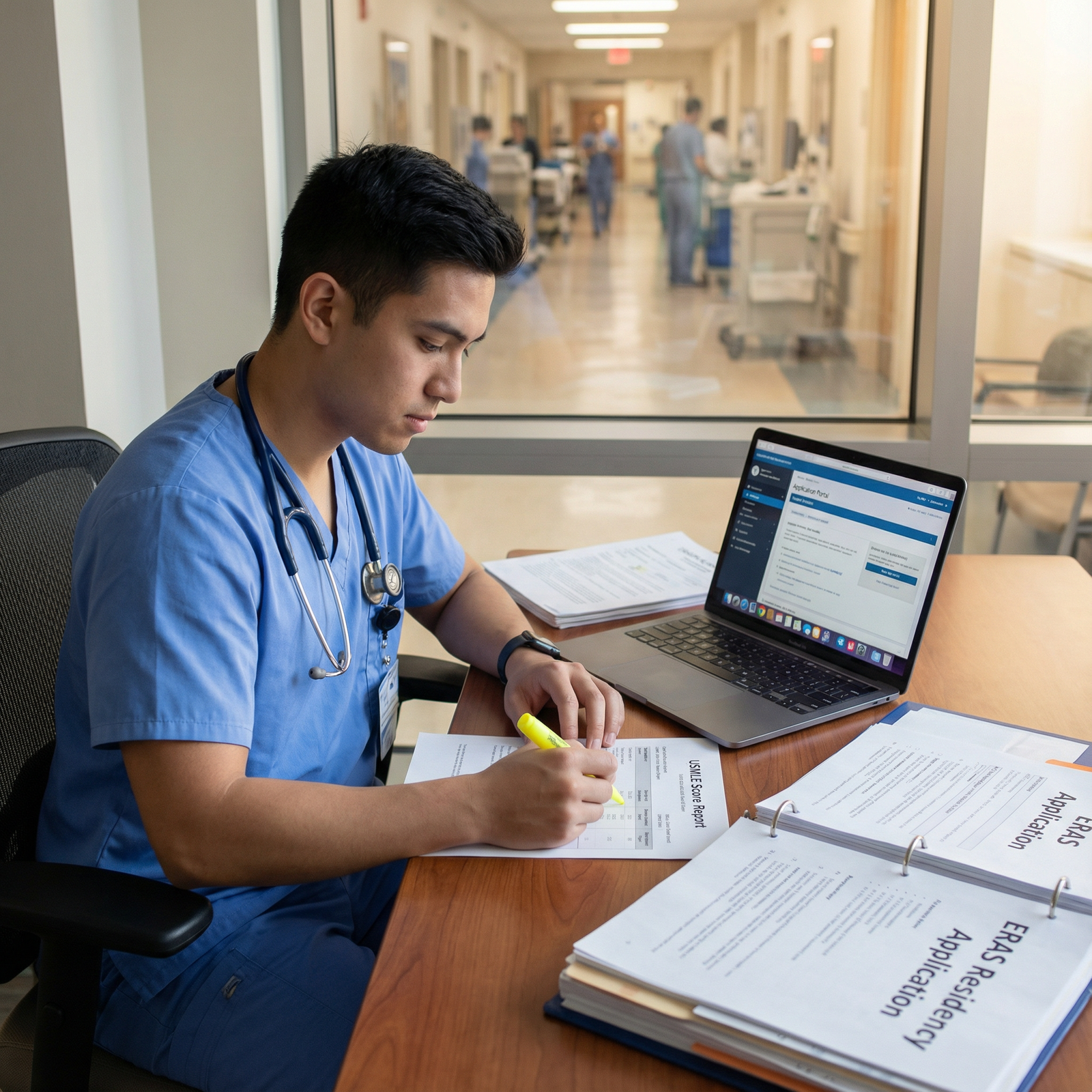
Reapplying for Residency: Essential Strategies to Strengthen Your Application
Reapplying for residency can feel overwhelming, especially after investing years into medical training and USMLE preparation. An unsuccessful match is emotionally and professionally difficult—but it is not the end of your path to becoming a physician. Many successful residents and attendings matched on their second or even third try.
