Discover innovative problem-solving techniques for on-call residents, enhancing decision-making, emotional resilience, and collaboration under pressure.
Understanding the Realities of On-Call Medical Residency
On-call shifts in Medical Residency are more than just long hours and pager alerts; they are accelerated training in clinical judgment, leadership, and crisis management. These shifts compress learning, stress, and responsibility into intense blocks of time that can feel overwhelming—especially for interns and early residents.
Yet these same shifts are also where you sharpen your problem-solving skills, develop Emotional Intelligence, and learn to drive Healthcare Innovation at the bedside.
The Nature of On-Call Shifts in Modern Residency
On-call responsibilities vary by specialty and institution, but common elements include:
- Rapid triage and prioritization of multiple simultaneous issues
- Cross-coverage of patients you don’t know well
- Night float or 24-hour call with circadian disruption and fatigue
- Reduced staffing and limited immediate supervision
- Frequent interruptions from pages, consults, families, and nursing staff
Common On-Call Challenges:
High Patient Volumes
You might be covering multiple floors or services. A single hour can mean:- New admissions from the ED
- A sepsis alert
- A chest pain evaluation
- A family meeting request
Learning to prioritize and handle these demands systematically is critical.
Complex, High-Stakes Cases
Distinguishing “sick” from “not sick,” deciding who can wait, and recognizing subtle red flags are core skills. On call, you may face:- Deteriorating vital signs with unclear cause
- Complications from procedures performed earlier in the day
- Patients with multiple comorbidities and unclear code status
Limited Resources and Support
