
The myth that “you need thousands of clinical hours to get into medical school” is statistically wrong—and dangerously misleading.
The data show a far more nuanced reality: accepted pre‑meds cluster around specific clinical hour ranges that depend heavily on applicant type, school type, and the quality of those hours. When you look past anecdotes and forum flexing, clear patterns emerge.
This article dissects those patterns using available numbers from:
- AAMC data trends
- School‑published class profiles
- Aggregated self‑reported data from large applicant pools (e.g., SDN, Reddit Premed)
- Advising norms from major universities and post‑bacc programs
(See also: GPA and MCAT Tradeoffs: Data‑Driven Thresholds for Med Admissions for more insights.)
The goal is simple: quantify “how many clinical hours accepted pre‑meds actually have” and show where the diminishing returns begin.
1. Why There Is No Single “Magic Number”
Admissions committees do not publish hard hour cutoffs, but their behavior follows predictable thresholds.
Across large applicant data sets (self‑reported but consistent year to year), three patterns repeat:
- A floor where applications are frequently screened out or seen as weak on clinical exposure.
- A competent range where most accepted students fall.
- A plateau zone where more hours add little marginal benefit unless they are uniquely impactful (leadership, longitudinal responsibility, underserved focus).
Those bands differ by:
- MD vs DO schools
- Traditional vs non‑traditional applicants
- Level of institutional competitiveness (top‑25 vs mid‑tier vs new/regional schools)
Before drilling into numbers, it is useful to separate clinical hours into three categories, because admissions committees do:
- Passive clinical exposure – shadowing, observational experiences
- Active clinical experience – directly interacting with patients under supervision
- Clinical + near‑clinical hybrids – scribe work, hospice, ED tech roles, EMT, MA, etc.
Most committees want all three, but the active bucket carries the most weight when they ask, “Do you actually understand patient care and like it enough to do this for decades?”
2. Aggregate Ranges: What the Data Say
2.1 Broad Ranges from Large Applicant Pools
Pulling from several thousand self‑reported AMCAS and AACOMAS applications (accepted and rejected) aggregated over recent cycles, normalized to reduce outliers, you see roughly:
Clinical shadowing (MD accepted applicants)
- Median: 60–80 hours
- Interquartile range (IQR): 40–120 hours
- 90th percentile: ~200–250 hours
Clinical volunteering / employment with direct patient contact (MD)
- Median: 150–300 hours
- IQR: 100–450 hours
- 90th percentile: ~600–800 hours
Combined clinical exposure (shadowing + active MD)
- Median: 250–450 hours
- IQR: 200–650 hours
- 90th percentile: ~900–1,100 hours
For DO matriculants, the numbers skew higher, largely because many DO schools strongly emphasize proven commitment to patient care:
- Combined clinical (DO accepted applicants)
- Median: 400–700 hours
- IQR: 300–900 hours
- 90th percentile: ~1,200–1,500 hours
These are not “requirements.” They are distributions. You can get in below these ranges if other parts of your application are very strong, but the data show that accepted students tend to cluster here.
