
The fastest way to make specialists ignore your pages is to call them like an amateur.
You can be smart, hardworking, and clinically solid, and still get a reputation as “that resident” whose cross‑cover consults nobody wants to take. And reputations like that stick. People remember the 2 a.m. nonsense page far longer than your excellent note on rounds.
Let me walk you through the mistakes that quietly poison your relationships with consultants—and how to never be that person.
1. Paging Before You Know the Patient
This is the cardinal sin. Consultants hate getting called by someone who clearly has not looked at the patient yet.
Here’s the pattern I see over and over:
You’re cross‑covering nights. Nurse: “Hey, the team wanted nephrology to follow this patient. Can you page them?” You, drowning in pages, think, “Sure, I’ll just call and they can sort it out.” You page nephrology, they call back, and then:
“Uh… I haven’t seen the patient yet. I think they just wanted you to follow.”
That single sentence flags you as unreliable.
What goes wrong when you call too early:
- You cannot answer basic questions: vitals, creatinine trend, exam, urine output, meds.
- You look like you want the consultant to do your thinking.
- You waste their limited call time. And yes, they track who does this.
Do this instead:
- Open the chart. Always. At minimum: vitals, labs, meds, last note, problem list.
- See the patient if it’s remotely acute. I’ve watched cardiology hang up on “chest pain” consults where the caller admitted they hadn’t even laid eyes on the patient.
- Build your own one‑liner and differential first. Even if it’s wrong, it shows you did the work.
If you cannot honestly say “I’ve at least reviewed the chart and have a working impression,” you are not ready to call. You’re just handing off responsibility, and consultants smell that a mile away.
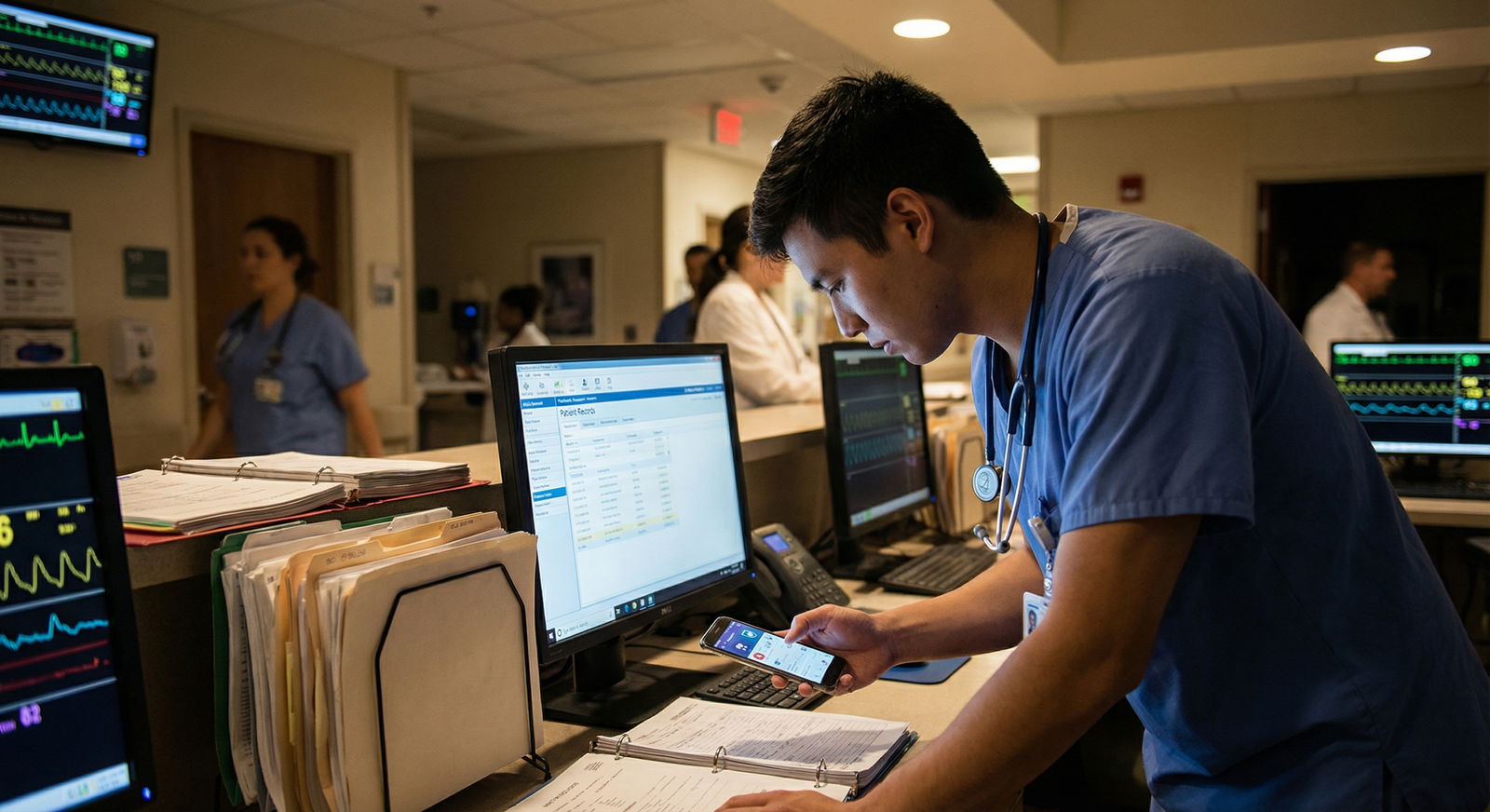
2. Vague, Rambling, or Disorganized Presentations
Consultants live or die by concise information. They’re fielding multiple services, multiple hospitals, and far too many pages.
The cross‑cover consult that kills your credibility sounds like this:
