
Failing to match into urology residency is deeply disappointing—and, for many, frightening. Years of work, high stakes, and a specialty you care about can make the words “didn’t match” or “unmatched applicant” feel like a verdict on your entire career. It is not.
This guide is designed to help you move from shock to strategy: understanding what happened, finding concrete recovery options, and rebuilding the strongest possible application for the next urology match (or for a thoughtful pivot if your goals change).
Understanding a Failed Urology Match
Before planning a comeback, you need a realistic, specific understanding of why your urology residency application was not successful. The reasons are usually multifactorial and often only partially visible to you—so structured reflection and external feedback are essential.
The competitive landscape of urology
Urology is one of the most competitive specialties in the residency match. Typical features of the applicant pool include:
- Strong USMLE/COMLEX scores (although the Step 1 score change has shifted emphasis to Step 2 CK and holistic review)
- Extensive research, often with urology-specific projects
- Multiple away rotations (“sub-Is”) in urology
- Strong letters of recommendation from known urologists
- Evidence of long-standing interest in the specialty
Even well-qualified candidates go unmatched. Each program has limited spots, and applicant fit, institutional priorities, and the randomness of a small sample size of interviews play a major role.
Typical factors contributing to a failed match
Common contributors to a failed match in urology residency include:
Insufficient number or quality of interviews
- Only a few interview invites, or cancellations due to scheduling conflicts
- No “safety” programs or imbalanced list (e.g., mostly highly competitive academic centers)
Application profile issues
- Limited or no urology research
- Weak or generic letters of recommendation
- Lower Step 2 CK or COMLEX Level 2 scores relative to the applicant pool
- Failed or repeated licensing exams, or academic struggles in pre-clinical/clinical years
- Limited urology exposure or late switch into the specialty
Interview performance
- Difficulty articulating “Why urology?” or your specific career vision
- Rigid, overly scripted answers or weak interpersonal communication
- Concerns about professionalism, maturity, or self-awareness
Strategic and structural issues
- Applied to too few programs
- Overly narrow geographic focus without strong regional ties
- Late completion of ERAS, letters, or Step 2 CK testing
- Weak personal statement or poorly constructed CV
First steps in the days after the match
Immediately after learning that you didn’t match:
Give yourself 24–72 hours
- It’s normal to feel grief, anger, embarrassment, or numbness.
- Avoid sending impulsive emails to programs or posting detailed public reactions on social media.
Confirm your status and options
- For NRMP-participating programs, verify whether you are partially matched (e.g., PGY-1 only) or fully unmatched.
- If SOAP is relevant this cycle, identify whether there are any preliminary or categorical spots that align with your longer-term plan.
Protect your mental health
- Talk to trusted friends/family away from the circular conversations of classmates.
- Reach out early for professional support if you have a history of anxiety, depression, or burnout.
Once the initial emotional wave passes, shift to structured analysis.
Forensic Review: What Went Wrong (and How to Find Out)
The most powerful recovery plans come from specific diagnoses of what limited your application. That means going beyond vague statements like “I guess I wasn’t competitive enough” and drilling down into concrete, actionable feedback.
Conducting an honest self-assessment
Start with a written reflection organized around five domains:
Academic record
- Step 1 (if numeric), Step 2 CK, and COMLEX scores
- Course and clerkship grades, particularly surgery and urology rotations
- Any failures, repeats, leaves of absence, or professionalism concerns
Urology-specific exposure
- Number and quality of urology rotations (home + away)
- Involvement with urology interest group, shadowing, mentorship
- Evidence of longitudinal interest vs. a late switch
Research and scholarly work
- Publications, abstracts, posters, and presentations—especially in urology
- Strength of research mentors and their ability to advocate for you
- Ongoing projects you could reasonably bring to completion in the next 6–12 months
Letters of recommendation
- Who wrote your letters, and what is their reputation in urology?
- How well did they know you? Did they see you on a urology rotation?
- Did you spread your letters across different institutions or lean heavily on one site?
Application strategy and interviewing
- Number of programs applied to, and their competitiveness level
- Number of interviews offered and attended
- Your preparation for interviews (mock interviews, feedback from mentors)
- Any red-flag moments you recall (awkward interactions, misunderstood questions, difficult MMI scenarios)
Be brutally honest. This document is for you and your closest advisors.
