
Understanding Work-Life Balance in Interventional Radiology as a DO Graduate
Interventional Radiology (IR) is often described as a “physician’s specialty” within radiology—highly procedural, clinically oriented, and increasingly longitudinal in patient care. For a DO graduate considering an interventional radiology residency, especially if you value lifestyle, work-life balance, and long-term sustainability, taking an honest look at the realities of IR is critical.
IR can offer a rewarding mix of hands-on procedures, problem-solving, and meaningful patient impact. At the same time, it is not what many would label a classic “lifestyle residency.” Understanding how duty hours, call, case acuity, and practice setting shape your day-to-day can help you decide if this path aligns with your personal and professional goals.
This article breaks down work-life balance in IR specifically for DO graduates, with an eye toward the osteopathic residency match landscape, training structure, and career options that can help you build a sustainable, fulfilling life in and out of the hospital.
1. Training Pathways for DO Graduates: How They Shape Work-Life Balance
Before you can judge residency work-life balance in IR, you need to understand how you actually get there as a DO graduate. The structure and length of your training directly impact your lifestyle during your late 20s and early 30s.
1.1 Interventional Radiology Training Models (Integrated vs Independent)
There are two main pathways to board certification in Interventional Radiology–Diagnostic Radiology (IR/DR):
Integrated IR Residency
- 6-year program (1 preliminary intern year + 5 IR/DR years, though some programs incorporate the intern year).
- Combines diagnostic radiology and IR training continuously.
- Typically:
- Years 1–3: Heavier diagnostic radiology (DR) rotations.
- Years 4–5: Increasing IR focus with heavier procedural and call responsibilities.
- Lifestyle gradation:
- Early years: More predictable daytime hours, some evening/weekend call for DR.
- Later IR years: More emergent procedures, longer days, and more frequent or intense call.
Independent IR Residency (after DR)
- Pathway: 1 clinical year + 4 years DR + 1–2 years IR.
- For DO graduates who match into DR first and then sub-specialize in IR.
- Lifestyle chronology:
- DR residency years: Often more structured, with call but fewer middle-of-the-night emergencies than IR.
- IR years: Concentrated procedural volume and higher acuity, so more variable hours and call demands.
For a DO graduate, the lifestyle impact is similar in both pathways by the time you’re a senior IR trainee: long procedural days, variable end times, and responsibility for acute patient issues. What changes is when that intensity ramps up and how early you commit to IR.
1.2 DO Graduate Residency Considerations: Osteopathic Pathways and Match Realities
With the single ACGME accreditation system fully implemented, DO and MD applicants enter the same osteopathic residency match/NRMP system. DO graduates now have very real access to both DR and integrated IR programs, but there are nuances:
- IR Match is competitive (IR match vs DR match):
- The IR match is significantly more competitive than diagnostic radiology alone.
- As a DO, you may face slightly higher barriers at some institutions with limited history of training DO residents—but this is improving steadily.
- DR-to-IR pathway for DO graduates:
- Many DO graduates successfully match into DR first, then pursue IR via independent residency or ESIR (Early Specialization in Interventional Radiology).
- This route may be more flexible and can offer a somewhat more predictable lifestyle during DR years before you fully take on IR intensity.
From a work-life balance standpoint:
- Integrated IR: Earlier and more continuous exposure to procedural call and IR workload, but more integrated training and early identity as an interventionalist.
- DR then IR: Slightly more measured lifestyle for the first 4–5 years, followed by more intense IR training; gives you time to confirm that the IR lifestyle fits you.
1.3 How Training Structure Affects Lifestyle
Key lifestyle implications:
- Length of Training:
IR/DR means you’re in training longer than many other fields—often 6 years post-graduation, not including any fellowship if pursued. That’s more years of resident-level salary and variable hours. - Duty Hours:
IR programs must adhere to ACGME duty hours (80-hour weekly average, one day off in seven, etc.). Nonetheless, your subjective workload can feel heavier because:- Procedures often run late.
- Emergencies can break up your off hours (especially during IR call).
- Flexibility and Autonomy:
As a senior IR resident, you’ll have less predictability in daily schedules compared to a pure DR resident who is primarily reading studies and doing scheduled procedures.
For a DO graduate prioritizing lifestyle, the structure of the training pathway—integrated vs independent—may be just as important as the specialty itself.
