
Are Community Programs an Untapped Resource in Healthcare Education?
Introduction: Why Community Programs Matter for Future Physicians
Healthcare is shifting faster than many training models can keep up. Rising costs, widening health disparities, increasingly diverse patient populations, and workforce shortages are reshaping what it means to be a well-trained clinician. Traditional hospital- and classroom-based training—while essential—often doesn’t fully prepare residents and students for the realities of outpatient care, social determinants of health, and complex community needs.
This is where community programs come in.
Community-based health initiatives—run by clinics, nonprofits, faith groups, public health departments, and neighborhood organizations—represent a powerful but underutilized arm of Healthcare Education. When intentionally integrated into medical training, these programs can:
- Deepen understanding of Public Health and social determinants
- Build skills in Patient Engagement and communication
- Strengthen Cultural Competency
- Provide low-cost, high-yield practicum and leadership experiences
- Improve local health outcomes while training future clinicians
For residency applicants and medical students, thoughtfully engaging with community programs can also demonstrate maturity, service, and alignment with program missions—especially in primary care, pediatrics, psychiatry, family medicine, and community-focused specialties.
This article explores how community programs function, what makes them distinct from academic settings, their benefits and challenges, and practical ways you can integrate them into your development as a future physician or healthcare professional.
Understanding Community Programs in Healthcare Education
What Are Community Programs in a Healthcare Context?
Community programs are organized, often locally driven initiatives designed to address the health needs, behaviors, and conditions of specific populations. They may be led by health systems, community-based organizations, schools, religious institutions, or local governments and can function in both urban and rural settings.
These programs bridge clinical care and Public Health by focusing on prevention, education, and access. They’re typically:
- Place-based: Focused on specific neighborhoods, towns, or demographic groups
- Needs-driven: Built around local health data and community voices
- Collaborative: Involving partnerships among clinicians, educators, public health agencies, and community leaders
- Practical: Focused on real-world outcomes like improved screening rates, medication adherence, diet, activity, or mental health support
For students and residents, community programs offer a front-row seat to how health and illness play out beyond the hospital walls.
Common Types of Community Health Programs
Below are some high-yield examples that intersect directly with Healthcare Education and training:
Health Outreach & Screening Initiatives
These programs target common conditions and health disparities:
- Free or low-cost blood pressure, glucose, or cholesterol screenings in churches, barbershops, or community centers
- Mobile clinics providing women’s health services, vaccinations, or HIV testing
- School-based programs addressing asthma management, obesity, or mental health
Educational opportunity: Learn motivational interviewing, brief counseling, risk communication, and population health approaches while engaging real patients in non-traditional clinical settings.
Culturally Tailored Education & Cultural Competency Workshops
These initiatives address cultural, linguistic, and systemic barriers to care:
- Programs teaching clinicians about cultural norms related to childbirth, end-of-life care, or mental health stigma in specific communities
- Bilingual or multilingual health education classes (e.g., prenatal classes in Spanish, diabetes education in languages spoken locally)
- Workshops co-led by community leaders, faith leaders, or promotoras (community health workers)
Educational opportunity: Deepen Cultural Competency and learn how to adapt counseling and care plans to patient values, beliefs, literacy levels, and social realities.
Mentorship, Pipeline, and Youth Programs
Designed to increase diversity and representation in the health professions:
- High school or college mentorship programs pairing students with clinicians in community clinics
- Summer programs introducing underrepresented students to clinical work and Public Health
- Shadowing programs in community health centers, FQHCs, and free clinics
Educational opportunity: Develop teaching, mentorship, and leadership skills while supporting the future healthcare workforce.
