What to Do Next: Comprehensive Strategies for Unmatched Medical Graduates
Navigating the path to becoming a physician is demanding, competitive, and emotionally intense. For most medical students, the residency match represents a pivotal turning point in their Medical Career—confirmation that years of study, sacrifice, and dedication are moving them toward independent practice.
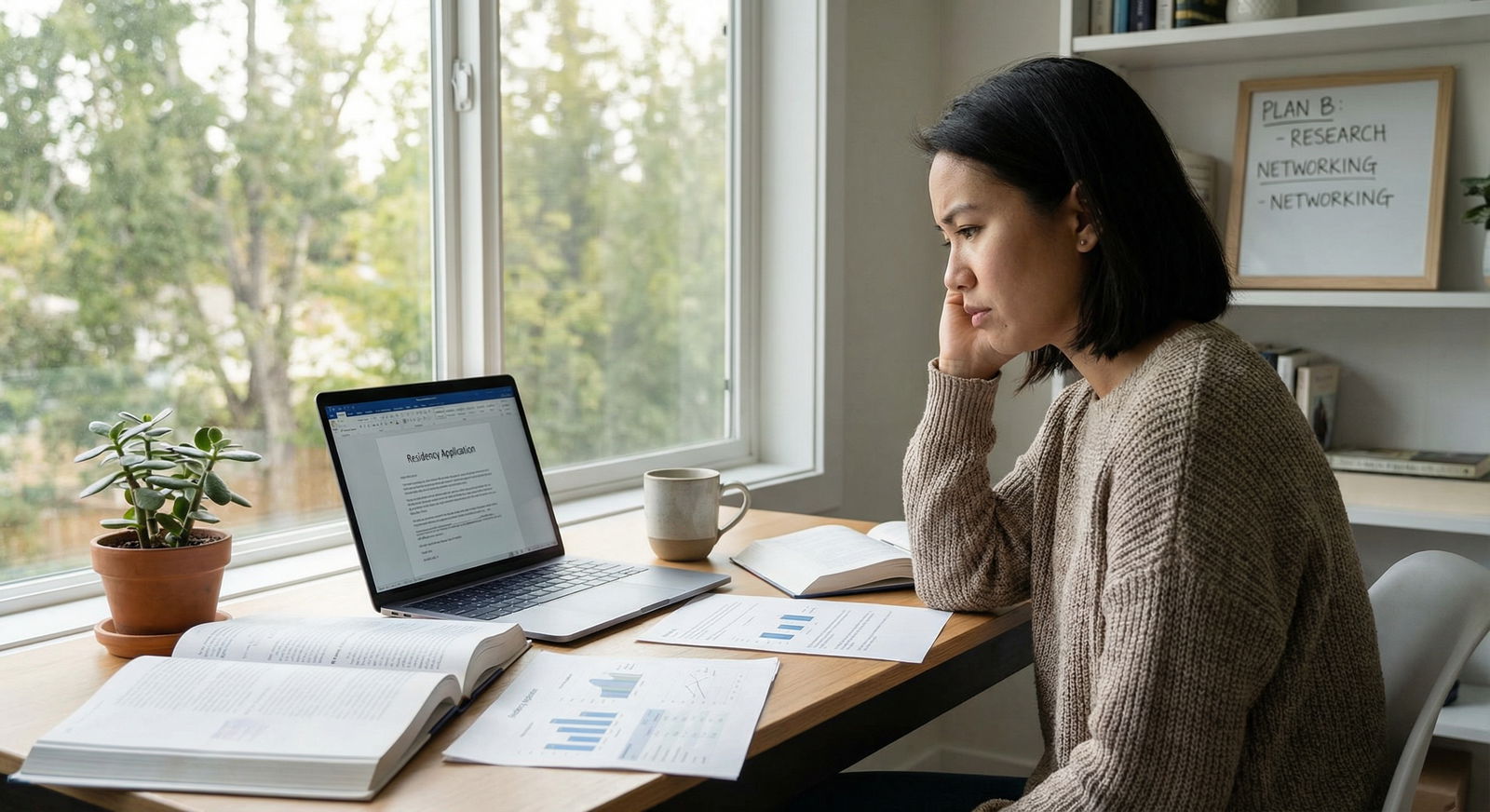
When Match Day arrives and you discover you are unmatched or partially matched, it can feel like the floor has dropped out from under you. This moment is often accompanied by shock, grief, shame, and fear about the future. Yet being unmatched, while painful, is not the end of your journey in medicine. Many physicians—now successful attendings, leaders, and educators—once stood exactly where you are.