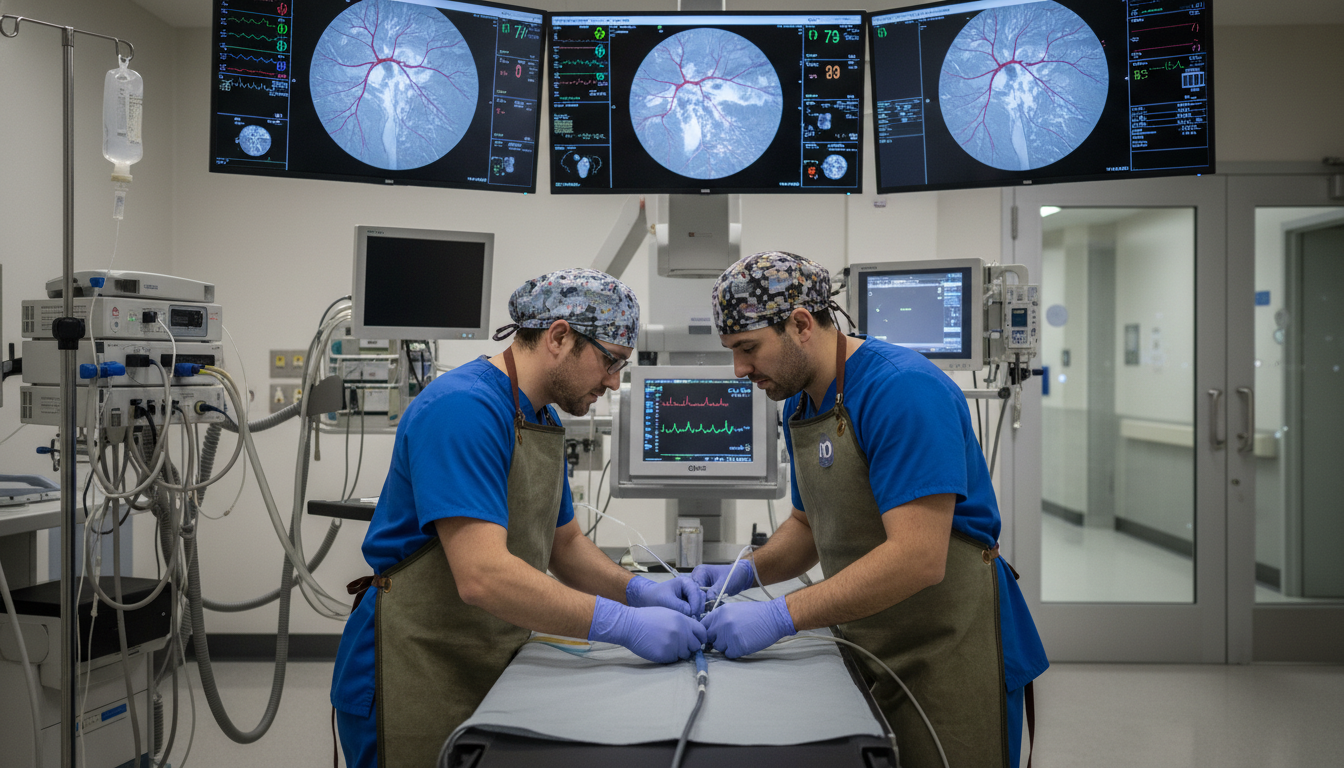
2. Day-to-Day Life in IR Residency: Hours, Call, and Case Mix
Work-life balance in an interventional radiology residency is less about a single number of hours and more about the texture of those hours: intensity, unpredictability, and emotional load.
2.1 Typical Duty Hours and Workload
While specific programs vary, here’s what many IR residents report:
- Weekday hours (IR-heavy rotations):
- Start: 6:30–7:30 a.m. (pre-rounds, check patient list, procedures set-up).
- End: 5:30–7:00 p.m., depending on case backlog and add-ons.
- Weekday hours (DR rotations within IR/DR):
- Often closer to 8:00 a.m.–5:00 p.m., with some later stays on busy services.
- Weekends:
- When on IR call: Can range from relatively quiet (a few consults, one or two procedures) to fully packed (bleeds, trauma, septic patients, emergent interventions).
- When off call: Typically off entirely, though some programs have DR weekend coverage for residents.