At night and on weekends:- Fewer senior staff are immediately available
- Ancillary services may be reduced or delayed
- Imaging and specialty consults may require stronger justification
Understanding this context helps you approach On-Call Challenges with deliberate problem-solving rather than constant firefighting.
Common Cognitive and Emotional Challenges on Call
Rapid Decision-Making Under Uncertainty
You will make important decisions with incomplete information:- Do you send the patient to the ICU now or monitor closely on the floor?
- Is this chest pain ACS, anxiety, or something else?
- Should you wake up your attending now or gather more data first?
Balancing thoroughness with urgency is a learned skill.
Team Dynamics and Communication Breakdowns
On call, miscommunication can quickly become a patient safety issue:- Unclear orders
- Incomplete handoffs
- Different mental models between nursing, residents, and consultants
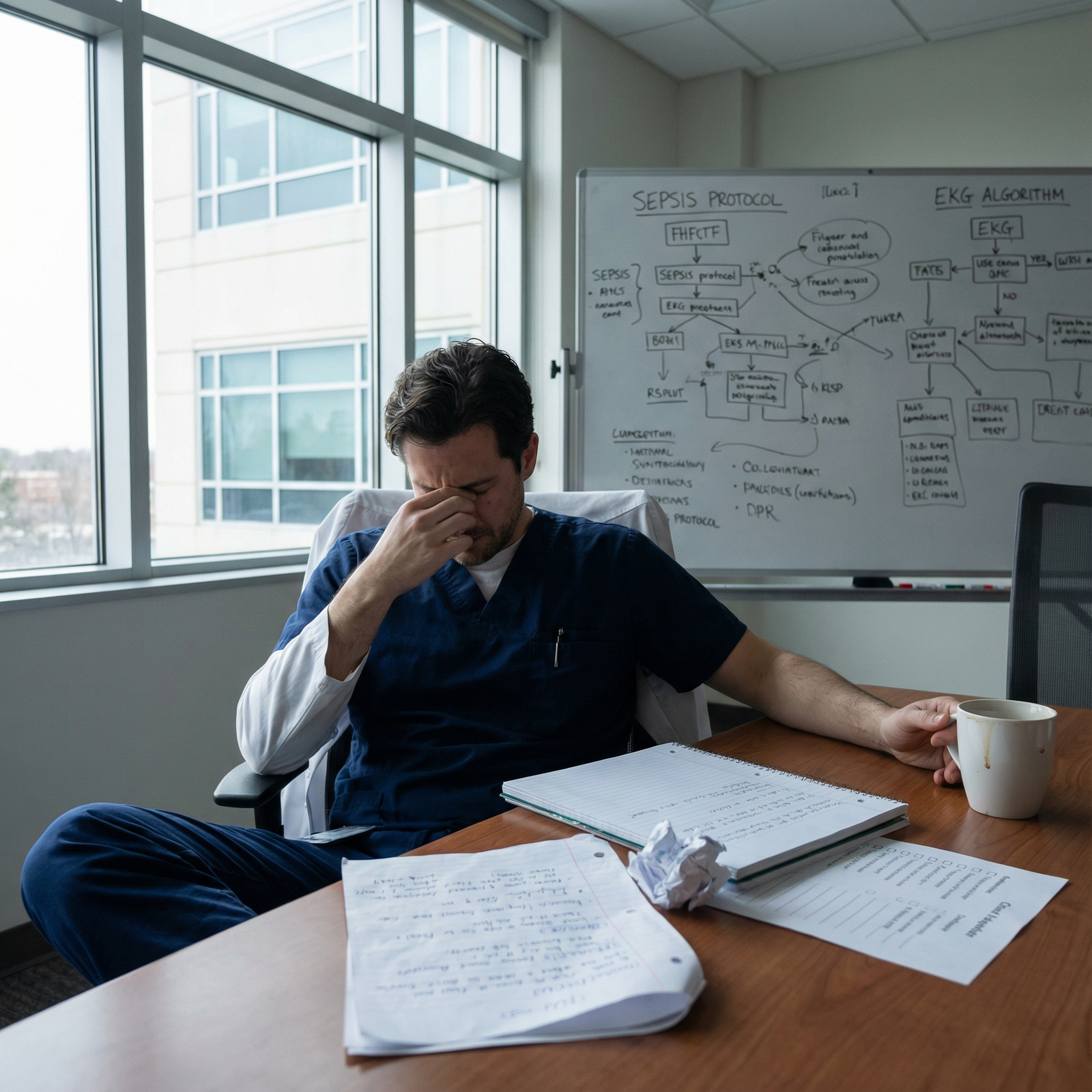
Fatigue, Stress, and Burnout Risk
Chronic sleep disruption, emotional load from adverse events, and pressure to perform can lead to:- Cognitive slowing
- Irritability and conflict with team members
- Decreased empathy and compassion fatigue
All of these realities make deliberate, innovative Problem-Solving essential during on-call duty.
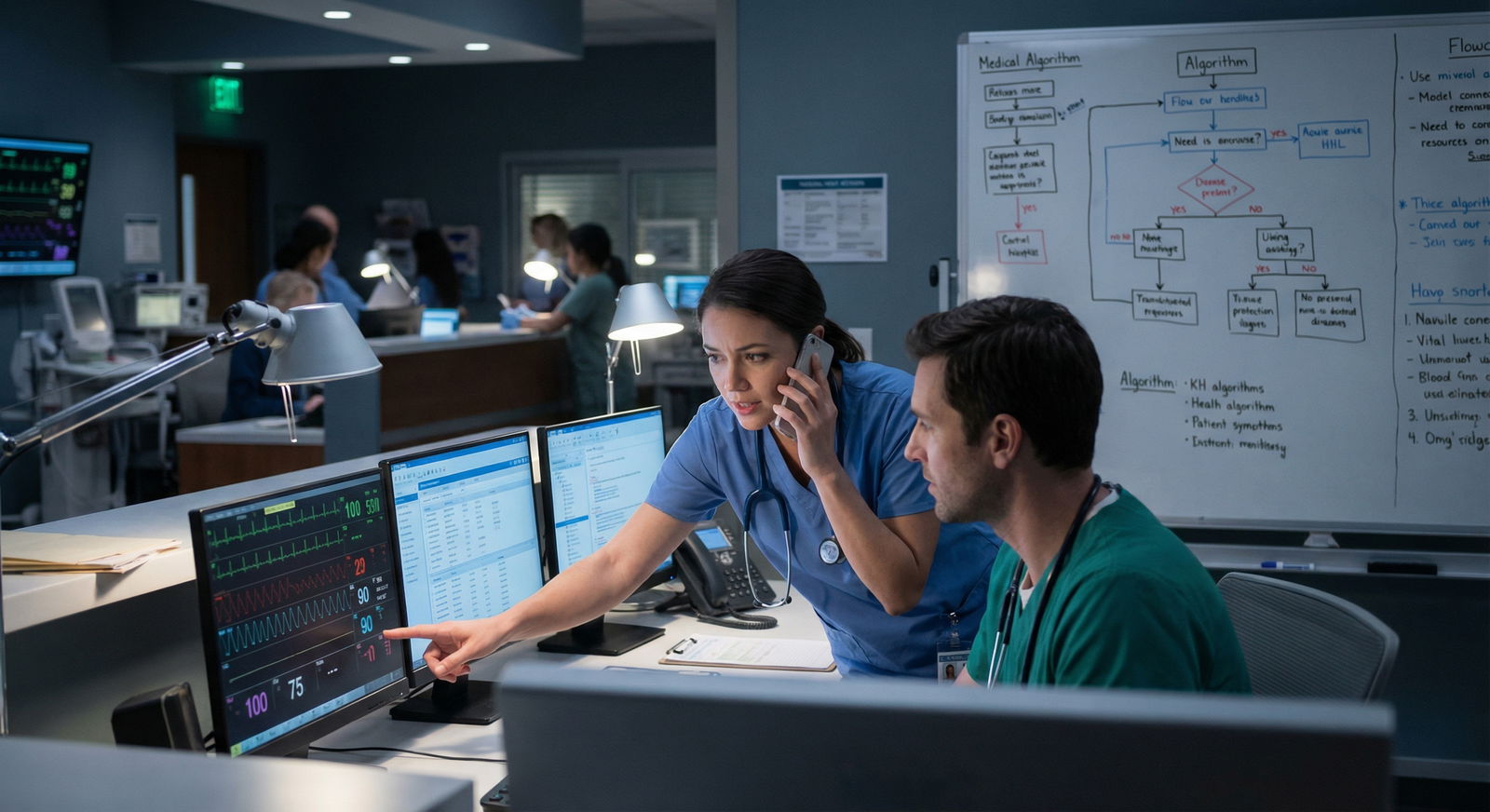
Leveraging Technology for Smarter On-Call Problem-Solving
Healthcare Innovation is reshaping the on-call experience. When used thoughtfully, technology can augment your clinical reasoning, streamline workflow, and reduce cognitive load.
Clinical Decision Support Tools
Digital tools should complement, not replace, your clinical judgment. Used strategically, they can significantly improve on-call performance.
Mobile Reference Apps (e.g., UpToDate, Medscape, Micromedex)