Reapplication is an opportunity to step back, analyze what went wrong, strategically rebuild your profile, and return to the Match with a stronger, more focused Residency Application. With deliberate planning, you can turn this setback into a powerful phase of Career Development.
This guide walks through practical, step-by-step strategies to strengthen your application, refine your story, and maximize your chances of matching on your next attempt.
Understanding Why You Didn’t Match: Honest Diagnosis Before Reapplication
Before changing anything, you need a clear, honest understanding of why your previous application was not successful. Without this “diagnosis,” your efforts to improve may be misdirected.
Common Reasons for an Unsuccessful Match
Some of the most frequent contributors include:
Weak or generic personal statement
- Did your essay sound like anyone else’s?
- Did it fail to explain why you chose your specialty and what makes you different?
- Did it avoid addressing obvious red flags (e.g., exam failures, gaps)?
Insufficient or outdated clinical experience
- Limited hands-on experience in the U.S. (for IMGs)
- No recent clinical work, especially if you’ve been out of school for a few years
- Lack of experiences aligned with your chosen specialty (e.g., applying to Internal Medicine without any inpatient exposure)
Uninspired or lukewarm letters of recommendation (LoRs)
- Letters from faculty who barely knew you
- Generic, template-like letters with no specific anecdotes
- Absence of specialty-specific letters (e.g., no Psychiatry letter for a Psychiatry application)
Low or borderline USMLE/COMLEX scores
- Scores below the typical cutoffs for your specialty or target programs
- Multiple attempts on Steps or Level exams without explanation
- Unbalanced profile (e.g., strong Step 1 but weak Step 2 CK)
Limited research and scholarly activity
- Especially important in competitive specialties (Dermatology, Radiology, Orthopedics, etc.)
- Lack of any academic involvement: no posters, abstracts, QI projects, or publications
Application strategy issues
- Applying too narrowly (too few programs or only highly competitive institutions)
- Poor geographic strategy (e.g., applying only to coastal academic centers with high competition)
- Missed deadlines or incomplete ERAS materials
How to Accurately Identify Your Weaknesses
Use multiple sources of feedback:
- Program director (PD) or faculty feedback: If any PDs or interviewers offered comments after the Match, take them seriously.
- Dean’s or career advising office: Many schools have dedicated staff to review and analyze unsuccessful applications.
- Mentors in your specialty: Ask a trusted attending or senior resident to review your full ERAS application, not just your CV.
- Self-audit: Compare your application against NRMP and specialty-specific data (Charting Outcomes, Program Director Survey, specialty society guidelines).
Document your findings in writing. This will form the basis of your reapplication improvement plan.
1. Structured Self-Assessment and Strategic Planning
Once you understand the likely reasons you didn’t match, convert those insights into a structured plan.
Conduct a Personal SWOT Analysis
A SWOT (Strengths, Weaknesses, Opportunities, Threats) analysis is a simple but powerful way to organize your thinking.
Strengths
- Examples: strong Step 2 CK score, honors in key clerkships, excellent bedside manner, prior leadership, bilingual skills.
- How can you highlight these more effectively in your next application?
Weaknesses
- Examples: low Step score, failed exam, gap in training, limited U.S. clinical experience, weak letters, late graduation.
- Which weaknesses are modifiable in the next 6–12 months, and which are fixed but explainable?
Opportunities
- Examples: potential research positions, observerships, prelim or transitional year positions, quality improvement projects, teaching roles.
- Which options are realistic given your location, timing, visa status, or personal responsibilities?
Threats
- Examples: increasing competitiveness of your specialty, financial constraints, immigration/visa issues, family obligations, needing to retake exams.
- How will you mitigate or plan around these?
Build a Concrete Reapplication Timeline
Treat reapplying like a project:
12–15 months before Match
- Begin clinical or research positions
- Plan any exam retakes (USMLE/COMLEX)
- Start exploring backup specialties if needed
6–9 months before ERAS opens
- Secure letter writers
- Begin drafting personal statements
- Decide on Geographic preferences and program list strategy
3–4 months before ERAS submission
- Finalize personal statement and CV
- Confirm completion of observerships/externships
- Update ERAS with new experiences and publications
Clarity and structure will reduce anxiety and keep your efforts focused.

