In medical residency, few experiences shape your identity as a physician more than being on call. Night shifts, rapid responses, unexpected codes, and complex cross-cover pages test not only your medical knowledge, but also your organization, communication skills, and resilience.
While nothing replaces solid clinical training and good judgment, having the right emergency tools, systems, and habits can dramatically improve how you handle on-call emergencies. This guide expands on the core essentials every resident should have—physically and mentally—to manage on-call demands safely and efficiently.
Understanding On-Call Dynamics in Medical Residency
Being on call is much more than “being available.” It’s a high-stakes period where you must:
- Prioritize multiple patients and simultaneous emergencies
- Make urgent decisions often with incomplete information
- Coordinate with nurses, consultants, and ancillary services
- Document, communicate, and hand off care safely
What “On Call” Really Looks Like
Depending on your specialty and hospital, on-call duties can include:
- Covering multiple inpatient services overnight
- Responding to rapid response and code blue activations
- Admitting new patients from the emergency department
- Managing cross-cover issues (pain, fevers, hypotension, confusion)
- Fielding urgent consults from other teams
The unpredictability is what makes on-call particularly challenging. You may have a quiet hour followed by three stat pages, two admissions, and a code in close succession. The right emergency tools and systems help you stay ahead instead of constantly reacting.
Case Snapshot: A Realistic On-Call Evening
Imagine a typical Friday night:
- 19:30 – You start night float, receive sign-out on 30+ patients
- 20:15 – Page for chest pain on the floor
- 20:30 – New ED admission with sepsis
- 21:00 – Rapid response for hypoxia in another wing
- 21:30 – Nurse calls about a confused elderly patient trying to leave AMA
- 22:00 – You still haven’t eaten, and sign-out notes are incomplete
In this scenario, your medical knowledge matters—but your preparedness and tools determine whether this night is chaotic or controlled:
- A well-organized sign-out system prevents missed critical issues
- Emergency algorithms at your fingertips streamline decisions
- Reliable communication tools ensure help is quickly mobilized
- A simple self-care kit helps you maintain focus and avoid burnout mistakes
The following sections outline the core categories of Emergency Tools and Healthcare Resources every resident should assemble to thrive on call.
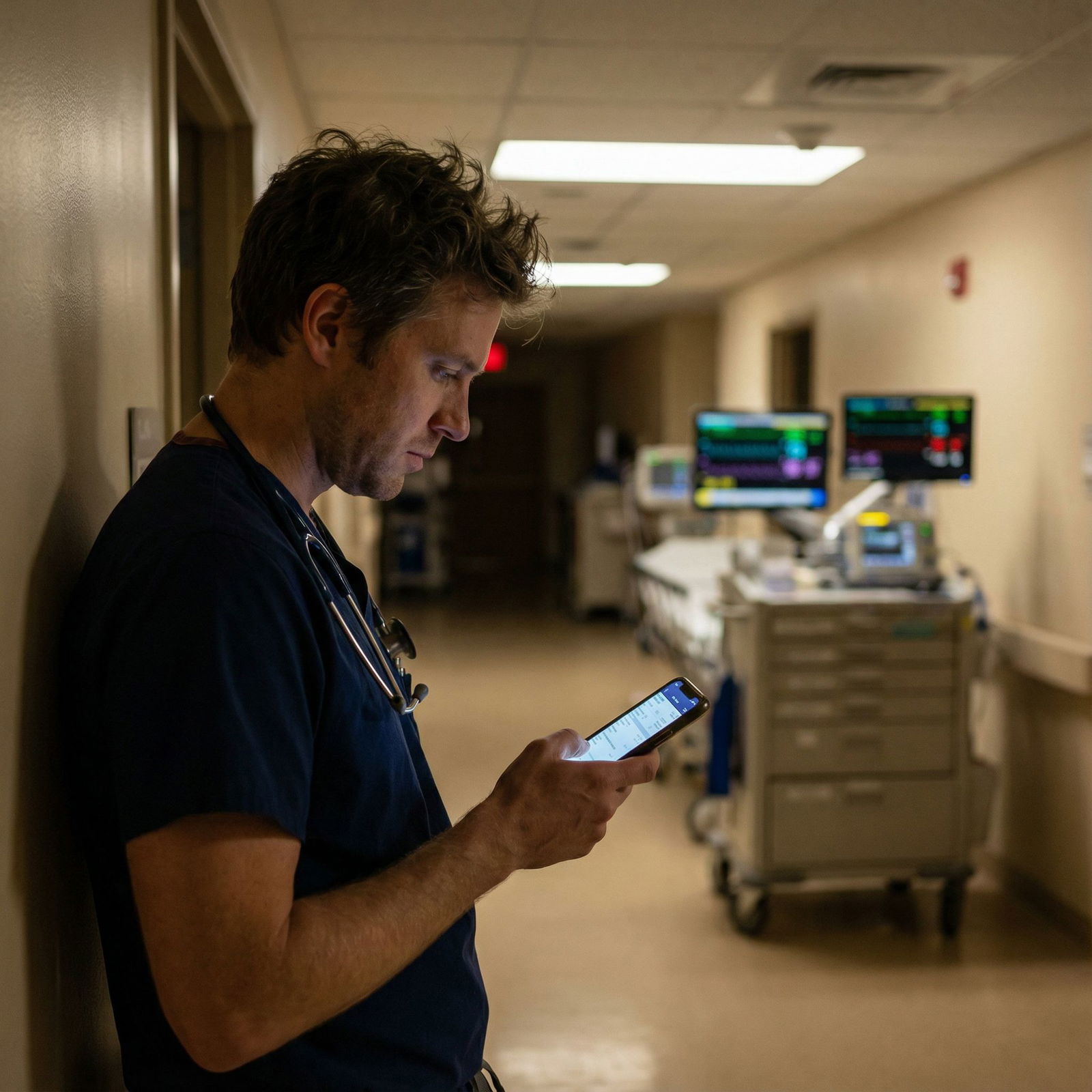
Digital Essentials: Mobile Medical Apps and Electronic Resources