“Hi, I’m calling about a patient on 6E, um, they’re kind of complicated, came in a few days ago with, like, breathing issues, and now there’s some concern for maybe like a kidney thing or something, and I think the primary team wanted nephro following but I’m not really sure…”
They tune out after eight seconds.
You need a sharp, structured presentation ready before the callback. Something like:
- Who are you and what team?
- Urgency level (now vs tomorrow vs routine).
- One‑liner with reason for consult.
- Key supporting data.
- Specific question.
Here’s a simple framework that works across specialties:
“Hi, this is [Your Name], cross‑covering [Service]. I’m calling about a consult on [Patient, age, key comorbidities]. They’re admitted for [original issue]. We’re requesting [specialty] for [clear reason] in the setting of [key data]. Vitals are [X]. Labs and imaging show [Y]. My specific question is [Z].”
Specialists do not want your life story. They want the filtered signal. If they need details, they will ask.
Do not:
- Read the entire H&P.
- Walk through the chart chronologically from the ED.
- Apologize repeatedly for calling. It makes you sound insecure and unprepared.
You should be able to give a 20–40 second coherent summary without babbling. Practice it. Out loud. Residents who can’t present tightly get labeled as “difficult to deal with” no matter how smart they are.
3. “Non‑Consult” Consults (Calling for the Wrong Stuff)
Another way to make people refuse your pages: call for things that aren’t actual consults.
These look like:
- Paging ID at 2 a.m. to ask, “Can they get another day of ceftriaxone, or is three enough?” on a stable, non‑toxic patient where guidelines are clear.
- Calling cardiology just to interpret a routine EKG on a stable floor patient that you haven’t even looked at.
- Asking neurology to see someone with long‑standing diabetic neuropathy because “they still have pain.”
If the answer is in UpToDate, your hospital clinical guidelines, or the last consultant note from that same service, and the clinical situation hasn’t changed meaningfully, you probably don’t need a fresh consult.
Before you call, ask yourself three blunt questions:
- Has there been a real change in status or data since the last plan?