Seeking external feedback (the right way)
Your own perspective is incomplete. You need outside eyes:
Home institution urology leadership
- Request a specific meeting with:
- Program Director (PD)
- Associate PD or Chair
- A faculty mentor who knows you clinically
- Frame the conversation:
- “I didn’t match in urology this cycle and I’d really value your candid assessment of my application. If I pursue a re-application, what would I need to strengthen to be viable?”
- Request a specific meeting with:
Away rotation mentors
- Email mentors at away institutions where you rotated:
- Briefly acknowledge you didn’t match.
- Ask if they’d be willing to discuss your candidacy and potential paths forward.
- They may offer insight into:
- How you were perceived on the rotation.
- Whether your letters were likely to be strong, average, or lukewarm.
- Their view of your competitiveness in the next cycle if you enhance key areas.
- Email mentors at away institutions where you rotated:
Residency program directors (beyond your own)
- Some PDs are willing to review an unmatched applicant’s CV and give quick impressions.
- Lean on your mentors to make warm introductions when possible rather than cold emailing dozens of PDs.
Objective data points
- Compare your metrics to published urology residency match data (AUA/NRMP reports, though details vary by year).
- This helps benchmark whether your scores or research output were significantly below the median.
You may hear painful feedback. Listen carefully, take notes, and ask clarifying questions. This is not about defending yourself; it’s about collecting the data you need to design your recovery.
Immediate Post-Match Options: Bridge Years and Alternatives
Once you understand the “why,” you can explore “what now.” As an unmatched applicant after a failed match in urology, you have several immediate and longer-term options. The right choice depends on your academic profile, finances, personal circumstances, and how committed you are to urology versus open to other specialties.

SOAP and late-cycle opportunities
If you discover your mismatch during Match Week:
Participate in SOAP (if eligible)
- Realistically, categorical urology spots are extremely rare in SOAP.
- Focus instead on:
- Preliminary general surgery positions
- Transitional year (TY) programs
- Internal medicine prelim positions
- Choose something that:
- Offers strong surgical exposure if you plan to re-apply in urology
- Resides in an institution with an active urology department if possible
Post-SOAP open positions
- Occasionally, programs in other specialties have unfilled spots outside SOAP.
- If you are considering pivoting away from urology, these can be options—but think carefully before committing to a specialty you don’t want long term.
Common structured “bridge year” paths
If you are fully unmatched or decide not to start a non-urology residency this year, there are several classic routes to strengthen a future urology match application:
1. Dedicated research year in urology
Often the strongest option for those with adequate exam scores but weaker scholarly output or letters.
Pros:
- Directly augments your urology CV with:
- Manuscripts, abstracts, conference presentations
- Exposure to academic urology and subspecialties
- Close relationships with urology faculty who can:
- Write powerful letters
- Advocate for you with colleagues and PDs
- Daily immersion in the field reinforces your “Why urology” narrative
Cons:
- Typically lower pay than a residency salary (some positions are unpaid or grant-funded).
- Visa, benefits, and location constraints for international applicants.
- Requires clear expectations: authorship, responsibilities, access to OR/clinic.
Key advice:
- Target institutions with a track record of successfully matching their research fellows into urology.
- Before committing, ask:
- “How many previous research fellows have matched into urology, and where?”
- “How involved are fellows in writing and first authorship?”
- “Will I have opportunities to attend clinics, ORs, and conferences?”
2. Preliminary surgery or transitional year
This is a common path for unmatched applicants who want clinical experience while they re-apply.
Pros:
- Solid surgical and inpatient experience—appealing for urology PDs.
- Demonstrates professionalism, work ethic, and the ability to function as an intern.
- Offers potential for strong letters from surgical faculty.
Cons:
- Demanding workload leaves less time for research and application-building.
- Some programs may be less supportive of residents simultaneously re-applying to another specialty.
- If you match into a PGY-1 that doesn’t convert to urology later, you’ll face a second match process.
Key advice:
- Choose a program with:
- A known urology department
- PDs who are explicitly supportive of your plan to re-apply to urology
- A culture that allows time for research/scholarly work if possible
3. Non-urology research or advanced degrees (e.g., MPH, MS)
Useful if your main deficits are academic (research methods, publications) or you’re still somewhat undecided about urology vs. a broader career in academic medicine.