In modern medical training, your smartphone and hospital computer access are as essential as your stethoscope. When used wisely, mobile medical apps and electronic tools are invaluable for safe and efficient on-call decision-making.
1. Clinical Knowledge and Guidelines Apps
These apps help you quickly access evidence-based information at the bedside:
UpToDate / DynaMed
- For: Clinical questions, diagnostic algorithms, treatment recommendations
- On-call examples:
- Checking latest management for new-onset atrial fibrillation in a septic patient
- Reviewing empiric antibiotic options for suspected meningitis
- Tip: Bookmark commonly used topics (e.g., DKA, sepsis bundles, ACS, stroke).
Medscape / Lexicomp / Micromedex
- For: Drug dosing, contraindications, interactions, side effects
- On-call examples:
- Double-checking renal dosing for vancomycin in a patient with AKI
- Confirming drug–drug interactions for a complex polypharmacy patient
2. Clinical Calculators and Risk Scores
Accurate dosing and risk assessment are crucial in urgent situations:
- MedCalc, MDCalc, or built-in EMR calculators
- For:
- Drug dosing (weight-based, renal adjustments)
- Risk scores (e.g., Wells, CHA₂DS₂-VASc, TIMI, CURB-65)
- Acid–base analysis, corrected sodium, anion gap, etc.
- On-call examples:
- Assessing PE probability to determine imaging urgency
- Calculating appropriate heparin or tPA dosing
- For:
Using these tools doesn’t replace understanding, but they reduce calculation errors when you’re tired at 3 a.m.
3. Emergency Protocol and Algorithm Apps
Fast reference to standardized protocols saves cognitive bandwidth:
Code / ACLS apps
- Contain: ACLS/PALS algorithms, defibrillation energy, drug doses
- On-call examples:
- Quickly confirming epinephrine dose in PEA arrest
- Reviewing tachycardia/bradycardia algorithms during a rapid response
Specialty-specific apps (e.g., EM, ICU, OB, pediatrics)
- Provide: Focused algorithms, normal value ranges, red flag symptoms
- On-call examples:
- Reviewing management of status epilepticus
- Checking pediatric dosing during a pediatric code or consult
4. Organizational and Task Management Tools
On call, information overload is your enemy. Use simple digital systems to stay organized:
- Secure to-do lists or note apps (if allowed by your institution)
- Organize tasks by priority, floor, and time
- Cross off items as they’re completed
- Password-protected sign-out templates
- Standardize information you track: code status, pending labs, key overnight issues
- Calendar and alarms
- Set reminders to recheck labs, repeat vitals, reassess unstable patients
Always follow your hospital’s privacy and security policies—never store identifiable patient data in non-approved apps.
Core Clinical Tools: Physical Examination and Point-of-Care Essentials
Even in an era of high-tech medicine, basic physical exam tools remain central to safe on-call care.