Practical uses on call:- Rapid review of treatment algorithms (e.g., management of DKA, sepsis)
- Checking dosing, renal adjustments, and drug interactions at 3 a.m.
- Refreshing diagnostic criteria for less common conditions
Strategy:
- Create “favorites” lists or saved topics for frequent on-call issues (chest pain, shortness of breath, fever, acute delirium, electrolyte abnormalities).
Institution-Specific Order Sets and Protocols
Many EMRs include:- Sepsis bundles
- Chest pain/ACS order sets
- Stroke or PE protocols
These structure your work, prevent omissions, and standardize care.
Clinical Calculators and Risk Scores
Use tools like:- Wells score for PE
- CHA₂DS₂-VASc for atrial fibrillation
- CURB-65 for pneumonia severity
- TIMI/GRACE scores for ACS
They support risk stratification and provide objective justification for your decisions when discussing with attendings or consultants.
Telemedicine and Real-Time Collaboration
Telemedicine is no longer only for outpatient care—it can be a valuable on-call problem-solving ally.
Remote Supervision and Consults
When your attending or fellow is off-site:- Share focused, structured presentations via secure video or phone
- Send images, EKGs, or case summaries through approved platforms
This can:
- Reduce delays in critical decisions
- Provide educational feedback in real time
- Increase your confidence while maintaining safety
Virtual Interdisciplinary Collaboration
Secure communication platforms can:- Enable group chats for complex cases (resident + nurse + pharmacist)
- Facilitate rapid clarification vs. multiple back-and-forth pages
Example:
- A patient with new AF with RVR: nurse, resident, and pharmacist coordinate a rate-control strategy and anticoagulation plan in one thread, minimizing delays and confusion.