- Is there a decision here that’s beyond my training and resource set?
- Would I feel comfortable defending this consult to my attending tomorrow morning?
If the answer to all three is “no,” you’re likely abusing the consult system.
Do not let nurses or families pressure you into a needless consult without you doing your own assessment. “The family wants neurology to see them” is not an indication. You can say, “I evaluated, discussed with my senior, and we don’t think a new consult will change management tonight. We’ll update the day team.”

| Category | Value |
|---|---|
| Cardiology | 3 |
| Nephrology | 4 |
| Neurology | 3 |
| ID | 4 |
(Think of those numbers as “how often things are called for the wrong reason” in a typical night; they’re not exact, but you get the idea.)
Bottom line: Consults are for expertise you cannot safely provide, not for outsourcing basic residency‑level thinking.
4. No Clear Question (Or Ten Questions at Once)
Consultants hate the phrase “We just wanted you to be involved.”
Translation: “I have no idea what I want, and I’m hoping your note will magically solve everything.”
A consult without a question is just a turf transfer attempt. They know it. You know it.
You must have a focused question. Not five. Not “manage this whole thing.” One primary question. For example:
- “Should this patient with new Afib RVR and borderline pressure be rate or rhythm controlled, and what is your preferred strategy tonight?”
- “This patient’s sodium is 119, down from 128, asymptomatic. How aggressively should we correct overnight and with what fluids?”
- “Is there any further work‑up you recommend for this new seizure in a patient with known brain metastases, or is current management adequate until morning?”
If you cannot state your question in one sentence, you’re not ready to call.
The flip side: shotgun consulting. Where you page three services simultaneously for overlapping issues and then expect one of them to “take over.” Nothing annoys surgeons more than discovering GI, IR, and hospitalist have all been paged for the same bleeding issue without a thought about who’s actually best suited.
Pick the primary consultant based on the main organ system or most likely intervention. If in doubt, ask your senior or attending—not the consultant—to help decide.
5. Calling the Wrong Service (or Too Many Services)
You will absolutely burn goodwill if you repeatedly call the wrong specialty for the same type of problem.
Examples I’ve watched go badly:
- Calling neurology for a clear metabolic encephalopathy with normal CT and no focal signs, when the real issue is sepsis and sedation.
- Calling nephrology for “AKI” that’s obviously pre‑renal in a volume‑down patient you haven’t even tried to fluid.
- Paging surgery for chronic pain in a post‑op patient when the surgeons have already written a clear pain plan and there’s no change in exam.
The cross‑cover rule: fix what you can fix before you call.
If the blood pressure is low and the patient looks dry—give fluid.
If the sugar is 30—treat the hypoglycemia.
If O2 sat is 86%—address airway/breathing before you go consultant‑shopping.
Use this simple mental flow:

| Step | Description |
|---|---|
| Step 1 | New Issue on Call |
| Step 2 | Stabilize and Call Rapid Response or Senior |
| Step 3 | Assess Patient and Chart |
| Step 4 | Treat and Reassess |
| Step 5 | Identify Likely Organ System |
| Step 6 | Choose Most Appropriate Specialty |
| Step 7 | Formulate Clear Consult Question |
| Step 8 | Emergent? Airway, Breathing, Circulation |
| Step 9 | Within My Scope to Manage? |
If it’s emergent, you call rapid response / ICU / your attending first, then consultants. Nobody wants to hear, “Yeah, the BP was 60/30 when I paged cardiology, but I figured they’d tell me what to do.”
6. Disrespecting the Chain of Command
Cross‑cover is not license to freelance your own consulting empire.
Two landmines here:
- Overriding the primary team’s plan without discussion.
- Going directly to attendings while skipping fellows or residents.
“I know the day team didn’t want cardiology, but I called them anyway” is how inter‑service wars start. There are exceptions in true emergencies when the primary is unreachable, but that’s not most cases.