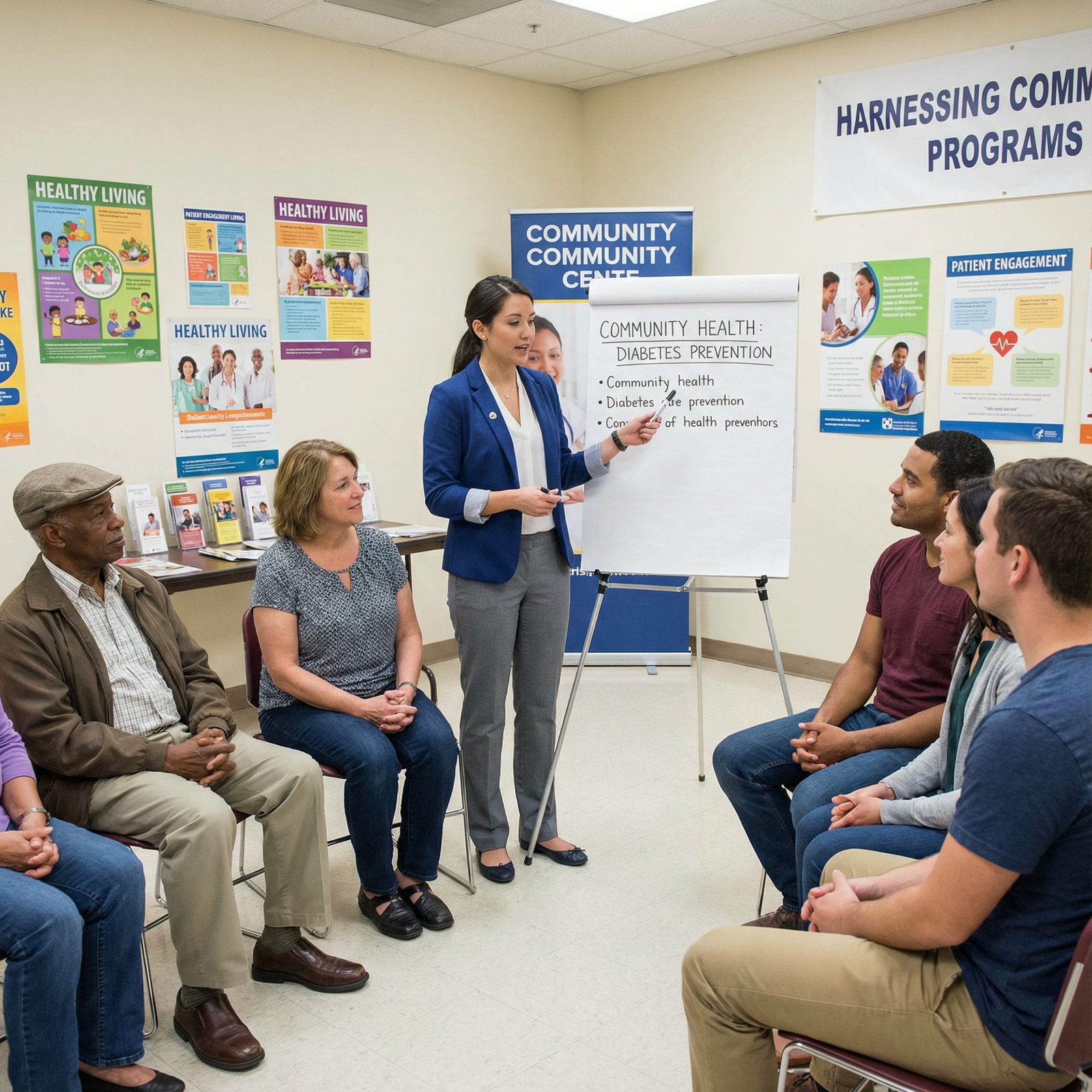
Disease-Specific Community Programs
Focused on high-priority local conditions:
- Smoking cessation groups run at community centers
- Peer-led diabetes prevention programs
- Community-based mental health peer support groups
Educational opportunity: Learn chronic disease management strategies, group visit models, and patient self-management support.