Although ACGME duty hours formally cap average weekly hours at 80, the nature of IR adds a layer of unpredictability that makes personal planning harder than in more controlled, “lifestyle residency” specialties.
2.2 Call Structure: The Biggest Lifestyle Variable
Call is one of the defining elements of IR lifestyle—both in residency and in practice.
Common call structures in IR residency:
- Home call:
You’re at home but carry the pager. You return to the hospital for emergent cases:- Active bleeding (GI bleeds, trauma, postpartum hemorrhage).
- Acute limb ischemia.
- Complicated drains or line placements.
- In-house call (less common for IR only):
Some programs with large hospitals or trauma centers may have IR residents in-house for night float, especially combined with DR call. - Frequency:
- 1 in 3 to 1 in 5 weeks on IR call is typical at many academic centers.
- Combined DR/IR call may increase the total number of nights you’re responsible for.
Lifestyle consequences:
- Sleep disruption:
Even if you’re on home call, a bleed at 3 a.m. means driving in, performing the case, and possibly staying through early morning rounds. - Unpredictable evenings/weekends:
It’s harder to commit to regular evening plans when any night might turn into an emergent embolization or trauma case. - Emotional intensity:
You often deal with critically ill, unstable patients—heavy responsibility, often with time pressure.
Compared to classic “lifestyle residency” options (like dermatology or certain outpatient specialties), IR call is clearly more intense and less predictable. But compared with many surgical fields, IR can be relatively more controlled, especially in settings where home call is the norm and in-house overnight coverage is rare.
2.3 Procedural vs Cognitive Load
Lifestyle in IR is also shaped by the type of work you do:
- Procedural load:
- Long cases (TACE, Y-90, complex vascular work).
- Multiple shorter cases (ports, drains, biopsies).
- Heavy concentration and motor coordination required.
- Cognitive load:
- Pre-procedure planning: reviewing imaging, assessing anatomy, risk, and approach.
- Post-procedure follow-up: managing complications, interpreting lab trends, coordinating with primary teams.
- Deciding when not to intervene—a key part of IR’s clinical role.
The combination of physical and mental fatigue is real. A full day of complex procedures can be more draining than a similarly long day of reading studies in DR.
As a DO graduate, your osteopathic training in whole-person care and clinical medicine can be an advantage—you are used to thinking clinically, which IR increasingly expects—but it also means you may naturally take on more longitudinal patient engagement, which can add hours and emotional load.
3. Interventional Radiology as a “Lifestyle Specialty”: Reality vs Perception
Interventional Radiology is almost never at the top of lists of “most lifestyle friendly specialties,” but it does offer certain characteristics that appeal to residents who want a balance between engaging work and time outside the hospital.
3.1 Where IR Sits on the Lifestyle Spectrum
Approximate lifestyle comparison:
- More lifestyle-friendly than:
- Many surgical residencies (neurosurgery, trauma surgery, orthopedics with heavy trauma, vascular surgery).
- Some acute care specialties with constant in-house call.
- Less lifestyle-friendly than:
- Outpatient-focused fields (dermatology, outpatient psychiatry, PM&R in certain settings).
- Non-procedural imaging-only careers (some DR-only positions, teleradiology).
In IR residency, you trade predictability for excitement and hands-on impact. The field is not lifestyle-maximized, but it can become lifestyle-balanced in the right practice setting post-training.
3.2 Practice Settings After Residency: The Key to Long-Term Work-Life Balance
Long-term work-life balance in IR is heavily dependent on where and how you practice:
Academic IR
- Pros:
- Structured rotations and academic scheduling.
- Subspecialization (e.g., oncologic IR, neuro-IR) can tailor the type of calls you take.
- Opportunities for research, teaching—intellectually rewarding.
- Cons:
- Often higher call burden and complex cases.
- More meetings, teaching responsibilities, and sometimes lower salary than private practice.
- Pros:
Private Practice IR/DR Hybrid
- Pros:
- Can mix DR reading days (often more predictable, shorter) with IR days (more intense but more satisfying procedurally).
- Potential for higher earnings, especially with procedural volume.
- Often more flexibility as senior partner in choosing call coverage and case mix.
- Cons:
- Early years as junior associate may mean higher call share.
- Business pressures can increase workload (productivity targets, RVUs).