2. Enhancing Clinical Experience and Demonstrating Ongoing Growth
Strong, recent clinical experience is one of the most persuasive ways to show growth between application cycles—especially if you have gaps in training or have already graduated.
High-Impact Forms of Clinical Experience
U.S. Clinical Experience (USCE) for IMGs
- Observerships, externships, sub-internships, or hands-on roles in U.S. hospitals or clinics
- Prioritize:
- ACGME-affiliated institutions
- Experiences directly related to your target specialty
- Roles where you can be evaluated and obtain strong LoRs
Volunteer Clinical Roles
- Free clinics, community health centers, mobile clinics, telehealth support roles
- Focus on responsibilities that demonstrate:
- Direct patient interaction
- Continuity of care
- Cultural competence and service to underserved populations
Gap-Year Clinical Jobs
- Clinical research coordinator, medical scribe, clinical assistant, or case manager
- These roles help:
- Maintain your clinical reasoning and documentation skills
- Generate powerful, specific letters of recommendation
- Demonstrate professionalism and reliability
Military or Public Health Service
- Opportunities with the U.S. Public Health Service, National Health Service Corps, or military medicine (if eligible)
- These environments showcase leadership, resilience, and service—qualities valued across specialties.
Making Clinical Experiences Count on Your Application
Simply listing experiences is not enough. To maximize impact:
- Highlight recentness: Programs want to see you remain clinically engaged.
- Emphasize skills and outcomes: For each experience, note what you did and what you learned—e.g., “managed medication reconciliation for 15–20 patients daily” or “participated in weekly interdisciplinary rounds.”
- Align experiences with your target specialty: E.g., for Internal Medicine, emphasize inpatient and chronic disease management; for Pediatrics, emphasize communication with families.
3. Addressing Your Academic Record and Examination Performance
Academic metrics remain a core part of Residency Application screening. If your previous application was limited by USMLE/COMLEX scores or academic issues, you must show clear and credible improvement.
Strengthening USMLE/COMLEX Performance
Retakes (where allowed/appropriate)
- If you failed an exam or scored significantly below average:
- Consider retaking (if permitted) with a structured plan: formal prep course, question bank schedule, weekly self-assessments.
- Document your changes in strategy (tutoring, study groups, additional resources).
- Improved scores can:
- Demonstrate resilience and growth
- Help reassure programs about your ability to pass future in-training and board exams
- If you failed an exam or scored significantly below average:
USMLE Step 3
- For some applicants—especially IMGs or those with older graduation dates—passing Step 3 before reapplying can:
- Show clinical reasoning competency
- Reduce perceived risk for the program
- Strengthen visa sponsorship arguments (for some institutions)
- For some applicants—especially IMGs or those with older graduation dates—passing Step 3 before reapplying can:
Academic Enrichment: Beyond Test Scores
Post-Baccalaureate or Master’s Programs
- Special Master’s Programs (SMPs) in biomedical sciences, public health, or clinical research
- These can:
- Provide fresh, recent academic performance to offset older records
- Offer structured research and mentoring opportunities
- Generate strong academic LoRs
Targeted Coursework and Certificates
- Examples: biostatistics, epidemiology, health policy, quality improvement, or medical education
- Short courses or certificates (e.g., online from reputable institutions) can:
- Support your research involvement
- Align with your specialty (e.g., QI for Internal Medicine, epidemiology for Infectious Disease interest)
Document all academic improvements clearly in your ERAS entries, and be prepared to briefly and confidently explain any prior academic difficulties in interviews.
4. Crafting a Stronger, More Authentic Personal Statement
Your personal statement is more than a narrative; it is your chance to show programs how you’ve grown since your last application and why you remain committed to this path.
Key Goals for a Reapplicant Personal Statement
Show reflection and insight—not excuses
- Acknowledge that your journey has not been linear, but focus on what you learned and how you changed.
- Avoid blaming others, the system, or circumstances; emphasize accountability and adaptation.