This guide offers practical, step-by-step strategies to help you move from crisis to clarity. You’ll learn how to process what happened, understand why it occurred, make the most of the Supplemental Offer and Acceptance Program (SOAP), strengthen your application, and explore both traditional and alternative pathways in Health Education and clinical practice. Most importantly, you’ll see how to protect your Mental Health and rebuild confidence as you plan the next phase of your Career Development.
1. First Steps: Processing the Emotional Impact of Not Matching
Before you update your CV or email a program director, you need space to acknowledge what you’re feeling. The experience of not matching is a real loss—of expectations, plans, and a particular timeline for your life. Treat it as such.
1.1 Allow Yourself to Feel and Name Your Emotions
Common reactions include:
- Disappointment and grief
- Embarrassment or shame
- Anger at the system, schools, or yourself
- Anxiety about finances, visas, or future prospects
- Numbness and difficulty concentrating
These reactions are normal. What matters is not suppressing them but managing them constructively so they don’t paralyze you during a time when decisions must be made.
Practical steps:
- Give yourself 24–48 hours, if possible, before making major decisions.
- Journal your thoughts: “What am I most afraid of right now?” “What hurts the most?” This can clarify what actually needs addressing.
- Limit social media exposure temporarily, especially posts celebrating matches. Protect your Mental Health Support in this vulnerable window.
1.2 Talk to Supportive People—You Are Not Alone
Reach out to:
- Trusted friends or classmates (including those who did match). Many will be more supportive than you expect.
- Family members or partners who know your long-term goals.
- Faculty mentors or advisors who understand the Residency Match process.
- Peer or alumni groups that explicitly support unmatched or reapplicant students.
You may also consider:
- School wellness or counseling services
- Physician/trainee-specific mental health resources
- Online communities for unmatched medical graduates
Saying “I didn’t match” is hard, but isolation can make the experience far worse. Early, honest conversations often become the foundation for practical help and new opportunities.
2. Understanding Why You Didn’t Match: Honest, Data-Driven Reflection
Once you’ve had initial time to process, move into structured reflection. You need a clear, realistic understanding of what likely contributed to your unmatched status. This is the basis of any effective reapplication plan or alternative route in your Medical Career.

2.1 Review Your Application Components Systematically
Assess each key element of your application:
Board scores (USMLE/COMLEX or equivalent):
- Were your scores below the average for your specialty?
- Were there failures or score delays that weren’t addressed in your personal statement?
Clinical performance and evaluations:
- Any failed or repeated rotations?
- Honors, distinctions, or strong comments in core rotations relevant to your chosen specialty?
Letters of recommendation (LORs):
- Did you have at least 2–3 strong, specialty-specific letters from faculty who know you well?
- Were your letter writers well-known in your field, or at least able to provide detailed, substantive support?
Personal statement and application narrative:
- Did you clearly explain why you chose your specialty?
- Did you address any red flags (gaps, failures, career changes) directly and professionally?
- Did your story demonstrate growth, insight, and resilience?
CV and extracurricular profile:
- Did you have relevant research, leadership, teaching, or volunteer work?
- Any prolonged gaps in training or inconsistent involvement in medicine?
Interview performance:
- How many interviews did you receive?
- Did you feel prepared, or did you struggle with common questions?
- Did you practice with mock interviews and receive feedback?
Collect feedback from:
- Specialty advisors
- Faculty who reviewed your previous materials
- Program directors or residents (if they’re willing to discuss your application)
Ask for specific, not vague, feedback: “If I were to reapply, what would you consider my top 2–3 areas for improvement?”
2.2 Evaluate Your Specialty Selection and Application Strategy
Sometimes a strong applicant doesn’t match because of strategy rather than inherent weakness.
Reflect on:
Competitiveness of your chosen specialty (e.g., dermatology, plastic surgery, orthopedic surgery, neurosurgery).
Number and range of programs:
- Did you apply broadly enough, including community and less well-known programs?
- Did you apply to a balanced range of locations, not just a few cities or regions?
Dual-application strategy:
- Did you consider applying to a second, less competitive specialty or a transitional/preliminary year in medicine or surgery?
- If you did, was your application tailored effectively for each specialty?
This analysis will guide whether you should:
- Reapply to the same specialty with a stronger profile,
- Apply more broadly within the same specialty,
- Or seriously consider a different specialty that better matches your credentials, interests, and life goals.