- Pros:
Outpatient-based IR / OBL (Office-Based Lab) or ASC (Ambulatory Surgery Center)
- Pros:
- More control over hours—mostly daytime elective work.
- Fewer emergent cases, thus fewer middle-of-the-night call events.
- Increasingly popular for certain procedures (varicose veins, PAD, some pain procedures).
- Cons:
- May have less hospital-based acute care, which some find less rewarding.
- Business and administration responsibilities for those who own or run centers.
- Pros:
For many IR physicians, the post-residency practice type is the biggest determinant of long-term residency work life balance and career satisfaction. A DO graduate committed to IR but also to lifestyle can deliberately steer toward practice models that favor daytime elective work and controlled call.

4. Strategies for DO Graduates to Optimize Work-Life Balance in IR
If you are a DO graduate committed to interventional radiology but mindful of lifestyle, you’re not helpless. You can actively shape your trajectory—from how you apply to how you train and eventually practice.
4.1 Be Strategic in the IR and Osteopathic Residency Match
To navigate the osteopathic residency match and IR match in a way that supports balance:
- Consider DR-first if you want flexibility:
- Matching into DR, then pursuing ESIR or an independent IR residency, gives you:
- Time to assess whether the IR lifestyle fits.
- A viable exit route to a purely diagnostic or more lifestyle-oriented radiology path if desired.
- Matching into DR, then pursuing ESIR or an independent IR residency, gives you:
- Research program culture:
- Talk to current residents, including any DO graduates, about:
- Realistic duty hours and enforcement of duty-hour limits.
- Support on heavy call nights.
- Attending expectations for off-hours coverage.
- Talk to current residents, including any DO graduates, about:
- Value programs that protect resident wellness:
- Look for:
- Formal wellness initiatives.
- Clear policies on backup coverage when residents are overwhelmed.
- A history of residents finishing on time and not consistently exceeding duty hours.
- Look for:
4.2 Use Your DO Skill Set to Your Advantage
Your osteopathic background can be an asset in IR:
- Communication and rapport:
You’re likely comfortable with bedside interactions and holistic care—this helps build trust with acutely ill patients and families, which can reduce conflict and stress. - Clinical perspective:
IR is increasingly a clinical specialty; being comfortable managing fluids, sepsis, anticoagulation, and complex medical issues gives you confidence and may reduce your cognitive burden. - Self-awareness and body mechanics (from OMM training):
You can leverage your understanding of posture, ergonomics, and musculoskeletal health to protect your own body as you spend hours in lead and at the angio table.
These strengths can help you work more efficiently and sustainably, even when the hours are long.
4.3 Develop Routines and Boundaries Early
Practical steps to manage residency work life balance:
- Create non-negotiable personal routines:
- Short daily exercise (even 10–20 minutes) to counter long hours in lead.
- Pre-sleep wind-down routines after call to improve sleep quality.
- Protected time weekly for relationships or hobbies (even a few hours).
- Use time-blocking:
- During DR rotations, maximize learning and productivity to reduce after-hours study.
- During IR-heavy weeks, be realistic: aim for minimal but consistent exam prep, focusing on high-yield topics.
- Set communication boundaries where possible:
- When off call, clarify expectations with your team about when you can be reached.
- Avoid unnecessarily checking work email or messages during protected personal time when not on call.
4.4 Build a Supportive Network
Interventional radiology can be intense; having a support structure matters:
- Mentors in IR (especially DO IR attendings if available):
- Ask explicitly how they balanced training with family or personal commitments.
- Get advice on selecting rotations, fellowships, or first jobs that align with lifestyle goals.
- Resident peers:
- Share call experiences, rotate coverage fairly, and support each other in speaking up when duty hours or fatigue become unsafe.
- Non-medical support:
- Family, partners, and friends need realistic expectations of your schedule.
- Clear communication about call cycles and likely busy periods can reduce conflict.
4.5 Plan Ahead for Lifestyle-Friendly Practice Choices
As you move toward the end of residency:
- Think deliberately about what you want:
- Are you comfortable with a busy trauma center and frequent emergent call because you love acute care?
- Or do you prefer a primarily outpatient IR practice with elective procedures and minimal middle-of-the-night emergencies?
- Negotiate call and duty hours when job hunting:
- Ask specific questions:
- How many nights per month are typically on call?
- Is call home or in-house?
- What is the average number of callbacks per night or weekend?
