
Why Research During Residency Matters So Much for IMGs in Radiation Oncology
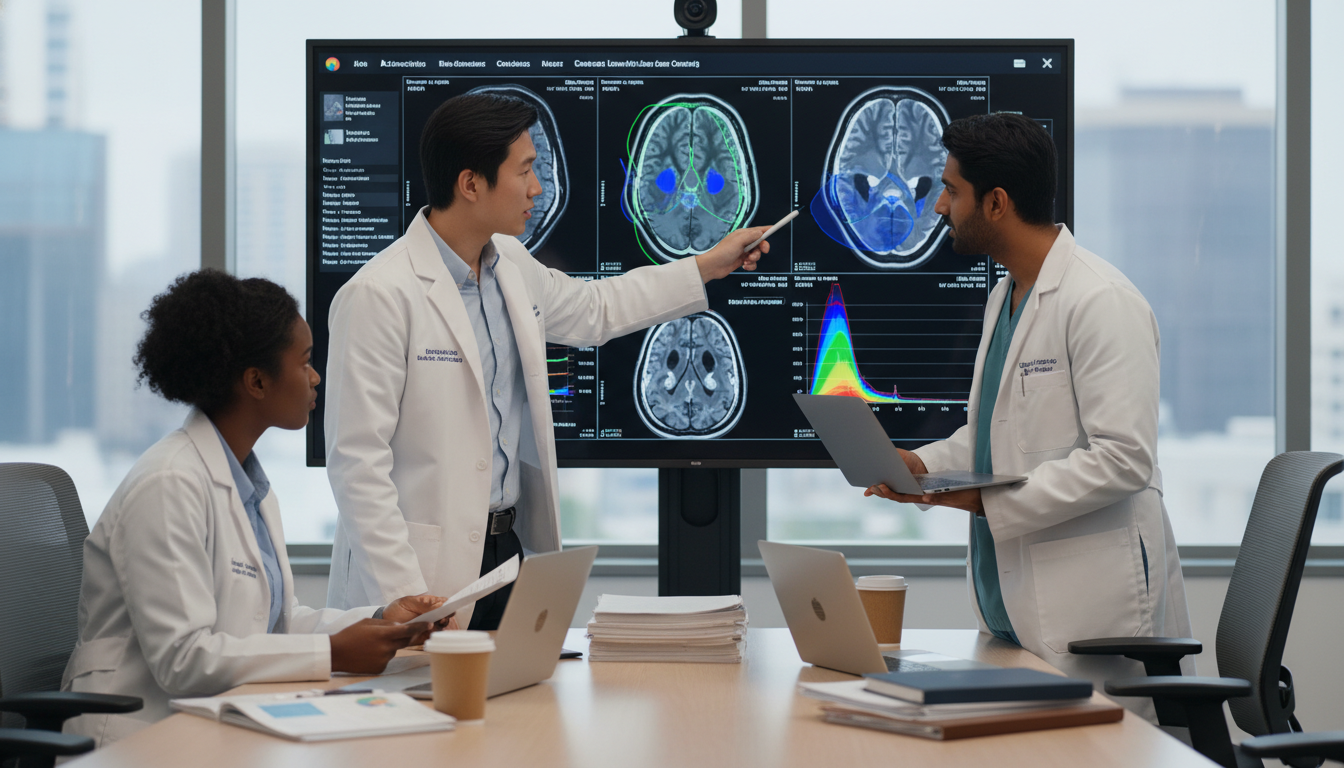
Radiation oncology is one of the most research-driven clinical specialties in medicine. Advances in imaging, treatment planning, radiobiology, and technology are almost entirely propelled by clinical trials and translational science. For an international medical graduate (IMG), research during residency is not just “nice to have” – it can be career-defining.