1. Stethoscope and Bedside Exam Kit
A high-quality stethoscope is non-negotiable, but consider building a compact exam pouch with:
Stethoscope
- Use consistently for lung, heart, and bowel sounds
- On-call examples: Distinguishing crackles vs. wheeze in dyspnea, new murmur in suspected endocarditis
Penlight
- For: Pupillary responses, oral mucosa, wound inspection
- On-call examples: Checking pupils in a new-onset confusion or head trauma
Reflex hammer and tuning fork (if neuro-heavy service)
- For: Focal neurologic exams, neuropathy assessment
- On-call examples: Evaluating unilateral weakness or suspected spinal cord involvement
Small notebook or index cards
- For: Jotting quick vitals, to-do items, differential diagnoses
- Many residents still prefer paper backup when EMR access is slow or distant.
2. Monitoring and Vital Sign Tools
In many hospitals, vital signs are nurse-collected, but residents still benefit from:
- Personal pulse oximeter (optional but useful in resource-limited or outpatient call)
- Familiarity with bedside blood pressure cuffs
- Helps when you need to quickly verify hypotension or a concerning reading
- Portable thermometer (in clinics or lower-resource environments)
The key is not necessarily owning this equipment, but being comfortable using it yourself when time is critical.
3. Practical Add-Ons for Efficiency
Small, low-tech tools can dramatically streamline your workflow:
- Multiple black and red pens
- Highlighter for key notes in printed sign-outs
- Badge card with quick references (common lab values, ACLS doses, normal ECG intervals)
- Small hand sanitizer bottle clipped to your pocket
These may seem trivial, but when you’re busy and moving between floors, every second and step matters.
Emergency Tools and Point-of-Care Testing: Rapid Diagnostics on Call
While residents don’t usually carry full “portable lab kits,” understanding and leveraging point-of-care (POC) testing and readily accessible emergency tools is essential.
1. Key Point-of-Care Tests You Should Master
Know what your hospital offers and where to find it:
Fingerstick glucose
- Critical in any altered mental status, seizure, or acute neuro change
- Always rule out hypoglycemia early—it’s fast, reversible, and often overlooked
Arterial or venous blood gas (with lactate when available)
- For: Respiratory failure, shock, unexplained acidosis
- On-call examples:
- Differentiating metabolic vs respiratory acidosis in a crashing patient
- Guiding oxygen and ventilation strategies
Rapid urine dip and pregnancy test
- For: Infectious workup, abdominal pain, AMS, pre-op assessment
- Always consider pregnancy testing in women of childbearing age with abdominal pain or hemodynamic instability
Rapid strep, influenza, COVID-19 (if available)
- Useful for ED-based call or urgent care shifts
2. Coagulation and Bleeding Risk Tools
You may not personally carry INR monitors, but you must know:
- Where urgent labs (CBC, PT/INR, PTT, fibrinogen) are processed
- Availability and location of:
- Reversal agents (vitamin K, PCC, FFP, idarucizumab, andexanet alfa)
- Massive transfusion protocols and how to activate them
On-call example: A patient on warfarin with head trauma and suspected bleed. Your emergency “tool” here is a combination of:
- Rapid labs
- CT imaging
- Reversal protocol knowledge
- Coordination with neurosurgery and pharmacy
3. Using POC Tools to Triage and Prioritize
POC tests help you quickly answer: “How sick is this patient, and how urgently do I need to act?”
- Hypotensive, tachycardic, febrile patient: Lactate and blood gas help determine if they require ICU-level care
- Shortness of breath on the floor: Bedside O2 saturation and quick exam differentiate anxiety from true respiratory distress
These diagnostic tools should be combined with your clinical judgment and escalation pathways (e.g., rapid response activation).
