these a priori)
- Length of stay (ICU and total)
- Functional outcomes (e.g., modified Rankin score for neuro cases)
- Follow-up time and status (if data are available)
Example: Data Fields for a Case Series of ECMO in COVID-19
Your collection sheet might include:
- Age, sex, BMI
- Comorbidities: hypertension (Y/N), diabetes (Y/N), CKD (Y/N), etc.
- Days from symptom onset to hospitalization
- Days from hospitalization to intubation
- Days from intubation to ECMO initiation
- Ventilator settings at ECMO initiation (FiO2, PEEP, plateau pressure)
- ECMO type (VV vs VA)
- ECMO duration
- Major complications:
- Stroke (Y/N)
- Major bleeding requiring transfusion (Y/N)
- Renal replacement therapy (Y/N)
- Survival to ECMO decannulation (Y/N)
- Survival to hospital discharge (Y/N)
Note how each variable is discrete and clearly defined. “Got worse” is not a variable. “Required ECMO within 7 days of intubation” is.
As a student, your job is to help build this form in a way that balances:
- Enough data to tell a complete clinical story
- Not so much data that each chart review takes 2 hours and burns you out
Before charting 30 patients, pilot your form on 2–3 cases, then refine.
Step 6: Analyzing and Interpreting the Data (Descriptively)
Case series are descriptive. Your primary outputs will be:
- Counts and percentages
- Means/medians with standard deviations or IQRs
- Sometimes simple exploratory comparisons (but do not overreach)
Typical Analyses for a Case Series
- Number of patients meeting criteria over the time period
- Age distribution (mean ± SD or median [IQR])
- Sex distribution
- Frequency of major clinical features (e.g., “fever in 10/12 patients,” “acute kidney injury in 7/12 patients”)
- Timing variables: median days from symptom onset to presentation, time to intervention
- Outcome frequencies: survival, complications, readmissions
You can stratify descriptively:
- Survivors vs non-survivors (just describe; do not claim causality)
- Patients with vs without a specific complication
- Early vs late intervention groups, as long as you frame this carefully
What you should avoid:
- Complex multivariable modeling unless your numbers are larger and you have statistical support.
- Strong causal language (“X caused Y”) in the absence of a comparator and robust design.
- Overinterpreting rare events in a very small N.
Your goal is to describe patterns that may generate hypotheses for larger studies. That is completely legitimate and valued when done honestly.
Step 7: Writing the Case Series: Structure That Journals Expect
Now you have your cohort identified, data collected, and preliminary analyses done. Time to write.
For clinical journals, a case series manuscript usually follows a structure similar to an original article, but with some nuances.
1. Title
Clear, specific, and honest about what the paper is.
Examples:
- “Spontaneous Spinal Epidural Hematoma: A Case Series of 9 Patients from a Tertiary Care Center”
- “Extracorporeal Membrane Oxygenation for Severe COVID-19: A Retrospective Case Series of 15 Patients”
Avoid vague titles like “Our Experience with…” unless the journal’s style leans that way.
2. Abstract
Often structured, even for case series. Typical components:
- Background: One or two sentences of context.
- Methods: Design, setting, inclusion criteria, time frame.
- Results: Key numbers, main clinical features, major outcomes.
- Conclusion: One restrained sentence on what your series adds.
Example conclusion line:
“In this single-center case series, severe bleeding and prolonged ECMO duration were common, while overall survival to discharge was limited.”
3. Introduction
Short, focused:
- What is already known about this condition or intervention?
- What gap does your case series fill?
- What is your objective, in one clear sentence?
For student-led work, concise is safer. One or two well-sourced paragraphs often suffice.
4. Methods
This is where the rigor of your inclusion/exclusion criteria shows.
Key subsections:
Study Design and Setting
- “We conducted a retrospective case series at a 900-bed academic medical center.”
Patient Selection
- Explicit inclusion and exclusion criteria
- How cases were identified (codes, logs, databases)
- Time frame
Data Collection
- How data were abstracted
- What variables were collected
- How missing data were handled (e.g., listwise deletion, noted as missing)
Ethics
- IRB approval number or exemption
- Consent details if prospective
Do not gloss over patient selection. Reviewers and editors scrutinize this in case series.