Digital Organization and Cognitive Offloading
When you are covering many patients, your brain is not the best place to store every detail.
Digital To-Do Lists and Task Managers
Use EMR task lists or secure apps (if permitted by your institution) to:- Track pending labs and imaging
- Flag critical follow-ups (e.g., recheck potassium after replacement)
- Prioritize tasks (stat vs. urgent vs. can-wait)
Smart Use of EMR Dashboards
Configure:- Custom patient lists sorted by floor or acuity
- Columns for vital signs, labs, code status
- “Watch list” for unstable patients
This purposeful use of technology can transform chaotic on-call hours into more structured, manageable work.

Structured Decision-Making Frameworks for High-Stakes Nights
When the pager won’t stop and the stakes feel high, structured frameworks protect you from cognitive overload and tunnel vision.
The OODA Loop: A Practical On-Call Algorithm
The OODA Loop (Observe, Orient, Decide, Act) is a simple but powerful framework for on-call scenarios.
Observe
- Gather key data quickly: vitals, chief complaint, brief history, focused exam, immediate labs.
- Ask nursing: “What exactly made you call? What has changed?”
Orient
- Synthesize data: What’s the likely system involved (cardiac, respiratory, neurologic, metabolic)?
- Consider context: baseline status, comorbidities, code status, time course.
- Ask yourself: “Is this patient stable, unstable, or potentially crashing?”
Decide
- Choose an initial, reversible plan:
- Oxygen? Bolus? EKG? Stat labs? Call rapid response?
- ICU vs. stepdown vs. stay on floor?
- Make contingency plans: “If X worsens, I will Y.”
- Choose an initial, reversible plan:
Act
- Implement orders and interventions promptly.
- Communicate clearly with the bedside nurse and team.
- Reassess frequently and re-enter the loop with updated data.
Example:
A nurse calls about a patient with new hypotension.
- Observe: BP 80/50, HR 115, slightly confused, fever 38.7°C, recent pneumonia dx.
- Orient: Likely septic shock vs. hypovolemia; review I/Os and meds.
- Decide: Activate sepsis protocol, give fluids, broad-spectrum antibiotics, lactate, blood cultures, consider ICU transfer.
- Act: Place orders, call rapid response or ICU fellow, reassess within minutes.
SBAR: High-Yield Communication to Support Problem-Solving
The SBAR method (Situation, Background, Assessment, Recommendation) is a core tool for efficient and safe communication—especially on call.
Use SBAR when:
- Calling your senior or attending
- Contacting a consultant at 2 a.m.
- Clarifying concerns with nursing
- Giving handoffs to the next team
Example of SBAR to your attending:
- Situation: “I’m calling about Mr. Lee in room 432 with acute shortness of breath and hypoxia.”
- Background: “He’s a 68-year-old with CHF and COPD, admitted for volume overload, on day 3 of IV diuresis.”
- Assessment: “He’s now satting 86% on 4L, RR 28, BP 140/85, crackles at bases, mild wheeze, CXR suggests worsening pulmonary edema. I think he’s in acute CHF exacerbation, possibly over-diuresed earlier then rebounded.”
- Recommendation: “I’d like to start BiPAP, give IV furosemide, repeat labs including BNP, and get ICU involved. Does that sound reasonable?”
Structured frameworks like OODA and SBAR help ensure you’re thorough, organized, and clear—especially when tired and under pressure.
Checklists and Micro-Algorithms
Create or adopt short, practical checklists for common on-call scenarios:
Altered Mental Status:
- Check vitals, glucose, oxygen
- Review meds (opioids, sedatives, new psych meds)
- Rule out infection, metabolic disturbances, stroke red flags
Acute Chest Pain:
- ABCs, vitals, O₂
- EKG within 10 minutes
- Troponin, chest X-ray, risk scores
- Consult cardiology early if high concern
Having these mental or written micro-algorithms reduces missed steps and speeds up decision-making.
Emotional Intelligence: The Hidden Superpower On Call
Technical skills and protocols matter, but Emotional Intelligence (EI) often determines how effectively you navigate complex on-call situations, lead teams, and maintain your own well-being.