Clarify your specialty choice
- Explain why this specialty remains the best fit for your skills, values, and goals, especially after a setback.
- Give specific examples of clinical encounters or experiences that shaped this decision.
Demonstrate growth and resilience
- Highlight the concrete steps you took after not matching:
- Clinical experience obtained
- Research or QI projects completed
- USMLE Preparation changes and improved performance
- New mentorship or leadership roles
- Highlight the concrete steps you took after not matching:
Practical Personal Statement Tips for Reapplicants
- Start with a focused, specific story—not a cliché (“I have always wanted to be a doctor…”).
- Avoid rewriting your previous statement with minor edits; create a fresh, updated narrative.
- Include details that differentiate you: language skills, unique volunteer experiences, or nontraditional background.
- Have multiple reviewers:
- A mentor in your specialty
- Someone strong in writing and editing
- Ideally, someone who has served on residency selection committees
In your story, show programs that you’re not just older—you’re wiser, more deliberate, and better prepared.
5. Building Stronger Letters of Recommendation and Professional Relationships
Letters of Recommendation can make or break a Residency Application—especially for reapplicants. You need letters that go beyond generic praise and provide specific evidence of your readiness for residency.
How to Secure Strong, Impactful LoRs
Choose writers who truly know you
- Prefer attendings who have observed you directly in:
- Clinical care
- Research or QI projects
- Longitudinal roles (over weeks or months, not days)
- Prefer attendings who have observed you directly in:
Prioritize specialty-specific letters
- For most specialties, you should have at least:
- 2–3 letters from attendings in that specialty
- 1 additional letter from another physician or supervisor who can speak to your character and work ethic
- For most specialties, you should have at least:
Provide helpful materials to your writers
- Updated CV and ERAS draft
- Your personal statement
- A short summary of:
- Your career goals
- Key experiences you shared with them
- Any growth you have demonstrated since not matching
Stay connected and follow up professionally
- Check in periodically with letter writers
- Notify them when ERAS opens and provide deadlines well in advance
- Thank them and update them on your Match outcome, regardless of result
Strong, recent, specialty-focused letters are one of the most concrete ways to show programs that you are residency-ready now—even if your earlier application fell short.
6. Networking, Professional Visibility, and Strategic Application Planning
In a competitive Match environment, who knows you (and who you know) can open doors. Effective networking is more than social media—it’s about building genuine professional relationships that yield mentorship, advocacy, and opportunities.
Practical Networking Strategies
Join Specialty Societies and Local Chapters
- Examples: ACP, AAP, APA, ACOG, ACEP, etc.
- Benefits:
- Access to mentorship programs
- Educational webinars
- Networking events with program directors and faculty
Attend Conferences and Regional Meetings
- Present posters or case reports if possible (even single-case projects can be presented).
- Introduce yourself to:
- Faculty from programs you’re interested in
- Potential mentors who may later support your application
Use Professional Social Media Thoughtfully
- LinkedIn: Maintain an updated, professional profile mirroring your ERAS content.
- X (Twitter): Follow residency programs, specialty societies, and educators; engage with journal clubs and academic discussions.
- Avoid unprofessional content across all platforms—programs do sometimes look.
Smart Application Strategy: Breadth, Fit, and Flexibility
Broaden your program list
- Include a mix of:
- Academic and community programs
- Different geographic regions
- A range of competitiveness levels
- Include a mix of:
Consider backup specialties
- If your chosen field is extremely competitive (e.g., Derm, Ortho, Radiology):
- Explore related fields that genuinely interest you (e.g., Internal Medicine, Family Medicine, Pathology).
- Ensure your application to backup specialties is authentic, not obviously “second choice.”
- If your chosen field is extremely competitive (e.g., Derm, Ortho, Radiology):
Be realistic and evidence-based
- Review NRMP “Charting Outcomes” and specialty match data.
- Seek honest input from mentors about your target specialty and competitiveness.
Career Development sometimes requires flexibility; exploring related specialties is not “giving up”—it’s adapting to the reality of the Match while preserving your core goal of practicing medicine.