Default behavior:
- If you’re unsure whether to consult, page or call your senior.
- If the question is non‑urgent and the patient is stable, it’s often reasonable to leave it for the day team with a clear sign‑out: “Possible need for GI consult tomorrow for X; didn’t call overnight as patient stable and no change.”
- Follow the established contact pattern: consult resident → fellow → attending. Do not jump levels because you think the resident will say no.
Consult services talk to each other. “This intern always pages our attending directly” is exactly the kind of comment that shows up in back‑channel conversations and consensus opinions about you.
Respect the structure. It protects you more than you think.
7. Disregarding Urgency and Timing
Nothing irritates consultants more than your poor sense of urgency.
Two ways residents screw this up:
- Calling something STAT that isn’t.
- Sitting on something urgent until it’s a disaster.
If you label everything as “urgent” or “stat,” people stop believing you. Then one day you really do have a crashing patient, and nobody hustles because you’re the “always crying wolf” resident.
On the flip side, if you hold consults on truly concerning things just because you “don’t want to bother them at night,” and the patient tanks, that’s on you.
A rough guide:
- Call now (middle of the night) if:
- Active chest pain, new neuro deficits, airway/breathing/circulation issues, rapidly rising potassium, unstable arrhythmia, sepsis with unclear source, post‑op complication with acute change.
- Can wait for first thing in the morning if:
- Stable chronic issue, fine‑tuning long‑term meds, non‑progressive minor lab abnormalities.
| Situation | Call Overnight | Defer to Day Team |
|---|---|---|
| New focal neuro deficit | Yes | No |
| Chronic pain without change | No | Yes |
| K 6.5 with EKG changes | Yes | No |
| Stable chronic hyponatremia Na 129 | No | Yes |
| New afib with RVR and soft BP | Yes | No |
If you’re truly torn, wake your senior. That’s their job. Better to ask than to make a solo bad call.
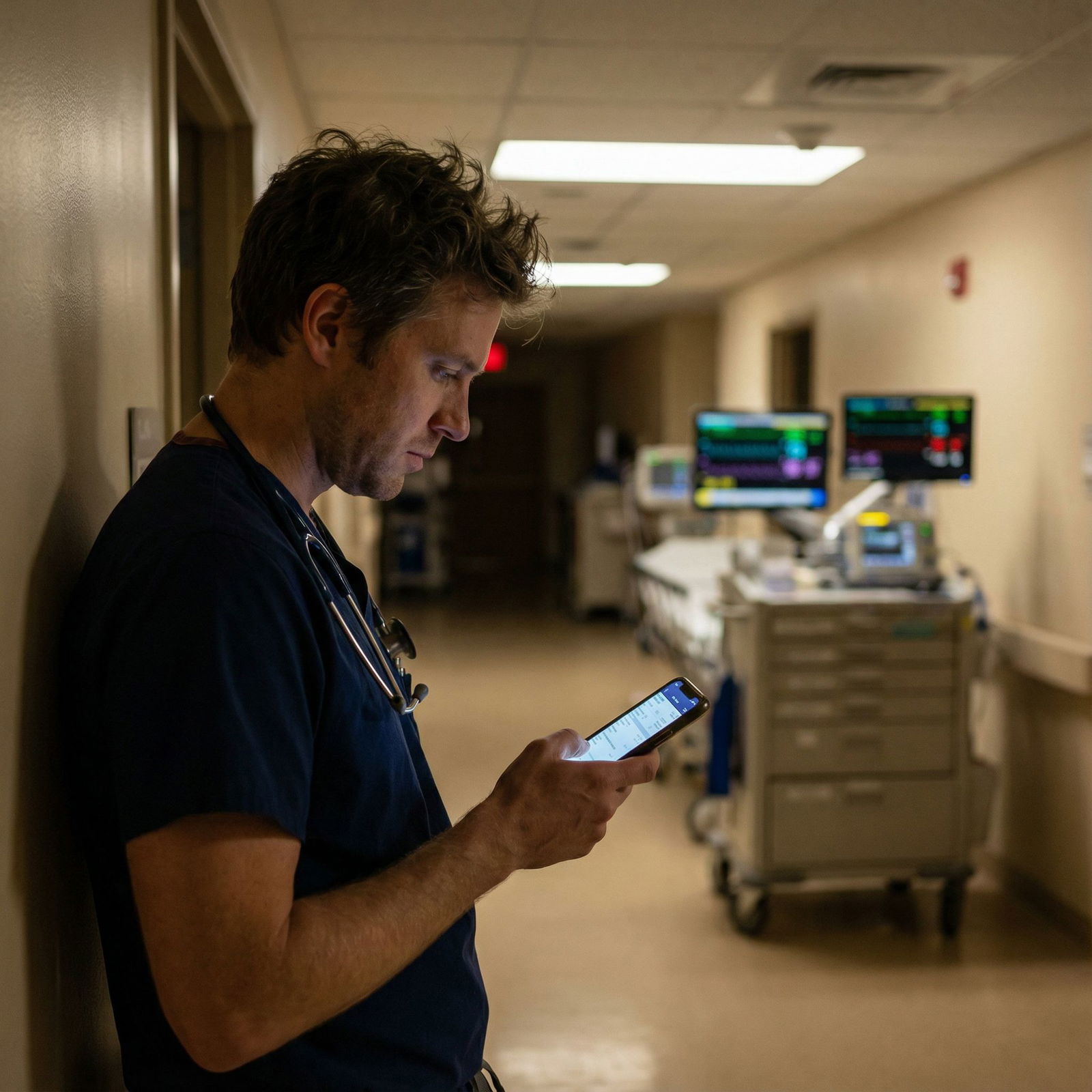