Self-Awareness and Self-Regulation
Recognizing your internal state in real time can prevent errors and relational conflicts.
Noticing Early Warning Signs
Pay attention to:- Irritability or snapping at colleagues
- Difficulty concentrating
- Impulsive decisions (“fine, just order everything”)
Micro-Resets During Shifts
When overwhelmed:- Take 60–90 seconds for slow, diaphragmatic breathing
- Step into a quiet hallway or call room for a short reset
- Mentally label your state: “I’m exhausted and anxious but still capable of thinking clearly if I slow down.”
These small interventions can refocus your Problem-Solving abilities when they matter most.
Empathy and Communication with Patients and Staff
On-call hours can bring emotionally intense situations: bad news disclosures at odd hours, distressed families, frustrated nurses.
With Patients and Families
- Use clear, jargon-free language.
- Validate emotions: “I can see this is really frightening. Let me walk you through what we’re doing.”
- Set expectations: “Tonight, my goal is to stabilize your breathing and control your pain. In the morning, your primary team will discuss the longer-term plan.”
With Nursing and Interdisciplinary Staff
- Acknowledge their concerns: “Thank you for calling—what’s worrying you most about this patient right now?”
- Avoid defensiveness when questioned; see it as shared responsibility for safety.
Good EI strengthens trust, which leads to better information flow and more effective team-based problem-solving.
Resilience and Burnout Prevention on Call
Resilience is not about being unaffected by stress; it’s about recovering and learning from it.
Post-Shift Debriefs
After a particularly difficult night:- Informally debrief with co-residents or seniors
- Reflect briefly: What went well? What could I improve next time?
- Seek specific feedback on challenging cases
Boundaries and Recovery
- Protect sleep time after call as much as possible
- Use days off intentionally for non-medical activities that restore you
- Know the signs of burnout and seek support early (program leadership, mental health services, peer groups)
Cultivating Emotional Intelligence not only helps you survive on-call duty—it positions you as a trusted, effective clinician and leader.
Team-Based Problem-Solving and Collaboration During On-Call Shifts
On-call problem-solving is rarely a solo act. Effective team dynamics dramatically improve safety, efficiency, and your own stress level.
Building Strong Relationships Before You’re On Call
Proactive relationship-building pays off when things get hectic.
Learn names and roles of:
- Charge nurses
- Pharmacists
- Respiratory therapists
- Unit secretaries
Ask about:
- Preferred communication methods
- Unit-specific workflows and pain points
This groundwork makes urgent collaboration smoother and less adversarial.
Fostering Psychological Safety on the Team
When people feel safe to speak up, they will alert you earlier to concerns—before patients crash.
You can promote psychological safety by:
- Inviting input: “Does anyone see something I’m missing?”
- Responding calmly to questions or challenges
- Thanking staff for calling early rather than only when things are dire
Simulation studies and real-world data both show that teams with high psychological safety identify and solve problems faster.
Efficient Interdisciplinary Huddles and Briefings
Even during busy nights, short, focused check-ins can be powerful.
Start-of-Shift Micro-Huddle (2–3 minutes)
- Ask the charge nurse about:
- Unstable or high-risk patients
- Anticipated admissions or discharges
- Share your plan: “I’ll prioritize these high-risk rooms early in the shift.”
- Ask the charge nurse about:
Case-Focused Huddles for Crises
For deteriorating patients:- Quickly gather bedside nurse, respiratory therapist, maybe charge nurse
- Clarify roles: who documents, who calls ICU, who prepares meds
- Use SBAR to align everyone on the current situation and plan
These small investments of time can prevent confusion and duplication of effort.
Resourcefulness and Adaptive Thinking with Limited Support
On call, you will frequently work with constraints. Adaptive Problem-Solving means learning to think like a “systems-aware” clinician, not just an individual provider.
Making the Most of Available Resources
Pharmacy as a Clinical Partner
- Ask for help with complex dosing, renal adjustments, drug interactions, or alternatives when formulary restrictions exist.
- Collaborate on anticoagulation plans, sedation regimens, and electrolyte correction.