In many departments, your ability to critically appraise evidence, design resident research projects, and contribute to publications is a key marker of your long-term potential. This is especially true if you’re interested in:
- An academic residency track
- A research-heavy fellowship
- A future in clinical trials leadership, outcomes research, or global oncology
This IMG residency guide focuses on how you, as an international medical graduate in a radiation oncology residency, can strategically use research to:
- Strengthen your academic profile
- Build a competitive portfolio for faculty positions or fellowships
- Expand your professional network in North America or Europe
- Make your clinical training more intellectually rewarding and future-proof
Whether you already matched into radiation oncology or you’re planning ahead for the rad onc match, understanding how to approach research during residency will give you a real edge.
Understanding the Research Landscape in Radiation Oncology
Radiation oncology is uniquely positioned at the intersection of technology, biology, and patient care. That means there are multiple research domains you can enter, even if you’re starting with limited experience.
Major Research Domains You’ll Encounter
Clinical Outcomes and Comparative Effectiveness
- Retrospective chart reviews (e.g., local control or toxicity rates with different fractionation schedules)
- Prospective observational studies
- Comparative studies of radiation techniques (IMRT vs 3D-CRT, SBRT vs conventional RT)
Translational and Radiobiology Research
- Radiosensitizers and radioprotectors
- Tumor microenvironment and DNA damage repair pathways
- Biomarkers predicting response or toxicity
Physics and Technology-Oriented Research
- Treatment planning optimization
- Image-guided radiotherapy and adaptive RT workflows
- QA methodologies and dosimetric assessments
- Emerging tech: proton therapy, MR-Linac, FLASH, AI-based planning
Quality Improvement (QI) and Safety Studies
- Standardizing contouring practices
- Reducing treatment delays
- Enhancing workflow safety (e.g., checklists, timeout protocols)
Health Services, Outcomes, and Global Oncology
- Access to radiation therapy in low- and middle-income countries
- Cost-effectiveness of technologies
- Disparities in outcomes by race, socioeconomic status, or geography
For an IMG, certain domains may be more accessible initially:
- Retrospective clinical projects and QI initiatives often require fewer resources and less protected lab time.
- Global oncology topics may align closely with your previous experience and perspective as an international medical graduate.
Where Research Fits Within Your Residency Timeline
Radiation oncology residencies (particularly in the US and Canada) are often 4–5 years. A common structure is:
PGY-2–3 (early clinical years):
- Learn fundamentals of contouring, planning, on-treatment visits.
- Start simple retrospective or QI projects.
- Join existing resident research projects.
PGY-3–4 (mid-residency – prime research time):
- Initiate and lead more substantial projects.
- Prepare conference abstracts and manuscripts.
- Possibly take a dedicated research elective (4–12 weeks, depending on program).
PGY-4–5 (senior years):
- Complete ongoing projects; focus on publications.
- Transition projects to junior residents.
- Use research output to support career planning (academic track vs private practice, fellowship applications, visas).
Understanding this timeline early allows you to align your energy and expectations with what’s realistically achievable at each stage.
Getting Started: First Steps for IMGs in a New System
Many international medical graduates enter radiation oncology residency in a completely new healthcare system. You may feel behind compared with US or Canadian graduates who have already done research at that institution. You can catch up quickly by being intentional.
Step 1: Map the Department’s Research Ecosystem
In your first 1–3 months:
Identify key research leaders:
- Program Director (PD)
- Vice Chair or Director of Research
- Site disease leaders (e.g., Breast, GU, CNS, Thoracic)
- Medical physicists with ongoing projects
- Active research fellows or senior residents
Learn what kinds of projects typically succeed in your department:
- Check departmental publications and recent conference abstracts (ASTRO, ESTRO, ASCO, ABS).
- Ask residents: “Which kinds of projects move quickly here and are realistic for residents?”
Clarify available support:
- Biostatistics core?
- Research coordinators?
- Access to databases and electronic medical records (EMR)?
- Internal funding for small projects or conference travel?
This quick “research landscape scan” helps you target advisors who have a track record of getting residents across the finish line.
Step 2: Be Honest About Your Starting Point
Ask yourself:
- Have I done research before, even if not in oncology?