Pros:
- Builds a strong scholarly foundation that’s valuable in any specialty.
- Adds credentials that can differentiate you in the urology match.
- May provide networking and exposure across disciplines.
Cons:
- Less urology-specific; may not directly improve your fit narrative.
- Extra tuition and opportunity cost of delayed residency start.
Pivoting to another specialty: when is it reasonable?
Though many unmatched applicants successfully re-enter the urology match and match the second time, not everyone will. Consider a pivot when:
- You have significant, unmodifiable barriers to urology (e.g., major academic issues, very low exam scores, multiple attempts).
- Multiple experienced PDs and mentors honestly tell you that your chances are extremely low despite maximal remediation.
- You discover that your passion may be broader than operative urology (e.g., general surgery, internal medicine with nephrology focus, radiology with GU emphasis, oncology, etc.).
A pivot is not a failure—it’s a strategic decision to build a fulfilling career aligned with your realistic opportunities and deeper interests.
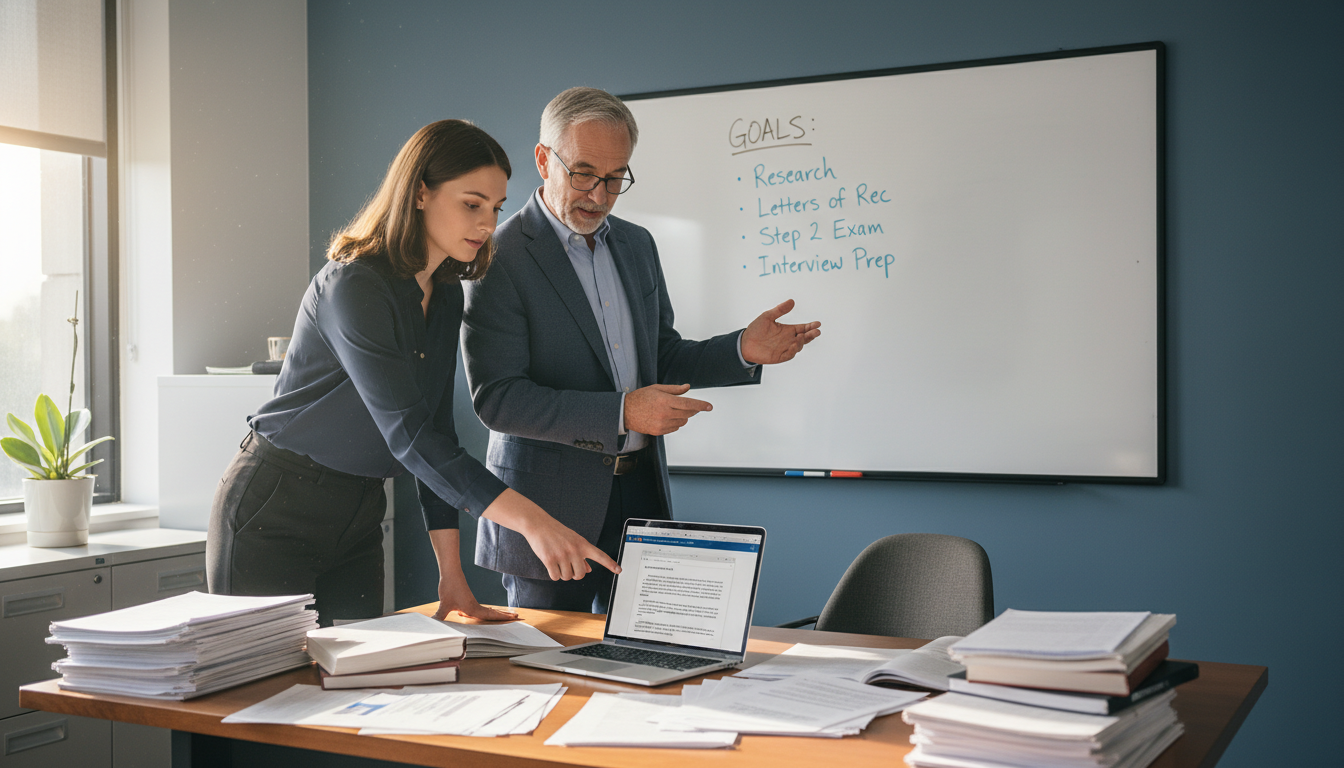
Strategic Rebuilding: Strengthening Your Next Urology Application
If you decide to re-enter the urology match after a failed attempt, treat the next cycle as a fresh campaign—not a repeat. Programs need to see a clearly stronger, more focused applicant, not the same file with an extra year on it.