3. Maximizing Your Chances Through SOAP (Supplemental Offer and Acceptance Program)
For unmatched and partially matched candidates in NRMP-participating programs, the SOAP is often the first actionable path forward. It can be intense and fast-paced, but with preparation, it can lead to excellent training opportunities.
3.1 Prepare Logistically and Emotionally for SOAP
Before SOAP begins:
- Ensure your ERAS application is updated (experiences, personal statement, CV).
- Obtain at least one SOAP-specific personal statement, especially if applying to a different specialty or broader set of programs.
- Confirm you have reliable internet, quiet workspace, and a charged phone during SOAP days.
Know the SOAP timeline for your match year (available on NRMP and ERAS websites):
- When the list of unfilled programs will be released
- Application submission windows
- Rounds of offers and response deadlines
3.2 Apply Strategically During SOAP
Approach SOAP like a targeted, rapid version of the Residency Match:
Be flexible, but intentional:
- Consider specialties related to your skills (e.g., Internal Medicine, Family Medicine, Psychiatry, Pediatrics) if they align with your long-term goals.
- If you’re switching specialties (e.g., from a surgical field to Internal Medicine), adjust your materials to demonstrate genuine interest and preparation.
Tailor quickly but meaningfully:
- Modify your personal statement to address why you’re interested in that specialty or program type.
- Highlight any experiences relevant to primary care, inpatient medicine, psych, etc.
Stay responsive:
- Keep your phone nearby and email notifications on.
- Respond to any communication from programs promptly and professionally.
3.3 Realistic Expectations and Success Stories
SOAP can feel unpredictable, but many unmatched students:
- Match into solid categorical positions they hadn’t considered initially
- Discover specialties that ultimately fit their values and strengths better than their original choice
- Gain preliminary or transitional year positions that later facilitate entry into advanced residencies
Maintain a mindset of: “I am looking for a place where I can learn, grow, and serve patients,” rather than focusing solely on prestige or location.
4. Considering a Gap Year: Turning a Setback into Strategic Growth
If SOAP doesn’t result in a match—or if you decide a more thorough reset is necessary—a structured gap year can significantly strengthen your application and clarify your direction.
4.1 Designing a Purposeful Gap Year
A successful gap year for Career Development in medicine usually includes one or more of the following:
Clinical Experience
- Clinical research coordinator, research fellow, or sub-investigator
- Medical assistant, scribe, or clinical observer in outpatient or inpatient settings
- Postgraduate sub-internships or visiting rotations (where available and permitted)
Benefits:
- Maintain clinical skills and exposure
- Earn new letters of recommendation
- Demonstrate ongoing commitment to patient care
Research and Academic Productivity
- Join a research group in your target specialty or a related field.
- Aim for tangible outputs:
- Abstracts and posters at national/local conferences
- Manuscripts (case reports, retrospective studies, reviews)
- Quality improvement or patient safety projects
Highlight these achievements in your next application cycle to stand out.
Teaching and Medical Education
- Participate in tutoring or teaching (medical students, undergraduates, MCAT prep).
- Serve as a teaching assistant or curriculum developer at your institution.
- Engage in simulation training, OSCE prep, or anatomy labs if available.
Teaching shows communication skills, leadership, and a commitment to Health Education—qualities valued across all specialties.
4.2 Networking: Building Relationships That Open Doors
Use your gap year to create and deepen professional connections:
- Attend specialty conferences, local medical society meetings, and grand rounds.
- Request informational interviews with attendings and program directors:
- Ask about what they look for in applicants.
- Seek honest feedback on your profile.
- Stay in touch with mentors through periodic updates:
- Brief emails summarizing your current work and progress.
- Requests for advice as you approach the next Match cycle.
Networking is not about asking for favors; it’s about building genuine professional relationships rooted in respect and shared goals.
5. Strengthening Your Future Application: From Good to Unmistakably Strong
Once you have a clear understanding of what went wrong and how you’ll spend the coming months, focus on upgrading each element of your application for the next Residency Match cycle.
5.1 Revise Your Personal Statement and Overall Narrative
Your personal statement should:
Tell a cohesive story that connects your past experiences, current activities, and future goals.
Address prior setbacks (exam failures, LOA, being unmatched) briefly and constructively:
- What happened?
- What did you learn?
- How have you grown?
Reflect clarity about why you are now a stronger, more resilient candidate.
Align clearly with the specialty’s values (e.g., continuity of care for Family Medicine, team-based care for Internal Medicine, neurobiology and psychotherapy for Psychiatry).
Have at least two experienced readers—ideally in your target specialty—review your statement for content, tone, and clarity.