8. Not Having the Data at Your Fingertips
Nothing makes a consultant silently vow to screen your pages later like this sequence:
Consultant: “What’s the creatinine trend?”
You: “Uh, let me scroll… hang on…”
Consultant: “What’s the latest K?”
You: “I’m not sure, I think it was normal.”
Consultant: “What meds are they on?”
You: “…I don’t have that open.”
They will remember that.
Before you ever hit “page,” you should have:
- The chart open with labs and imaging pulled up.
- Key trends jotted down: vitals, relevant labs (not every test from admission).
- Current meds, especially ones relevant to that service (anticoagulants for cards/neurology, nephrotoxic drugs for nephrology, antibiotics for ID, etc.).
Make yourself a one‑page scratch template for consult calls. Something like:
- Name / age / location
- Reason for admission
- Reason for consult
- Vitals now + trend if relevant
- Labs: key ones only (Na, K, Cr, Hgb, WBC, troponin, lactate, etc. as appropriate)
- Imaging: type + main finding
- Meds: especially ones that change management
You are not aiming for a novel. You’re aiming for immediate answers when they ask.
9. Hiding Your Level or Faking Certainty
Consultants hate being misled. It makes their job harder and their trust in you evaporate.
Two flavors:
- Pretending to understand when you don’t.
- Acting like you’re the attending when you’re a PGY‑1 on night float.
When they say, “Are they on pressors?” and you’re not actually sure what counts as a pressor, do not bluff. Just say, “I’m not certain; I see [med names] running at these rates.” That’s honest and fixable.
Similarly, introduce yourself clearly: “I’m the cross‑cover resident on [service], PGY‑1.” Hiding your level just makes them adjust their language mid‑call when they realize you can’t answer fellowship‑level questions.
You are allowed to say:
- “I’m not sure, but I can pull that up right now.”
- “I don’t know the answer to that yet, but I can check the chart/go examine the patient and call you back with that specific info.”
- “I’m early in training, so if I’m missing something obvious, please tell me.”