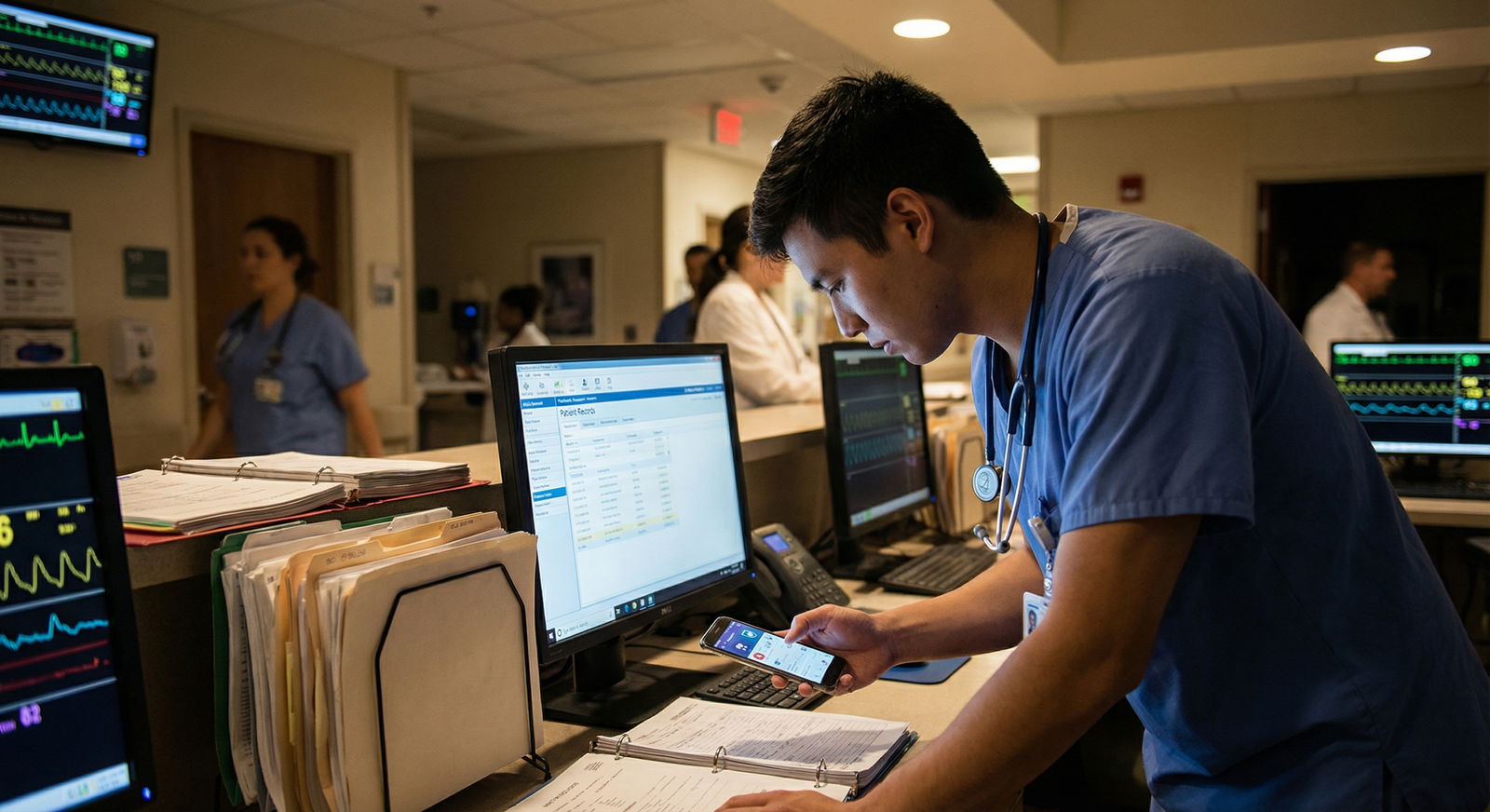
Communication, Documentation, and Team Coordination Tools
Safe on-call care is a team sport. Your communication and documentation systems are as important as your clinical gear.
1. Secure Messaging and Call Systems
Understand and master your institution’s communication infrastructure:
Secure messaging apps (e.g., TigerConnect, Epic Haiku/Canto messaging, Voalte)
- Use for: Non-urgent questions, clarifications, sending quick updates
- Benefits: Time-stamped, traceable, reduces lost pages
Pager or phone etiquette
- Respond promptly—even if just: “Received, will come see the patient after finishing current emergency.”
- Ask focused questions when paged: vitals, key symptoms, code status.
2. Structured Handoffs and Sign-Out Tools
A strong sign-out is one of the most powerful tools for on-call safety:
Use a standardized system (e.g., I-PASS):
- Illness severity
- Patient summary
- Action list
- Situation awareness and contingency plans
- Synthesis by receiver
On-call sign-out should clearly highlight:
- Code status and goals of care
- High-risk patients (unstable vitals, recent procedures, new diagnoses)
- Tasks to be completed overnight
- “If–then” plans (e.g., “If fever >38.5, draw blood cultures and start cefepime.”)
Good handoffs prevent you from being blindsided by preventable emergencies.