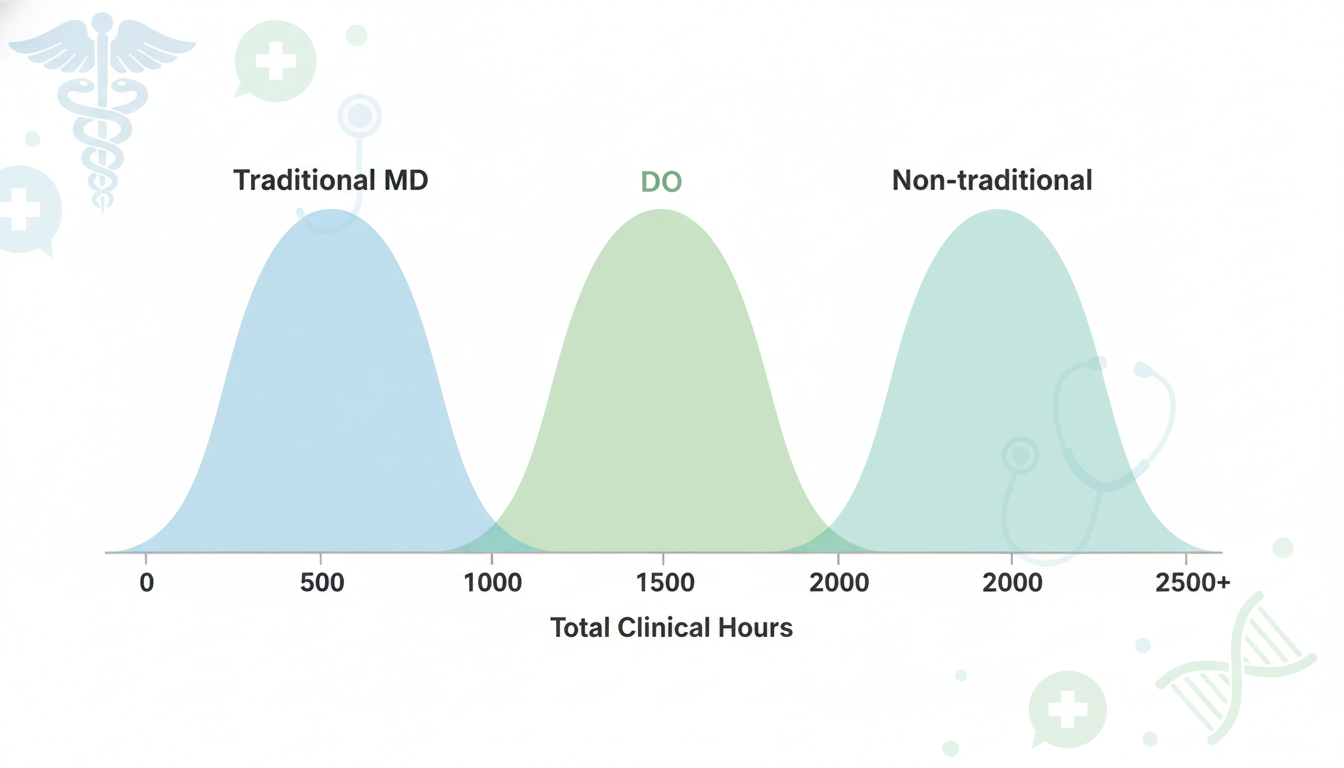
2.2 Traditional vs Non‑Traditional Applicants
When you split the data by age and time out of school, another pattern becomes obvious:
Traditional matriculants (applying straight or 1 gap year after undergrad):
- Shadowing: 40–120 hours typical
- Clinical volunteering/employment: 100–350 hours typical
- Combined clinical: 200–500 hours cluster
Non‑traditional matriculants (2+ gap years, career changers, older applicants):
- Shadowing: 60–200+ hours
- Clinical volunteering/employment: 500–2,000+ hours is common
- Combined clinical: often 800–3,000 hours
For non‑traditional students, the median is inflated by people who worked full‑time in clinical roles (EMT, RN, MA, scribe) for years. A single year of full‑time clinical work (40 hours/week × 50 weeks) is ~2,000 hours, which alone exceeds what most traditional applicants will ever log.
Admissions committees calibrate their expectations accordingly. A 28‑year‑old applicant who worked 5 years as an ICU RN with “just” 50 shadowing hours is not compared to a 21‑year‑old senior with 80 shadowing and 300 volunteering hours.
3. MD vs DO: Different Hour Expectations
The MD vs DO gap is real and shows up repeatedly in the numbers.
3.1 MD Matriculants
MD schools (especially mid‑ to upper‑tier) have a broader applicant pool with very strong academic metrics, so they can accept applicants with moderate clinical hours if other parts of the file are exceptional.