What you cannot do is give confident wrong answers because you’re scared to look inexperienced. That’s how consultants decide you’re unsafe.
10. Disappearing After You Call
One more way to make specialties hate your pages: vanish.
The pattern:
You page neurology about a concerning neuro change. They call back. No answer. They call again. No answer. Eventually they come see the patient anyway, but now they’re annoyed and your number is on their “low priority” mental list.
Or you ask for urgent input, they recommend a plan, and then you don’t implement it or even document it. So on morning rounds, your attending reads, “Nephrology recommended X,” but nothing was done. Guess who looks irresponsible? You, not them.
If you’re going to call:
- Keep your phone on you and audible.
- If you might be scrubbed or tied up, warn the operator or nurse where to find you, or ask if they can leave a callback time.
- Document the conversation and plan clearly. Include, “Discussed with [Consult Service], plan is X, Y, Z.”
And when consultants actually help you out at 3 a.m., tell your day team. They remember the teams that throw them under the bus versus the ones that acknowledge their work.

| Category | Value |
|---|---|
| Unprepared | 45 |
| Wrong Service | 25 |
| No Question | 40 |
| Non-urgent STAT | 30 |
| Data Missing | 35 |
Those numbers aren’t exact, but they mirror what most seniors quietly complain about.
11. Burning Bridges with Attitude
One last landmine: your tone.
Consultants tolerate inexperience. They do not tolerate arrogance, entitlement, or hostility.
Fastest ways to get your pages mentally blacklisted:
- Sounding like you’re ordering them: “You need to come see this patient.”
- Getting defensive when they ask basic questions.
- Rolling your eyes or making snide comments on speaker where others can hear (trust me, word travels).
- Calling at 3 a.m. for something that obviously could have waited and then acting annoyed that they questioned it.
You can be firm without being rude. Something like: “I understand it’s late, but I’m genuinely concerned about X, and I don’t have the expertise to manage this safely on my own.”
A little humility goes a long way. Consultants will go out of their way for residents who are consistently prepared, respectful, and honest—even if they’re green. They will avoid residents who treat them like a dumping ground.

FAQs
1. How much data is “enough” before I call a consultant on cross‑cover?
You don’t need a thesis. You need: a one‑liner, current vitals, key labs and imaging relevant to the question, current meds that matter, and a clear reason for the consult. If you can’t summarize those in under a minute, you haven’t prepped enough.
2. Should I ever refuse to call a consult if nursing or family insists?
You should not blindly refuse, but you also shouldn’t be a human fax machine. Evaluate the patient yourself, discuss with your senior, and document your reasoning. If, after that, you still think a consult won’t change management overnight, you can say no and explain the plan and timing clearly.
3. Is it okay to leave potential consults for the day team instead of calling overnight?
Often yes, if the patient is stable and the issue is non‑urgent. The key is to explicitly flag it in your sign‑out: “Consider endocrine consult in the morning for complex diabetes regimen; no acute issues overnight.” Don’t just silently hope someone notices.
4. What if the consultant seems annoyed or dismissive on the phone?
Stay calm, stay factual, and don’t match their attitude. Re‑state your concern clearly: “I understand you’re busy. My concern is X in the context of Y, and I don’t feel comfortable managing this alone.” If they still flatly refuse and you truly think the patient is at risk, escalate to your senior or attending immediately.
5. How do I recover if I already made some of these mistakes and think services dislike my pages?
You fix it by being consistently better from now on. Prepare thoroughly before calling, have clear questions, respect urgency, and be transparent about your level. Over a few weeks, people notice. Consultants have short memories for residents who improve and very long memories for those who keep making the same lazy errors.
Key points to walk away with:
- Never call a consult blind—know the patient, know the data, and know your question.
- Respect urgency, the chain of command, and the consultant’s time; don’t use them as a shortcut for your own thinking.
- Your reputation on call is built one page at a time. Protect it.


