3. Note-Taking and Rapid Documentation Strategies
During a busy on-call night, documentation can feel overwhelming. Streamline it:
Use templates for common scenarios (e.g., cross-cover note, admission H&P, rapid response note)
Immediately jot key facts after an event:
- Time you were paged
- Vital signs
- Primary concern
- Initial differential
- Interventions and response
When possible, document critical interventions early:
- Code events, rapid responses, major medication changes
- Discussions about code status or goals of care
Robust documentation not only protects patients—it protects you and supports continuity of care.
Emergency Response Equipment and Hospital Resources
You are rarely alone during an on-call emergency. Knowing where equipment is, how to use it, and who to call is as important as the tools themselves.
1. BLS and ACLS Tools: What You Must Know Cold
Even if you’re not carrying this equipment personally, you must be intimately familiar with:
Code carts / crash carts
- Defibrillator and AED
- Emergency medications (epinephrine, amiodarone, atropine, etc.)
- Airway tools: Bag-mask device, oral/nasal airways, laryngoscopes (depending on specialty and institution)
ACLS and BLS protocols
- Cardiac arrest algorithms
- Tachycardia and bradycardia management
- Post-ROSC care basics
Walk through a code cart when you’re not under pressure. Knowing “top left drawer = airway,” “right side = fluids,” etc., reduces chaos during real codes.
2. Airway and Respiratory Support Resources
Early recognition of respiratory failure is critical:
Know where to find:
- Oxygen sources (wall O2, portable tanks)
- Bag-valve masks and appropriate mask sizes
- Suction equipment
- Non-invasive ventilation (CPAP/BiPAP) if within your scope and setting
Practice calling for help early:
- Respiratory therapy
- Anesthesia or ICU team
- Rapid response / critical care outreach
Your role may be initial stabilization and activating the right resources promptly.
3. Personal Protective Equipment (PPE)
Always treat PPE as a core emergency tool, not an afterthought:
Have easy access to:
- Surgical masks, N95 when indicated
- Eye protection / face shields
- Gowns and gloves
Use appropriate PPE especially for:
- Respiratory infections
- Known or suspected COVID-19, TB, or other airborne pathogens
- Body fluid exposure risks
Protecting yourself ensures you can continue to care for others—and models best practices for medical trainees and staff.
Quick Reference Guides, Cognitive Aids, and Mental Checklists
Under stress and fatigue, memory becomes unreliable. Cognitive aids and structured checklists are powerful tools in on-call emergencies.
1. Pocket Cards and Laminated Protocols
Consider carrying:
- ACLS algorithm cards
- Common drug dosing cards (e.g., code meds, sedation, analgesia)
- Specialty-specific cards (OB hemorrhage bundle, stroke codes, sepsis bundles)
These cheat sheets don’t weaken your knowledge—they reinforce correct action when seconds count.
2. Mental Models and Mnemonics
Develop and rehearse a few “go-to” frameworks:
- For altered mental status: AEIOU-TIPS
- For chest pain: OPQRST + risk factors
- For shortness of breath: “O’s” (Obstruction, Oxygenation, Overload, Obstruction PE, Others like anemia)
- For sepsis: “3 in 1” within first hour—blood cultures, broad-spectrum antibiotics, bolus fluids (per local protocol)
Use these to systematically structure your assessment and avoid missing critical diagnoses.
3. Simulation and Rehearsal as “Invisible Tools”
Regularly participating in simulation labs, mock codes, and case discussions sharpens your internal toolkit:
- Practice leading codes and rapid responses
- Drill on medication dosing under pressure
- Debrief after real events—what went well, what could be improved?
These experiences build the mental muscle memory that you’ll rely on when you’re the most senior person in the room at 3 a.m.
Resident Survival Kit: Self-Care Tools for Long On-Call Shifts
Your performance in on-call emergencies depends heavily on your own physiologic and mental state. A well-prepared survival kit is not a luxury—it’s a patient-safety tool.
1. Nutrition and Hydration
- Healthy, portable snacks
- Nuts, protein bars, fruit, yogurt, trail mix
- Avoid relying solely on sugary snacks or vending machines
- Water bottle
- Aim to keep it filled and visible at your workstation
- Dehydration worsens fatigue, headaches, and cognitive performance
2. Comfort and Energy Management Tools
- Compression socks to reduce leg fatigue
- Lightweight jacket or fleece for overly air-conditioned areas
- Blue-light filtering glasses if screen use is heavy at night
When you get a short break, use it intentionally:
- Five-minute walk or stretch rather than doom-scrolling
- Short breathing exercise (e.g., 4-7-8 breathing) to reset between crises
3. Cognitive and Emotional Support
No resident should face on-call pressures in isolation.