Academic optimization: exams and transcript
USMLE/COMLEX
- If Step 2 CK/Level 2 scores are borderline:
- Consider dedicated prep and a retake only if allowed and realistically likely to improve.
- For DO students, ensure Step 2 CK is completed with strong performance if most urology programs you’re targeting prefer or require it.
- If you failed an exam, be prepared with:
- A concise explanation
- Evidence of remediation (courses, improved later scores, tutoring others, etc.)
- If Step 2 CK/Level 2 scores are borderline:
Clinical performance
- In a prelim/TY year:
- Aim for strong evaluations and visible professionalism.
- Volunteer for urology consults when appropriate.
- If you are still a student (e.g., early grad), maximize performance on surgical and urology rotations.
- In a prelim/TY year:
Urology exposure and letters of recommendation
Rotations and observerships
- Seek additional urology experiences:
- Short electives at institutions where you’re doing research
- Local or regional urology groups
- If you previously lacked away rotations, prioritize at least one targeted away at a program that knows your mentors.
- Seek additional urology experiences:
Letters of recommendation
- Aim for:
- At least two letters from practicing urologists who have worked with you clinically or in research.
- One letter from a non-urology physician who can attest to your work ethic, professionalism, and team skills (e.g., general surgery, medicine).
- Ask letter-writers explicitly:
- “Do you feel you can write me a strong letter for urology?”
- Provide them with:
- Updated CV
- Personal statement draft
- Summary of what has changed since your last application
- Aim for:
Mentorship network
- Build a small “advisory board” of 2–4 mentors:
- At least one urology faculty member
- A program director or associate PD (any specialty) who understands the match process
- Possibly a recent re-applicant who successfully matched in urology
- Build a small “advisory board” of 2–4 mentors:
Research and scholarly productivity
Well-structured research can transform an unmatched applicant into a strong re-applicant:
Short-term vs long-term projects
- Short-term:
- Case reports
- Retrospective chart reviews
- Review articles
- Long-term:
- Prospective studies
- Clinical trials
- Basic science projects
- Short-term:
Aim for visible outputs
- Abstract submissions to:
- AUA, sectional/regional urology meetings
- Specialty-specific societies (e.g., SUO, pediatric urology groups)
- Poster or oral presentations
- Manuscripts in process with realistic timelines for submission
- Abstract submissions to:
Tell a coherent story
- Your research portfolio should reinforce your “Why urology” narrative:
- E.g., health disparities in prostate cancer, outcomes after stone surgery, reconstructive urology.
- Your research portfolio should reinforce your “Why urology” narrative:
Programs are not counting just the number of projects; they’re evaluating your depth of engagement and trajectory.
Rewriting your story: personal statement and application narrative
Your personal statement and ERAS experiences must clearly acknowledge and contextualize your failed match—without sounding defensive or self-pitying.
Key principles:
Own the outcome without apology tours
- Briefly mention that you didn’t match.
- Frame the year as a period of growth, focus, and confirmation of your commitment.
Highlight specific growth
- Examples of enhanced maturity, resilience, scientific thinking, or clinical skills.
- Concrete contributions in your research year or prelim/TY role.
Clarify your dedication to urology
- Show deep understanding of:
- The lifestyle and demands of the field
- Subspecialty interests you’ve explored
- The aspects of urology that most energize you (operative, longitudinal care, technology, etc.)
- Show deep understanding of:
Be forward-looking
- Programs want a picture of you as a future colleague and trainee, not a rehash of last cycle’s disappointment.
Interview preparation for the second round
Your previous status as an unmatched applicant will come up. Prepare thoughtful, concise answers.
Common questions and how to approach them:
“What did you do in your gap year?”
- Outline:
- Your main position (research fellow, prelim surgery, etc.)
- 2–3 specific accomplishments
- Skills gained that will make you a better urology resident
- Outline:
“Why do you think you didn’t match last cycle?”