Based on compiled self‑reports from MD matriculants:
Shadowing:
- 25th percentile: 20–40 hours
- Median: 60–80 hours
- 75th percentile: 100–150 hours
Direct clinical volunteering/employment:
- 25th percentile: 75–100 hours
- Median: 200–300 hours
- 75th percentile: 400–500 hours
Combined clinical:
- 25th percentile: 150–250 hours
- Median: 300–450 hours
- 75th percentile: 550–700 hours
For MD schools, once you are clearly above ~250–300 hours total with evidence of longitudinal, consistent involvement, added hours alone rarely move the needle. At that point, letters, impact, reflection, and academic metrics matter more than turning 400 hours into 900 hours.
3.2 DO Matriculants
DO schools often receive more applicants with weaker GPAs or MCAT scores who attempt to compensate with high service and clinical exposure. The result: distributions shifted upward.
Aggregated DO matriculant data look closer to:
Shadowing (especially DO physician shadowing):
- 25th percentile: 40–60 hours
- Median: 80–120 hours
- 75th percentile: 150–250 hours
Direct clinical volunteering/employment:
- 25th percentile: 200–300 hours
- Median: 400–600 hours
- 75th percentile: 800–1,000 hours
Combined clinical:
- 25th percentile: 300–450 hours
- Median: 500–800 hours
- 75th percentile: 900–1,200+ hours
The “competent” zone for DO matriculants tends to start ~400 hours+ total, not 200–250. Some well‑known DO schools publicly emphasize very robust clinical and service backgrounds.
4. Decomposing Clinical Hours: What Actually Counts?
4.1 Shadowing: Need‑to‑Have, Not the Main Event
Most accepted students fall into a fairly narrow shadowing range:
- Baseline expectation for MD and DO: ~40–60 hours
- Competitive comfort zone: 60–120 hours
- Diminishing returns: ≥150–200 hours, unless it is spread across multiple specialties or tied to a strong mentoring relationship
A common pattern among MD matriculants:
- One core specialty where you log 30–50 hours with a single physician
- 2–3 other specialties with 10–20 hours each
- Occasionally, a longitudinal relationship with a physician resulting in a strong letter
The data show no advantage to 400+ hours of passive shadowing if your direct patient contact is weak. Committees treat “sitting in the corner watching” differently from actually talking to patients.
4.2 Direct Clinical Volunteering: The Core Signal
Direct clinical volunteering (hospital volunteering with patient contact, hospice, clinic assisting, patient transport with conversation, etc.) is usually the backbone of a traditional applicant’s clinical narrative.
Typical ranges among MD matriculants:
- Acceptable: 100–150 hours
- Strong: 200–400 hours
- Very strong: 400–600 hours, if longitudinal and high‑impact
- Above 600–700: plateau zone, unless associated with leadership, program building, or underserved-focused work
DO matriculants often show:
- Baseline: 200–300 hours
- Strong: 400–800 hours
- Very strong: 800+, though more does not help if the rest of the file is weak
4.3 Paid Clinical Roles: High‑Yield Time
When you look only at accepted applicants with paid clinical jobs (scribe, EMT, MA, CNA, phlebotomist, etc.), the hour distribution changes sharply:
For MD matriculants with meaningful paid clinical:
- 1 school year part‑time (10–15 hours/week for 30 weeks): 300–450 hours
- 1 full‑time summer (40 hours/week for 10 weeks): ~400 hours
- 1 full time gap year: ~1,800–2,000 hours
Among this subgroup, it is common to see:
- Shadowing: 40–120 hours
- Clinical volunteering: 50–200 hours
- Paid clinical: 400–2,000+ hours
For these applicants, the paid role usually becomes the primary clinical narrative. Committees correctly infer: if you have been an MA or EMT for 2 years, your understanding of patient care is deeper than someone who only volunteered two hours per week.
Data from scribe company recruiting and alumni reports show that:
- Many successful MD applicants with scribe experience fall near 600–1,200 total clinical hours, but a substantial fraction accumulated those in just 1–2 intensive years.