- Peer support network
- Co-residents, senior residents, chief residents
- Use them for clinical advice and emotional debriefing
- Know when to escalate concerns
- Call your attending earlier rather than later for unclear, unstable, or deteriorating patients
- Awareness of wellness resources
- Institutional counseling services
- Resident support groups or wellness committees
Supporting your mental health is directly connected to your ability to function with clarity and compassion on call.

Putting It All Together: Applying Your Tools in Real On-Call Emergencies
Consider a patient you’re called to see for new-onset respiratory distress on the floor:
Before entering the room
- Check recent vitals and trends in the EMR
- Ask the nurse brief, focused questions:
- “What changed?”
- “Any chest pain, fever, new meds?”
- “What’s their code status?”
Initial bedside assessment (using core tools)
- Use your stethoscope and pulse oximeter (if needed)
- Perform a rapid ABC assessment
- Apply supplemental oxygen and reposition the patient
Leverage point-of-care resources and protocols
- Order stat CXR and labs, consider POC gas if available
- Use your emergency app or pocket card to quickly review escalation pathways
- If unstable, activate a rapid response early
Communicate and coordinate
- Update your senior or attending if there is significant instability or diagnostic uncertainty
- Use secure messaging or phone calls for rapid updates to the team
- Document the event with a concise, focused note
Self-monitor
- After the event, take 1–2 minutes to reset: hydrate, take a breath, update your task list
- If the case was emotionally difficult (e.g., code or death), check in with peers or seniors
In every emergency, your effectiveness depends on an integrated system: medical knowledge + physical tools + digital resources + communication strategies + self-care.
FAQ: Tools and Strategies for Managing On-Call Emergencies in Residency
1. What are the most important emergency tools I should have on me during call?
At minimum, every resident should carry:
- Stethoscope
- Penlight
- Multiple pens and a small notebook or index cards
- Hospital ID/badge with access to secure systems
- Smartphone with approved medical apps and secure messaging (if allowed)
- Quick reference badge cards (ACLS algorithms, common doses)
The rest—such as POC testing and emergency equipment—is usually available on the unit, but you must know where it is and how to use it.
2. Which medical apps are truly essential for on-call emergencies?
Focus on a core set rather than dozens of apps:
- UpToDate or DynaMed for evidence-based clinical guidance
- Medscape / Lexicomp / Micromedex for medications and interactions
- MDCalc / MedCalc for risk scores and dose calculators
- An ACLS/code reference app
- Your hospital’s secure messaging or EMR app (e.g., Epic Haiku/Canto)
Use downtime early in residency to explore and bookmark common pages (sepsis, chest pain, stroke, DKA, anticoagulation).
3. How can I improve my communication and handoffs during on-call shifts?
- Use a structured handoff system like I-PASS
- Clearly identify sick/high-risk patients and specific contingency plans
- When paged, respond quickly and ask targeted questions
- Document critical conversations and interventions in real time when possible
- Debrief with seniors to refine your sign-out style and content
Good communication is one of the strongest predictors of safe on-call care.
4. Is self-care really that important during emergency-heavy call nights?
Yes. Self-care during call is a patient-safety intervention, not indulgence:
- Hunger, dehydration, and sleep deprivation worsen decision-making
- Brief, intentional breaks improve your ability to triage and think clearly
- Emotional processing after difficult events (like codes or deaths) reduces burnout and compassion fatigue
Even small habits—keeping a water bottle full, eating a quick healthy snack, stretching between tasks—can significantly impact performance over a long night.
5. How can I prepare myself before starting a new on-call rotation or service?
In the days before starting:
- Review key emergencies relevant to that specialty (e.g., sepsis for medicine, postpartum hemorrhage for OB, airway emergencies for anesthesia)
- Walk through the unit to locate:
- Code carts
- Oxygen and suction
- Crash buttons/rapid response activation methods
- Save or print laminated quick references
- Talk to senior residents: Ask, “What are the 3 most common overnight emergencies here, and how do you like to handle them?”
Proactive preparation transforms call from something you endure into an experience where you can grow, learn, and lead safely.
By thoughtfully assembling and using these Emergency Tools and Healthcare Resources, you equip yourself to meet the challenges of Medical Residency with greater confidence and control. On-call shifts will always be demanding—but with the right systems, tools, and support network, they become some of the most formative and rewarding experiences of your medical training.


