Community Programs vs. Academic Institutions: Complementary, Not Competing

Different Structures, Different Strengths
Academic medical centers and residency programs excel at:
- Delivering standardized, evidence-based curricula
- Training in pathophysiology, diagnostics, operations, and advanced procedures
- Managing complex inpatient and specialty-level care
However, they can be limited in:
- Exposure to uninsured or underinsured populations
- Understanding of neighborhood-level barriers (transportation, housing, food access)
- Hands-on experience with community-based prevention and health promotion
- Longitudinal follow-up with patients in their real-world environments
Community programs, in contrast, tend to:
- Be more flexible and responsive to local needs
- Focus on prevention, education, and behavior change
- Engage patients in their own homes, schools, and neighborhoods
- Utilize community leaders, peer educators, and non-traditional health workers
For Healthcare Education, the most robust training combines both: rigorous academic learning plus grounded community experiences.
Why This Matters for Residency Applicants
Programs—especially community-based and hybrid academic-community residencies—want trainees who:
- Understand health systems and community resources
- Recognize the impact of social determinants and structural inequities
- Show commitment to service and community engagement
- Can partner effectively with multidisciplinary teams and community stakeholders
Meaningful involvement in community programs can differentiate your ERAS application, your personal statement, and your interview answers. It provides concrete stories of Patient Engagement, advocacy, and interprofessional collaboration.
Key Benefits of Community Programs for Healthcare Education
1. Addressing Local Health Needs and Disparities
Community programs are uniquely positioned to respond to local epidemiology and disparities that may not be as visible from an inpatient ward.
Examples:
- A rural area with high rates of opioid use disorder develops a program combining naloxone training, MAT referral pathways, and peer recovery support.
- A predominantly immigrant neighborhood creates a perinatal health program addressing nutrition, breastfeeding norms, and immigration-related stressors.
- A community with high cardiovascular mortality establishes faith-based blood pressure screening and hypertension education events.
For trainees, this helps you:
- See how neighborhood, policy, and socioeconomic context shape disease patterns
- Understand Public Health principles like needs assessment and community engagement
- Learn to tailor interventions and communication strategies to specific populations
You move from asking, “What’s the guideline?” to also asking, “What will actually work for this community?”
2. Strengthening Patient Engagement and Trust
Community programs excel at building trust—something you cannot learn from a textbook.
They often:
- Employ community health workers, promotoras, or peer educators who share lived experience with participants
- Operate in trusted spaces: churches, community centers, schools, shelters
- Emphasize shared decision-making and respect for cultural norms
For you as a learner, this environment is ideal to practice:
- Active listening and non-judgmental communication
- Explaining diagnoses and plans at appropriate literacy levels
- Exploring barriers such as stigma, fear of the healthcare system, or past negative experiences
These skills are fundamental to effective Patient Engagement and will serve you in any clinical setting.
3. Encouraging Collaboration Across Local Systems
Community programs usually sit at the intersection of multiple institutions:
- Hospitals and clinics
- Public Health departments
- Nonprofits and advocacy groups
- Schools, faith-based organizations, and social services
Participating in these collaborations exposes you to:
- Interdisciplinary and interprofessional teamwork
- How policy, funding, and regulations influence health delivery
- Referral networks and care coordination beyond the hospital
For example, a community mental health promotion initiative might bring together:
- Family doctors and psychiatrists
- School counselors and social workers
- Peer support specialists and community organizers
- Residency trainees helping with psychoeducation groups
Learning to navigate these relationships prepares you for real-world practice, particularly in primary care, psychiatry, pediatrics, and community-focused specialties.
4. High-Impact Practicum and Longitudinal Experiences
Community programs can provide hands-on learning that complements formal rotations:
- Conducting home visits with community health workers
- Leading group education sessions (e.g., diabetes or prenatal classes)
- Designing and implementing small quality improvement or outreach projects
- Participating in neighborhood health assessments or research
These experiences sharpen skills in:
- Communication, counseling, and education
- Leadership, project management, and teamwork
- Community-based research and data interpretation
Residency programs increasingly value applicants who demonstrate these competencies. Longitudinal engagement (not just one-off volunteering) is especially impactful and easy to highlight on your CV and in your personal statement.
5. Cost-Effective, Accessible Education and Service
Community programs often run on:
- Grants and public health funds
- Philanthropy and local donations
- Volunteers, including students and trainees
This can make them:
- Accessible to low-income communities
- Approachable educational environments for students and residents
- Flexible sites for pilot projects, electives, and service-learning
For institutions, incorporating community programs into Healthcare Education can expand training opportunities without the high overhead of new clinical infrastructure.