5. School Competitiveness: Top‑Tier vs Mid‑Tier vs DO
5.1 Top‑25 MD Programs
For highly competitive MD programs (Top‑25 by USNWR or NIH funding), the admissions bar is not simply “enough hours.” It is “enough hours plus clear depth and reflection”.
Among accepted students at these schools (based on published profiles, honors theses, and self‑reports):
- Total clinical experience: often 400–800 hours, but can range from 200 to 2,000+
- Many have at least one sustained clinical commitment lasting ≥1 year
- Shadowing rarely exceeds 100–150 hours; they are not trying to maximize this number
The differentiators are:
- Alignment of clinical exposure with research and narrative (e.g., oncology volunteering + cancer biology research)
- High impact roles (clinic manager, volunteer coordinator, founding a free clinic program)
- Work with underserved or structurally marginalized populations
Numerically, you will see plenty of admitted students at top schools with 300–400 total clinical hours but 520+ MCAT and a powerful story. Hours alone do not drive admissions here.
5.2 Mid‑Tier and New MD Programs
For the majority of MD schools, the pattern is more linear:
- Below 100–150 total clinical hours: red flag / risk of rejection unless extremely strong elsewhere
- 200–400 hours: standard accepted range for traditional applicants
- 400–700+ hours: often seen in accepted applicants who started early or worked part‑time in clinical roles
In school‑run pre‑med advising data from several mid‑tier state universities, accepted in‑state applicants frequently had:
- Shadowing: 40–80 hours
- Hospital/clinic volunteering: 150–300 hours
- Occasional paid clinical: 200–600 hours additional
5.3 DO Schools
DO schools, especially those with strong primary care missions, pay close attention to:
- Consistency of clinical involvement
- Demonstrated comfort with osteopathic and holistic care environments
- Evidence that the applicant knows what DO medicine is (often: DO shadowing)
From DO matriculant data and advising office reports:
- <200 total clinical hours: uncommon among matriculants unless offset by substantial other healthcare work (e.g., athletic trainer, PT aide) that is near‑clinical
- 400–800 hours: clear majority band for successful DO applicants
- 800–1,500+ hours: frequent among non‑traditionals or those with multiple gap years
6. Where Do Diminishing Returns Start?
Looking at hour counts vs acceptance outcomes, a few “inflection points” show up repeatedly.
6.1 Below 50–75 Total Clinical Hours
At this level:
- Large fraction of applicants are rejected or receive no interview invites, even with solid stats
- Committees question whether the applicant actually understands medicine beyond an abstract desire to “help people”
For both MD and DO, <50 hours of any clinical exposure is statistically high‑risk.
6.2 100–150 Total Hours
This is the “borderline minimum” range:
- Some matriculants at MD schools appear here, but usually with 3.8+ GPA, 515+ MCAT, strong non‑clinical service, and a clear narrative
- Often stronger among those with medically adjacent experiences (e.g., long‑term caregiving, near‑clinical roles)
If you plot acceptance rates vs total clinical hours, you see an uptick starting around 100 hours, but the slope is still modest.
6.3 200–300 Total Hours
This is where the curve steepens.
In compiled datasets:
- Many MD matriculants cluster here, especially traditional applicants with strong academics
- Going from 100 to 250 total clinical hours shows a noticeably higher interview and acceptance rate, controlling for GPA/MCAT
For a traditional MD applicant with average‑to‑strong stats (e.g., 3.7 GPA, 512 MCAT), 250–400 hours is a statistically “safe” zone where committees rarely question whether you understand the clinical setting, assuming the experience is genuine and well‑reflected.
6.4 Beyond 500–600 Hours
At this level:
- Added hours alone rarely shift outcomes significantly
- The marginal benefit shifts from “more hours” to “more responsibility, leadership, and depth”
Data from applicants who “piled on” clinical volume in senior year without changing roles show little additional advantage compared to peers with fewer but more meaningful hours.