5. Results
Organize logically:
Baseline characteristics table
- Table 1 with demographics and key comorbidities.
Clinical presentation and diagnostics
- Narrative summary plus possibly a table or figure.
- Highlight consistent or distinctive patterns.
Management and interventions
- How many received which treatments.
- Timing variables if relevant.
Outcomes
- Survival
- Complications
- Functional outcomes or follow-up
You can intersperse short illustrative vignettes if the journal allows, but keep in mind this is a series, not 10 separate case reports. The emphasis should be on patterns.
6. Discussion
Four pieces to aim for:
Brief summary of main findings
- One concise paragraph.
Comparison with existing literature
- How do your patients’ presentations, treatments, or outcomes align or differ?
- Are there prior case series, cohorts, or trials in this area?
Interpretation and implications
- What hypotheses does your series suggest?
- Are there potential practice or diagnostic implications?
Limitations
- Retrospective design
- Single center
- Small sample size
- Potential selection bias
- Missing data
- Limited follow-up
End on a balanced note: emphasize what your series contributes without overselling its importance.
7. Tables and Figures
For a student-led case series, 2–4 tables/figures is typical:
- Table 1: Baseline characteristics
- Table 2: Clinical features and treatments
- Table 3: Outcomes and complications
- Optional figure: Flow diagram of case selection or a timeline graphic
Carefully de-identify any imaging figures (e.g., remove names, dates, MRNs from DICOM exports).
Step 8: Targeting the Right Journal and Final Submission
Not every case series belongs in NEJM, and that is fine. Your goal is to match:
- Topic + scope + rigor
with - Journal audience + impact level
Choosing a Journal
Consider:
- Specialty focus: If your series is on pediatric appendicitis, pediatric surgery or general surgery journals are natural.
- Case report/series–friendly journals:
- BMJ Case Reports
- Journal of Medical Case Reports
- Many specialty journals have “Case Report” or “Case Series” sections.
- Institutional journals: Some large academic centers have their own journals, which are often good first submissions for student projects.
Check:
- Author guidelines for case reports/series.
- Word limits, figure/table limits.
- Requirements for patient consent in case series (varies by journal and country).
Submission Checklist
Before you click submit:
- Manuscript formatted per journal guidelines (references, headings, abstract format).
- All authors:
- Agree on authorship order.
- Meet authorship criteria (substantial contribution, drafting or critical revision, approval of final version).
- IRB approval or exemption letter available if requested.
- Any required patient consent forms obtained and documented.
- Figures de-identified fully.
- Cover letter clearly states:
- Type of article (retrospective case series)
- Why this series is relevant for the journal’s readership
- That the work is original and not under review elsewhere.
Rejection is common. If it happens, use reviewer feedback to refine and submit to the next appropriate journal. Many case series find a home eventually if the clinical content is meaningful and the methodology sound.
How This Fits into Premed and Medical School Preparation
From a training perspective, working on a case series as a student teaches you concrete, transferable skills:
- How to formulate a researchable clinical question
- How to define operational inclusion/exclusion criteria
- How to navigate IRB and ethical considerations
- How to extract structured data from messy real-world charts
- How to write a coherent, clinically grounded manuscript
Admissions committees and residency PDs recognize this. A well-done case series shows that you:
- Understand clinical context
- Can handle data responsibly
- Can see a project from conception to submission
If you are early in your journey, your best move is usually:
- Find a mentor with a real clinical question and cluster of relevant patients.
- Offer to help with chart review, data abstraction, and first-draft writing.
- Use the project to learn the full arc from “inclusion criteria” to “submission portal.”
Key Takeaways
- A publishable clinical case series starts with a precise research question and operational inclusion/exclusion criteria that any other researcher could apply and reproduce.
- Rigorous case identification, ethical oversight, and structured data collection are what separate a genuine case series from a pile of anecdotes.
- To reach submission, you must write and structure the series like a formal study—clear methods, honest limitations, descriptive results—then match it to an appropriate journal that welcomes well-constructed case series.





