- Acknowledge 1–2 key factors:
- “I had limited urology research and my letters reflected only a single institution…”
- Then pivot to corrective actions:
- “Since then, I’ve completed X, Y, and Z, which have given me a much stronger application and a deeper understanding of the field.”
- Acknowledge 1–2 key factors:
“What did you learn from that experience?”
- Emphasize resilience, insight, and adaptability.
- Avoid blaming programs or the system; focus on your growth.
Behavioral questions
- Have multiple examples ready around:
- Handling failure or criticism
- Managing high workload situations
- Working in teams under stress
- Have multiple examples ready around:
Engage in multiple mock interviews with mentors and, if available, your school’s career office. Record yourself and watch for filler words, body language, and clarity of your responses.
Emotional Resilience, Identity, and Long-Term Perspective
The urology match is intense, and a failed match can feel like a rejection of your identity as a future surgeon. You’re not just rebuilding an application; you’re rebuilding confidence and purpose.
Normalizing the experience
Many excellent urologists have:
- Gone unmatched on their first attempt
- Completed preliminary years or research fellowships
- Considered or tried other specialties before ultimately landing in urology
You usually don’t hear these stories publicly, but in private conversations, they are common. Your career will be defined not by this single outcome, but by how you respond.
Protecting your mental health
Name what you’re feeling
- Grief and shame are common, especially if peers have matched.
- Impostor syndrome can spike even for high-performing individuals.
Build a support structure
- Confide in:
- A small circle of peers
- A therapist or counselor (many schools and hospitals offer free or low-cost services)
- Mentors who validate your feelings but push you toward constructive steps
- Confide in:
Maintain a life outside the match
- Preserve time for exercise, sleep, and non-medical interests.
- This is not wasted time; it protects the very resilience you’ll need to succeed as a resident.
Redefining success
Even if your ultimate path leads away from urology, your training and efforts have not been wasted. You are building:
- Clinical reasoning skills applicable across specialties
- Research and critical appraisal skills
- Professional habits and networks that will support you for decades
Give yourself permission to hold both truths: you can be deeply disappointed and still build a meaningful, fulfilling medical career.
FAQs: Failed Match Recovery in Urology
1. Is it realistic to match into urology after failing to match once?
Yes. Many applicants successfully match into urology on their second attempt. Your odds improve significantly if you:
- Address specific weaknesses (research, letters, exam scores, interview skills)
- Engage in a meaningful bridge year (urology research, prelim surgery, or TY with urology contact)
- Have honest guidance from urology mentors and PDs
The key is demonstrating clear progression, not just additional time.
2. Should I mention that I didn’t match in my personal statement?
Briefly, yes. Ignoring it can feel evasive. A good approach:
- Acknowledge the failed match in 1–2 sentences.
- Focus the majority of the statement on:
- What you did in the interim
- How the experience confirmed your commitment to urology
- Concrete growth and readiness for residency
Keep the tone accountable and forward-looking, not apologetic.
3. Which is better for a re-applicant: a research year or a preliminary surgery year?
It depends on your specific deficits:
Research year:
- Best for applicants lacking urology-specific research and letters.
- Ideal if you want to build a strong academic profile and network in urology.
Prelim surgery/TY:
- Best if you need to demonstrate clinical excellence and professionalism.
- Helpful if you already have some research but limited clinical evaluations.
Discuss your situation with multiple mentors and, if possible, a urology PD who can help you choose the path with the highest yield for the next urology match.
4. When should I consider pivoting away from urology?
Consider a serious pivot when:
- Multiple seasoned urology PDs or chairs, after reviewing your full file, advise that your chances are very low despite remediation.
- You recognize that your interests might be well served in related fields (e.g., general surgery, IR, nephrology, oncology).
- The cumulative personal, financial, and emotional toll of repeated attempts outweighs the likely benefit.
A thoughtful pivot can still lead to a rich, rewarding career. Changing direction is not giving up; it’s choosing a path where you can thrive.
A failed match in urology is a painful event—but not a dead end. With honest feedback, strategic planning, and sustained effort, many unmatched applicants become successful urology residents and respected surgeons. Whether your next step is a research year, a prelim position, or a new specialty direction, you retain the most important assets: your capacity to learn, to grow, and to care for patients.






