Respiratory Therapy and Nursing Expertise
- Tap RT for nuanced assessment of respiratory distress and appropriate oxygen delivery or non-invasive ventilation.
- Ask experienced nurses what’s typical for a given floor and how similar cases have been handled.
Community and Post-Discharge Resources
Anticipate needs early:- Social work for high-risk discharges
- Home health nursing or physical therapy
- Outpatient follow-up with primary care or specialty clinics
Personal Systems: Checklists, Cards, and Quick References
Create your own “on-call survival toolkit”:
Pocket Reference Cards or Digital Notes for:
- Common medication starting doses and max doses
- Insulin regimens and sliding scales
- Management of hyperkalemia, hyponatremia, and acute GI bleeds
- Steps for rapid response / code situations
Standardized Sign-Out Templates
Use I-PASS or similar frameworks to:- Highlight patients most likely to decompensate overnight (“watcher” list)
- Clarify contingency plans: “If X, please do Y and call me if Z.”
Over time, this personal system design becomes a powerful, individualized Healthcare Innovation that keeps you organized and safe.
Frequently Asked Questions: Problem-Solving and On-Call Residency
Q1: How can I quickly improve my on-call decision-making skills as a new resident?
Focus on three things:
- Use structured frameworks like OODA for clinical decisions and SBAR for communication.
- Deliberately practice triage—each time your pager goes off, pause and mentally rank tasks by urgency and potential harm if delayed.
- Debrief after shifts—pick 1–2 challenging cases, review guidelines, and discuss them with a senior or attending to refine your approach.
Over weeks, this transforms isolated experiences into cumulative learning and sharper clinical judgment.
Q2: Which specific technologies are most useful during on-call shifts?
High-yield tools include:
- UpToDate, Medscape, Micromedex, or similar apps for rapid evidence-based guidance
- EMR-based order sets and alerts for sepsis, DKA, ACS, and stroke
- Secure messaging platforms approved by your institution for quick coordination with nurses, consultants, and pharmacists
- Clinical calculators (often embedded in apps or websites) for risk stratification and drug dosing
The key is to set these up in advance (logins, favorites, frequently accessed topics) so they’re instantly usable at 3 a.m.
Q3: How does Emotional Intelligence specifically improve on-call performance?
Emotional Intelligence helps you:
- Regulate your reactions when stressed, preventing escalation of conflicts with nurses or colleagues.
- Communicate clearly and empathetically with patients and families, even when you’re tired and under time pressure.
- Maintain situational awareness by recognizing when fatigue or frustration might be impairing your thinking and prompting you to slow down or seek help.
This leads to better teamwork, fewer errors due to miscommunication, and a more sustainable residency experience.
Q4: What are practical strategies to reduce burnout associated with on-call duties?
Evidence-informed strategies include:
- Prioritizing sleep hygiene on non-call nights and protecting post-call rest as much as possible.
- Using micro-breaks during call (even 1–2 minutes of deep breathing or stretching) to reset.
- Seeking connection with peers—informal check-ins and venting with co-residents normalize your experience.
- Debriefing emotionally difficult cases with mentors, program leadership, or mental health professionals rather than isolating.
- Clarifying your purpose—remind yourself periodically why you chose medicine and what kind of physician you want to become.
Q5: How can I become more resourceful in low-resource or understaffed on-call settings?
- Know your system: understand what services are available at night, who is on call for what, and how to reach them efficiently.
- Prioritize diagnostics that change management rather than ordering everything “just in case.”
- Leverage team expertise—ask experienced nurses or pharmacists how similar situations have been handled effectively in the past.
- Develop and refine personal checklists for recurring scenarios (e.g., hypotension, chest pain, confusion) so your approach remains systematic even when support is limited.
With time, this ability to creatively and safely adapt to constraints becomes one of your most valuable professional skills.
By combining technology, structured frameworks, Emotional Intelligence, collaborative teamwork, and personal resourcefulness, you can transform challenging on-call shifts into powerful training grounds. These experiences are not just about surviving the night—they are where you actively shape yourself into a thoughtful, resilient, and innovative physician.


