- Am I comfortable with:
- Basic research design (cohort, case-control, RCTs)?
- Reading and understanding hazard ratios, odds ratios, p-values, confidence intervals?
- Writing in English for academic journals?
If you are starting with minimal experience, prioritize two foundational skills in the first 6–12 months:
- Literature appraisal (knowing what’s been done and what’s missing)
- Simple data management and analysis (Excel or basic statistical software)
Take advantage of:
- Institutional workshops on biostatistics and study design
- Online resources (e.g., ASTRO webinars, NCCN educational material)
- Free statistical software tutorials (e.g., R, SPSS videos; many hospital libraries provide free access)
Step 3: Begin with “Low-Barrier” Resident Research Projects
As an IMG adapting to a new system, picking the right first project matters. Aim for something with:
- Clearly defined scope
- Existing data or protocols
- An experienced mentor
Examples well-suited to early residency:
- A retrospective review of toxicity outcomes after SBRT for lung lesions treated in the past 5 years
- A QI project standardizing documentation of ECOG performance status before starting radiotherapy
- A patterns-of-care study for prostate hypofractionation in your department
- A small project assessing adherence to contouring guidelines (e.g., RTOG atlases)
These projects teach you:
- How to navigate the EMR
- How to de-identify data
- Basics of IRB/ethics submissions
- Early abstract and manuscript writing
Completing one such project to publication or presentation early builds your confidence and credibility.
Building a Sustainable Research Portfolio During Residency
Once you’ve done your first project, your goal shifts from “get something done” to “build a coherent academic story.” This is especially important if you’re aiming for:
- An academic residency track
- A post-residency faculty or fellowship position
- Competitive visas or sponsorship that may rely on your academic impact
Choosing a Reasonable “Niche” as an IMG
You don’t need a permanent subspecialty focus in PGY-2, but it helps to select 1–2 disease sites or themes where you concentrate your resident research projects.
Common “niche” examples in radiation oncology:
Disease-site oriented:
- Prostate cancer hypofractionation and toxicity
- CNS tumors and reirradiation strategies
- Head and neck cancer and adaptive RT
- Breast cancer regional nodal irradiation
Methodology or theme-oriented:
- Stereotactic body radiation therapy (SBRT/SABR)
- Reirradiation outcomes
- Toxicity prediction and normal tissue constraints
- Global radiation oncology and access to care
- Quality and safety in complex planning
For IMGs, leveraging your background can be an advantage. For example:
- If you previously worked in a low-resource setting, global oncology or access-to-care research may be a natural fit.
- If you have physics or engineering experience, you might align with planning optimization or AI-based decision support.
Balancing Project Types: Quick Wins vs. High Impact
A strong IMG residency guide for research emphasizes diversification:
Short-term, quick-win projects (3–9 months)
- Single-institution retrospective reviews
- QI interventions with pre/post analysis
- Small dosimetric comparison studies
- Outcomes of specific protocols used in your department
Longer-term, higher-impact projects (12–24+ months)
- Multi-institutional collaborations
- Prospective observational studies
- Complex large dataset analyses
- Roles in ongoing clinical trials (e.g., substudies, correlative work)
As an IMG, having a mix of both is critical:
- Quick projects help build your CV early (abstracts, posters, small papers).
- Larger projects demonstrate depth, leadership, and the ability to manage complexity.
A realistic goal by the end of residency:
- 4–8 conference abstracts (local, national, or international)
- 3–6 peer-reviewed publications (not all as first author, but at least 1–2 where you lead)
- Clear alignment around one or two research themes
Practical Time Management Strategies
Research during residency competes with:
- Clinical duties and call
- Board preparation
- Personal and family responsibilities
- Visa or immigration-related tasks (very real for IMGs)
Some practical strategies:
- Block protected time, even if unofficial:
- Example: Wednesday and Friday evenings 7–9 pm reserved for research-related reading and writing.
- Use rotation variation:
- Busier inpatient/GU/H&N months: focus on data collection and small tasks.
- Lighter rotations or elective time: push writing and analysis.