- Clarify expectations about post-call days off or lighter schedules after intense call.
- Ask specific questions:
Your first job doesn’t have to be your last; you can pivot later into more lifestyle-focused IR settings or even a DR-heavy role if your priorities change.
5. Is Interventional Radiology the Right Balance for You as a DO Graduate?
Ultimately, the question isn’t, “Is IR a lifestyle specialty?” but rather, “Does IR offer a work-life balance that fits you, given your values, interests, and tolerance for intensity?”
5.1 Who Tends to Thrive in IR from a Lifestyle Perspective?
You may thrive in IR if:
- You enjoy procedural intensity and are energized rather than drained by acute cases.
- You appreciate a mix of cognitive and technical work and don’t mind late additions to the schedule.
- You like team-based care, working closely with surgeons, intensivists, oncologists, and hospitalists.
- You’re comfortable with variable days and can adapt when cases run long or emergent situations arise.
- You can set boundaries and maintain routines, even within an irregular schedule.
For many DO graduates—especially those drawn to hands-on work, clinical medicine, and patient relationships—IR can offer a deeply meaningful career, even if it’s not the easiest path in terms of duty hours.
5.2 When to Consider Alternate or Adjacent Paths
On the other hand, you might want to reconsider a purely IR trajectory if:
- You strongly prioritize predictable hours and minimal overnight or weekend responsibilities.
- You are uncomfortable with frequent high-acuity decision-making or the pressure of emergent interventions.
- Your personal life (e.g., major caregiving responsibilities) demands high schedule stability.
Adjacent options that can maintain a procedural/cognitive mix with more predictable lifestyle may include:
- Diagnostic Radiology with limited or no IR:
Many DR jobs now allow you to limit call and choose subspecialty focuses (e.g., body imaging, neuroimaging). - Other image-guided or procedural fields (e.g., some PM&R pain practices) with more outpatient focus.
- Lifestyle-oriented DR roles (teleradiology, part-time work) after finishing at least DR training, if you decide to pivot.
FAQs: Work-Life Balance in Interventional Radiology for DO Graduates
1. Is an interventional radiology residency considered a lifestyle residency?
No. Interventional radiology is not typically categorized as a “lifestyle residency” like dermatology or some outpatient specialties. IR involves variable hours, significant call responsibilities, and frequent emergent procedures. That said, compared with many surgical specialties, IR can offer more flexibility, especially if call is home-based and if you eventually choose an outpatient-focused practice. Long term, many IR physicians achieve a good residency work life balance, but it requires deliberate practice-setting choices.
2. As a DO graduate, is it harder to match into interventional radiology, and does this affect lifestyle?
The IR match is competitive for both MD and DO applicants. DO graduates may face additional challenges at some historically MD-dominated academic centers, but the gap has narrowed with the unified ACGME system. The main lifestyle implication is flexibility: many DO graduates strategically match into DR first, then pursue IR via ESIR or independent IR residency. This pathway can provide more predictable early training years and allows you to reassess whether the IR lifestyle truly fits before committing fully.
3. What kind of work-life balance can I expect after finishing an IR residency?
Post-residency lifestyle varies much more by practice type than by degree (DO vs MD):
- Academic tertiary centers:
More complex cases, frequent emergent work, and heavier call—often less predictable but very stimulating professionally. - Private practice IR/DR hybrid:
Mix of procedural days and reading days, with variable call; often better compensation and, over time, more control of your schedule. - Outpatient-based IR (OBL/ASC):
More daytime, elective work with minimal emergent call, often leading to a more classic “lifestyle” structure.
By choosing your practice setting and negotiating duty hours and call expectations, you can significantly shape your long-term work-life balance in IR.
4. Can I have a family or significant personal commitments during an IR residency?
Yes, many IR residents successfully balance training with marriage, parenting, or other significant personal commitments. However, it requires:
- Honest conversations with partners or family about call, duty hours, and unpredictability.
- Strong time management and the willingness to protect limited off-time.
- Choosing programs that are genuinely supportive of resident wellness, parental leave, and schedule flexibility.
Interventional radiology is demanding, but it is possible to build a meaningful life outside the hospital with careful planning, supportive relationships, and clear boundaries—particularly as you transition into a post-training practice that aligns with your lifestyle priorities.






