Challenges and Limitations of Community Programs
While promising, community programs are not a panacea. Thoughtful engagement requires awareness of their constraints.
1. Limited and Unstable Funding
Many programs face:
- Short-term grants with uncertain renewal
- Staff burnout and turnover due to budget cuts
- Limitations in data collection and evaluation capacity
Implications for you:
- Projects may start strong and then lose resources
- You may need to adapt quickly, pivot roles, or redesign initiatives
- Sustainability should be a central part of any project you help design
However, this also creates opportunities to learn about grants, advocacy, and program evaluation—skills valuable in leadership roles.
2. Variability in Quality and Evidence Base
Unlike accredited academic curricula, community programs may:
- Lack standardized content or training for educators
- Use materials that are outdated or not evidence-based
- Vary widely in evaluation methods and outcome tracking
As a trainee, you can:
- Bring an evidence-based lens to help strengthen content
- Collaborate with faculty to create evaluation tools or QI methods
- Advocate respectfully for data-driven improvements
Some regions are working on accreditation or formal recognition pathways for community health worker training and community-based programs—an important development in enhancing quality.
3. Barriers to Participation and Equity
Even well-designed programs may struggle with:
- Low attendance due to work schedules, childcare, or transportation
- Limited accessibility for individuals with disabilities or limited literacy
- Distrust of healthcare systems, particularly in historically marginalized groups
You can help address these challenges by:
- Involving community leaders early and often in planning
- Using flexible formats (evenings, weekends, virtual options)
- Advocating for supports like childcare, transportation vouchers, or interpretation services
- Practicing humility and acknowledging historical and ongoing inequities
This is where Cultural Competency becomes not just a buzzword but a daily practice.
How to Leverage Community Programs in Your Healthcare Education and Residency Path
1. Partnering with Medical Schools and Residency Programs
Many institutions already have pathways you can plug into:
- Service-learning courses: Required or elective courses pairing didactics with community work
- Community-based electives or tracks: E.g., urban underserved, rural health, or Public Health–focused tracks
- Student-run clinics: Often embedded in community settings and serving uninsured populations
Actionable steps:
- Ask your dean’s office or GME office about existing community partnerships
- Seek faculty mentors involved in Public Health, family medicine, pediatrics, psychiatry, or internal medicine with community ties
- Propose integrating your community work into a scholarly project, poster, or publication
As a residency applicant, you can highlight these collaborations in ERAS under experiences, leadership, and scholarly activity.
2. Integrating Technology and Telehealth in Community Programs
Digital tools can greatly expand access and educational impact:
- Telehealth visits from community centers for patients lacking devices or broadband at home
- Virtual workshops on topics like hypertension, asthma, parenting, or stress management
- Text message–based programs reminding patients about medications, appointments, or healthy habits
- Online platforms for youth mentorship, career guidance, or mental health support
As a trainee, you can:
- Help design or facilitate virtual group visits or webinars
- Evaluate engagement data and help optimize workflows
- Learn best practices for telehealth etiquette, privacy, and rapport
Tech-enabled Community Programs align well with current healthcare trends and signal innovation on your CV.
3. Advocating for Policy and Structural Support
Sustainable community engagement requires supportive policies and funding structures, such as:
- Dedicated reimbursement for community health workers and preventive services
- Grants supporting Community Programs as part of healthcare transformation initiatives
- Policies that incentivize health systems to partner with communities (e.g., value-based care models)
Ways you can engage, even as a student or resident:
- Participate in advocacy days, write op-eds, or support local initiatives
- Join institutional committees focused on health equity or community engagement
- Include policy implications in your QI or scholarly work
Understanding the policy landscape makes you a more effective clinician and advocate, and resonates strongly with many residency program missions.