- Apply the “Rule of One”:
- Each week, aim for at least one tangible research output: one page written, one figure drafted, one IRB form section completed, one dataset cleaned.
Communication helps:
- Let your mentor know your schedule constraints.
- Set realistic deadlines and negotiate them early.
- If you are on visa restrictions and cannot easily extend training, be very upfront about your available windows for intensive work.
Practical Steps: From Idea to Publication
Many residents struggle not with ideas, but with execution. Breaking the process into discrete, manageable steps is essential.
1. Generating a Feasible Research Question
Use the FINER criteria for your research question:
- Feasible – Do you have enough patients, time, and support?
- Interesting – To you and to the field.
- Novel – Adds something incremental or confirms/extends prior findings.
- Ethical – Meets IRB/ethics board expectations.
- Relevant – To patient care, practice patterns, or scientific understanding.
Example:
- Broad idea: “I want to study head and neck cancer outcomes.”
- Narrowed question:
“Among patients with HPV-positive oropharyngeal cancer treated at our institution between 2014–2022, what is the association between total RT treatment time and locoregional control?”
The second question is more focused, measurable, and actionable within a residency timeline.
2. IRB / Ethics Approval: What IMGs Need to Know
As an international medical graduate, you may be less familiar with the IRB process in your new system. Key tips:
- Start with retrospective chart reviews; IRBs are usually more straightforward.
- Ask for templates from prior approved projects in your department.
- Learn the department’s expectations for:
- Data security and storage
- De-identification and HIPAA/GDPR compliance
- Authorship and conflict of interest reporting
Be sure to:
- Clarify whether your project is research vs QI (different oversight structures).
- Anticipate 4–12 weeks for IRB review depending on your institution.
- Keep all approvals and correspondence organized – they may be needed if you move institutions.
3. Data Collection and Collaboration
For many resident research projects, data collection is the most time-consuming phase. Make it systematic:
- Use standardized data collection sheets (Excel, REDCap, institutional databases).
- Define your variables before abstraction (e.g., toxicity scales, staging, dose metrics).
- If language or documentation practices in your new system are unfamiliar, do pilot abstraction on 5–10 patients to refine definitions.
As an IMG, you may have to adjust to:
- Different naming conventions for labs, imaging, and progress notes.
- Specific structured fields vs free-text documentation.
Collaborate when possible:
- Splitting data collection with co-residents or medical students can dramatically accelerate progress.
- In return, ensure clear authorship agreements upfront (agree on first, second, and last authorship and expectations).
4. Basic Analysis and Working With Biostatistics
You don’t need to become a biostatistician, but for research during residency you should:
- Understand basic statistical tests: t-test, chi-square, logistic and Cox regression.
- Be able to communicate clearly with statisticians:
- Primary outcome (e.g., overall survival, local control, grade ≥2 toxicity)
- Key covariates and confounders
- Planned subgroup analyses (only when justified)
Many institutions require a statistician’s sign-off for abstracts and manuscripts. Build a professional relationship and respect their time by:
- Sending a clean, labeled dataset.
- Providing a 1-page summary of your project, research question, and hypothesis.
5. Writing Abstracts and Manuscripts as an IMG
Writing in academic English may be a hurdle for some international medical graduates, but it is absolutely a trainable skill.
For abstracts:
- Follow word and structure limits exactly (background, methods, results, conclusion).
- Prioritize clarity over complex vocabulary.
- Ask a co-author fluent in academic writing to proofread.
For manuscripts:
- Use a standard structure (IMRAD: Introduction, Methods, Results, Discussion).
- Read 3–5 recent papers from your target journal before writing.
- In the Discussion:
- Compare your findings with prior literature.
- Highlight clinical relevance.
- Acknowledge limitations honestly.
Take advantage of:
- Institutional writing centers or editorial services.
- Mentor feedback with track-changes.
- Tools for grammar and style checking.
Publishing even a few well-written papers as an IMG significantly enhances your profile and credibility heading into faculty recruitment or visas that value “extraordinary ability.”