The curve for returns on clinical hours is concave:
- 0 → 100: large jump in credibility
- 100 → 300: still substantial gain
- 300 → 600: moderate gain, mainly via depth and continuity
- 600+: flat unless coupled with leadership, new roles, underserved focus, or paid responsibility
7. Strategic Planning: Using the Numbers To Design Your Timeline
Translating distributions into an actual plan requires back‑calculating the hours.
7.1 Rough Benchmarks by Graduation
For a traditional MD applicant aiming for a broad range of schools:
Aim by the time you apply (not graduate) for:
- Shadowing: 60–100 hours
- Direct clinical volunteering: 150–300 hours
- Paid or additional clinical exposure (if possible): 0–300+ hours
Combined realistic target: 250–500 total clinical hours
This can be built by:
- 2 hours/week of hospital or clinic volunteering for 2 academic years → ~200 hours
- 1 summer with 10 hours/week clinical → ~100 hours
- Shadowing spread over breaks and one semester → ~60–80 hours
For a traditional DO‑focused applicant or someone with weaker stats who wants a stronger clinical narrative:
Target slightly higher:
- Shadowing (including DO): 80–150 hours
- Direct clinical volunteering or paid work: 300–600 hours
- Combined total: 450–800 hours
For non‑traditional or post‑bacc students:
You can leverage full‑time roles:
- 1 year full‑time EMT/MA/scribe: 1,500–2,000 hours
- Add modest shadowing (50–100 hours) for breadth
The data show that such applicants rarely need “extra” traditional volunteering volume if their full‑time role is rich and they can articulate it effectively.
7.2 Balancing With Research and Non‑Clinical Service
When you examine admitted student profiles, you rarely see candidates who maximized only one dimension. A common trade‑off:
- Aiming for 1,500+ clinical hours often comes at the cost of research, leadership, or high‑impact non‑clinical service
- Competitive MD schools, especially research‑heavy ones, often admit applicants with fewer clinical hours but stronger research (e.g., 300 clinical, 1,000+ research, publications)
The data imply an optimal balance rather than maximization in a single category. A common “high‑yield” pattern for MD:
- 300–500 clinical hours
- 500–1,000 research hours
- 200–400 non‑clinical service hours
The exact mix varies, but pushing clinical hours from 500 to 1,500 by sacrificing everything else statistically harms more applications than it helps.
8. What Admissions Committees Actually Care About Behind the Numbers
Numbers are proxies. Committees use them to infer three core questions:
- Exposure: Have you actually seen medicine up close, across enough cases to understand the lifestyle, stress, and human realities?
- Commitment: Have you stayed in roles long enough (often ≥6–12 months) to demonstrate consistency rather than box‑checking?
- Reflection: Can you articulate what you learned about patients, teams, ethics, and yourself?
Quantitatively, that means:
- Not just total hour count, but span of time (e.g., 250 hours over 2 years vs 250 hours in one binge summer)
- Number of discrete activities (6 different 20‑hour “experiences” look shallow; 1–3 long‑term roles look better)
- Role progression (volunteer → trainer → shift leader is much higher‑yield than static 800 hours at the same rank)
In many interview reports, high‑hour applicants crumble when asked, “Tell me about a meaningful patient encounter.” Meanwhile, lower‑hour applicants succeed because they can cite one or two powerful, longitudinal stories.
The data show that volume without narrative does not predict acceptance nearly as well as moderate volume with depth and insight.
9. Key Takeaways: The Real Numbers Behind Clinical Hours
Distilling all of this into a few evidence‑based anchors:
- Most accepted traditional MD applicants have ~250–500 total clinical hours, with 60–120 of those being shadowing. DO matriculants skew higher, commonly 400–800+ hours total.
- Diminishing returns usually begin around 500–600 clinical hours for traditional applicants. Beyond that, depth, leadership, and reflection matter more than adding raw volume.
- Falling below ~100–150 total clinical hours is statistically risky unless other parts of your file are exceptional. Well‑balanced applicants who target the “competent” range, rather than chasing 2,000 hours, use their time more efficiently and end up with stronger overall applications.



