4. Training and Empowering Community Health Workers and Peer Educators
Community health workers (CHWs) and peer educators are central to many successful programs. They:
- Share cultural, linguistic, and lived experience with the populations they serve
- Bridge gaps between clinical teams and communities
- Support adherence, navigation, and behavior change
As a learner, you can:
- Co-teach or co-learn alongside CHWs
- Help develop training modules (e.g., for diabetes education, mental health first aid)
- Learn to integrate CHWs into care teams during your rotations
These collaborations:
- Improve Cultural Competency
- Enhance Patient Engagement
- Provide a model for how you might structure teams in your future practice
Practical Tips for Students and Residents: Turning Community Engagement into a Strength
- Be intentional, not performative: Choose a community commitment you can sustain over time rather than multiple brief, disconnected experiences.
- Reflect and document: Keep a log of cases, projects, and outcomes you were involved in. These become powerful examples for interviews and personal statements.
- Seek mentorship: Identify faculty or community leaders who can guide your involvement and provide letters of recommendation later.
- Align with your specialty interests: Pediatrics? Engage in school-based health. Psychiatry? Collaborate with community mental health or peer support groups. Internal medicine or family medicine? Work with chronic disease management or home visit programs.
- Connect to broader themes: In your residency application, frame your experiences around themes like health equity, Public Health, system-based practice, community partnership, and patient-centered care.
FAQ: Community Programs and Healthcare Education for Residency Applicants
Q1: How can involvement in community programs strengthen my residency application?
Meaningful community engagement signals to program directors that you:
- Understand health beyond the hospital setting
- Care about health equity, prevention, and Public Health
- Have experience with Patient Engagement and Cultural Competency
- Can collaborate with diverse teams and work in low-resource environments
Highlight these experiences in your CV, personal statement, and interviews by emphasizing specific roles, outcomes, and what you learned about systems of care.
Q2: What types of community experiences are most relevant for competitive specialties?
It depends on the specialty, but as a guide:
- Primary Care (FM, IM, Pediatrics): Free clinics, chronic disease outreach, school health, home visits, Public Health partnerships
- Psychiatry: Community mental health programs, crisis centers, peer support groups, substance use outreach
- OB/GYN: Prenatal education programs, maternal health equity initiatives, family planning outreach
- Emergency Medicine: Mobile outreach units, harm reduction programs, injury prevention campaigns
- Surgical Specialties: Injury prevention, cancer screening programs, postoperative support groups
Programs care less about the “brand name” of the initiative and more about your depth of involvement, reflection, and impact.
Q3: How do I find reputable community programs to get involved with?
Consider:
- Your medical school or residency’s Office of Community Engagement or Service-Learning
- Local Public Health departments’ websites (often list active programs and needs)
- Federally Qualified Health Centers, free clinics, and community health centers
- Faith-based or nonprofit organizations focused on health, housing, or social services
- Faculty mentors with known interests in health equity or Community Programs
When in doubt, start with a conversation: ask how you can contribute in a way that respects existing structures and priorities.
Q4: How can I balance community work with demanding clinical and academic schedules?
Strategies include:
- Choosing longitudinal roles that require a few hours weekly or monthly
- Integrating community work into elective time, scholarly projects, or QI projects
- Using team-based approaches so responsibilities are shared and sustainable
- Setting clear boundaries and expectations with both community partners and your training program
Program directors understand time constraints; they value sustained, thoughtful involvement more than high volume.
Q5: What are common mistakes to avoid when engaging in community health programs?
Pitfalls to watch for:
- “Savior” mindset: Approaching communities with preconceived solutions rather than listening first
- Short-term, disruptive projects: Launching initiatives you can’t help sustain or hand off responsibly
- Ignoring local expertise: Overlooking the knowledge of community health workers, leaders, and participants
- Poor communication: Failing to close the loop with partners, share results, or acknowledge contributions
Focus instead on humility, partnership, sustainability, and transparency.
By embracing community programs as integral to Healthcare Education, you prepare yourself not only for residency, but for a career that is clinically excellent, community-responsive, and aligned with the realities of Public Health and patient lives. Community engagement is no longer “extra”—it’s essential training for the kind of physician today’s healthcare system needs.




