Strategically Using Research to Shape Your Future Career
Radiation oncology offers diverse paths: pure clinical practice, hybrid clinician–researcher roles, or heavily research-focused careers. Research during residency can help you position yourself for any of these.
Path 1: Clinician-Educator With Selective Research Involvement
If you envision a primarily clinical career (including community practice), focus your research energy on:
- QI projects that improve workflow and safety
- Practical outcomes research that directly affects your local practice
- Limited but meaningful publications demonstrating critical thinking
For this path:
- Aim for 2–4 solid publications by graduation.
- Emphasize your ability to participate in multi-center trials and implement evidence-based protocols.
Path 2: Academic Clinical Faculty (Hybrid)
This is a common goal for IMGs pursuing an academic residency track:
- 60–80% clinical, 20–40% research/teaching.
- Involvement in clinical trials, resident research projects, guideline committees.
For this path:
- Build a coherent “research narrative” (e.g., SBRT outcomes and toxicity, CNS reirradiation, global oncology).
- Target:
- 4–8 publications
- First-author work
- National conference presentations (ASTRO, ASCO, ESTRO)
- Seek mentors who are established academic clinicians and ask about their own time allocation, funding, and expectations.
Path 3: Physician-Scientist or Trials Leader
This path is more research-heavy (e.g., running phase I/II trials, lab-based translational work, or large-scale data science projects).
For this path during residency:
- Prioritize:
- High-impact projects with strong mentors
- Early exposure to trial design and translational science
- Consider a dedicated research year (if your program allows) or post-residency fellowships (e.g., in clinical trials methodology, health services research, or lab-based oncology)
As an IMG, you must also think about:
- Visa compatibility with grant funding (some awards require citizenship or permanent residency).
- Strategic selection of institutions with a track record of supporting IMGs into successful research-focused faculty roles.
Frequently Asked Questions (FAQ)
1. I’m an IMG with little prior research experience. Is it too late to start during residency?
No. While prior research helps with the rad onc match, residency is still an excellent time to develop a strong research profile. Start with small, well-defined projects under experienced mentors. Focus first on learning basic study design, literature review, and data management. Within 1–2 years, you can build toward more complex resident research projects.
2. How many publications do I “need” by the end of radiation oncology residency?
There is no fixed number, but a reasonable target for an IMG interested in an academic residency track or academic career might be:
- 3–6 peer-reviewed publications (including co-authorships)
- Evidence that you led at least 1–2 projects (first authorship)
- Several conference abstracts/posters at national or international meetings
Quality, relevance, and coherence of your work often matter more than absolute volume.
3. I struggle with academic English writing. How can I improve as an IMG?
Use a structured approach:
- Read several articles from your target journal to learn style and tone.
- Draft in simple, clear sentences; avoid overly complex language.
- Have a trusted co-author or mentor review your work.
- Use institutional writing centers and, when allowed, language editing tools.
- Over time, keep a personal “phrase bank” of useful academic sentences (e.g., how to introduce a topic, mention limitations, or compare with prior work).
Consistency and repeated practice across multiple manuscripts will significantly improve your writing skills.
4. How can I balance research, clinical work, and board exam preparation?
Plan longitudinally:
- Start simple projects early in residency when board pressure is lower.
- Use quieter clinical months to push manuscripts and IRB submissions.
- In the year before board exams, shift toward writing and completing existing projects rather than starting new, large endeavors.
- Protect weekly time blocks for research, even if short (1–2 hours), and communicate openly with mentors about your exam timeline.
Research during residency should support, not jeopardize, your primary goal: becoming an excellent, safe, and thoughtful radiation oncologist.
By approaching research during residency deliberately—as a set of skills to be built, relationships to be nurtured, and a narrative to be shaped—you, as an international medical graduate in radiation oncology, can emerge from training with a portfolio that opens doors in academia, clinical leadership, and global oncology for years to come.





