7. Using a Gap Year Intentionally and Productively
If you are reapplying, you effectively have a “gap period” between Match cycles. How you use this time will significantly affect how programs perceive you.
High-Value Gap-Year Activities
Clinical Research or QI Positions
- Work as a research coordinator or research assistant in your specialty of interest.
- Aim to:
- Participate in manuscripts, abstracts, and poster presentations
- Contribute to quality improvement projects that relate to patient safety, outcomes, or workflow
Teaching and Educational Roles
- Tutor medical students or pre-med students in anatomy, physiology, or USMLE Preparation.
- Serve as a teaching assistant or small-group facilitator if opportunities exist.
- These roles showcase communication skills, leadership, and professionalism.
Additional Degrees or Certificates
- MPH, MS in Clinical Research, or other relevant advanced degrees can:
- Deepen your skill set
- Help you stand out in academic programs
- MPH, MS in Clinical Research, or other relevant advanced degrees can:
How Programs Interpret Your Gap Year
Programs will ask, explicitly or implicitly: “What did this applicant do after not matching?” You want to be able to respond:
“I used this year to strengthen my clinical skills, expand my research exposure, and reflect on how to become a better future resident and physician.”
That clear narrative, backed by concrete experiences, can transform a previous unsuccessful Match into a story of resilience and growth.
FAQs About Reapplying for Residency
1. Should I address my previous unsuccessful Match in my personal statement or interviews?
Yes—but briefly and constructively. You do not need to dwell on it in your personal statement, but you can:
- Acknowledge that you previously applied.
- Emphasize what you learned from the experience.
- Highlight the specific steps you took to strengthen your application (clinical work, improved scores, research, mentorship).
In interviews, be ready with a concise, honest, and forward-looking explanation. Avoid blaming others; focus on growth and readiness now.
2. Can I apply to a new specialty when reapplying for residency?
You can—and for some applicants, it is a wise move. Consider applying to a new specialty if:
- Your previous choice is extremely competitive relative to your metrics.
- Your experiences and strengths align more naturally with another field.
- You can obtain at least 1–2 strong specialty-specific letters and relevant clinical exposure before the next cycle.
If you do apply to a new specialty, make sure your Personal Statement Tips, LoRs, and experiences clearly support that choice.
3. How long should I wait before reapplying to residency?
Most applicants reapply in the very next cycle, using the intervening year to:
- Gain clinical or research experience.
- Improve USMLE/COMLEX performance (if needed and feasible).
- Strengthen letters and refine their application strategy.
Waiting more than one year may be reasonable if you are pursuing a degree (e.g., MPH) or completing a multi-year research position—but you should ensure you maintain some form of clinical connection during that time.
4. Are there programs or resources that specifically support reapplicants?
Yes. Helpful resources include:
- Your medical school’s advising and career development office: Many have reapplicant-focused advising.
- Specialty organizations: Some offer mentorship programs or webinars for unmatched applicants.
- Online forums and official NRMP/ERAS resources: Provide timelines, data, and process guidance.
- Institutional “pre-residency” or research fellow positions: Some departments informally view these as pipelines into their residency programs.
Always prioritize credible, official sources and trusted mentors over anonymous online opinions.
5. How do I handle weaknesses like low USMLE scores or failed exams in my application?
You cannot change the past, but you can shape how it is perceived:
- Be honest and factual—never attempt to hide or misrepresent exam history.
- Show evidence of improvement (retakes, better subsequent exams, Step 3 passed).
- Demonstrate consistent clinical performance, strong letters, and professionalism.
- If asked in interviews, briefly explain contributing factors, but focus on:
- What you changed
- How your recent performance reflects your true capability
Residency programs are often more forgiving of earlier missteps when they see a consistent upward trajectory and a mature, reflective applicant.
Reapplying for residency is demanding—but it can also be one of the most clarifying and formative phases of your medical career. With honest self-assessment, targeted clinical and academic improvements, stronger Personal Statement Tips, and a strategic Residency Application plan, you can return to the Match as a more competitive, confident candidate.
Use this period not only to “fix” your application, but to grow into the kind of physician you aspire to be.






