5.2 Upgrade Your Letters of Recommendation
Focus on obtaining new or updated letters that:
- Reflect your most recent clinical, research, or teaching work.
- Speak to growth since your previous application.
- Are written by supervisors who:
- Directly observed you in clinical or academic settings.
- Understand residency expectations.
- Can comment on your professionalism, teamwork, communication, and reliability.
Provide letter writers with:
- Your updated CV
- Brief summary of your goals and what you’d like them to emphasize
- Clear deadline and submission instructions
5.3 Improve Interview Skills and Professional Branding
Many strong paper applicants fail to match due to weak interviews. Address this head-on:
- Schedule mock interviews with faculty, advisors, or professional coaches.
- Record yourself answering common questions:
- “Tell me about yourself.”
- “Why this specialty?”
- “Tell me about a time you failed and what you learned.”
- “Walk me through your path since medical school graduation.”
- Practice virtual interview etiquette if interviews are remote:
- Lighting, camera angle, sound quality
- Professional background and attire
Seek feedback on:
- Clarity and organization of responses
- Nonverbal communication
- How well you address prior setbacks without sounding defensive
6. Reassessing Specialty Fit and Exploring Alternative Career Pathways
Not matching can prompt an important—and sometimes overdue—question: “Is this specialty truly the best fit for me, my skills, and my long-term vision?”
6.1 Reconsidering Your Specialty Choice
Evaluate honestly:
- Does your chosen specialty match your:
- Academic record and exam performance?
- Personality and working style (procedural vs cognitive, inpatient vs outpatient, continuity vs episodic care)?
- Life priorities (family, geography, work-life balance)?
Consider speaking with:
- Faculty from multiple specialties
- Residents who switched specialties
- Career development advisors at your institution
If you decide to switch specialties:
- Spend time shadowing or rotating in the new field.
- Adjust your application materials to reflect this shift clearly and authentically.
- Secure specialty-specific letters from your new field.
6.2 Exploring Non-Traditional or Alternative Medical Career Options
While residency is the most common path, your medical degree can open diverse doors in healthcare and beyond. Some unmatched graduates choose to pursue or temporarily explore:
Clinical Research and Trials
- Roles as a research fellow or coordinator in academic medical centers or industry.
- Opportunity to publish, present, and build a strong academic profile.
Pharmaceutical, Biotech, and MedTech Industry
- Medical science liaison (MSL)
- Clinical affairs or pharmacovigilance roles
- Medical affairs and regulatory roles
Public Health and Policy
- MPH programs
- Work with NGOs, government agencies, or global health organizations
- Roles focused on health systems, epidemiology, or health equity
Medical Education and Academic Support
- Teaching anatomy, physiology, clinical skills, or USMLE prep.
- Curriculum development and simulation-based training roles.
Some individuals stay in these roles long-term and find them deeply fulfilling. Others use them to re-enter the match later with a stronger and more differentiated profile in Health Education or healthcare leadership.
7. Protecting Your Mental Health and Well-Being Throughout the Process
Being unmatched is not just a professional setback; it is an emotional challenge that can affect your sense of identity and self-worth. Deep, proactive Mental Health Support is essential.

7.1 Establish Routine and Structure
Without a residency schedule, days can quickly become unstructured, which may worsen anxiety or depression.
Build a weekly plan that includes:
- Scheduled work or study blocks
- Exercise (even 20–30 minutes of walking daily)
- Time for social connection
- Hobbies or restorative activities (music, art, reading, faith/spiritual practice)
7.2 Recognize When Professional Help Is Needed
Seek professional mental health support if you experience:
- Persistent sadness, hopelessness, or guilt
- Loss of interest in activities you previously enjoyed
- Significant changes in sleep, appetite, or energy
- Thoughts of self-harm or feeling that your life is over because you didn’t match
You are not your match status. Many excellent physicians and healthcare professionals have struggled with similar feelings and benefited from therapy, peer support, or medication when needed.
8. Planning Strategically for the Next Match Cycle
If you decide to reapply, approach the process with intention, organization, and resilience.
8.1 Create a Detailed Timeline
Work backward from the next application deadline and identify milestones:
- When to finalize your specialty decision
- Deadlines for research projects, abstracts, or manuscripts
- When to secure new letters of recommendation
- Personal statement draft and revision deadlines
- Target date to complete mock interviews
Use a spreadsheet or project management tool to track:
- Programs you’re considering
- Their requirements and average metrics
- Application status and interview invitations
8.2 Apply Broadly, but Thoughtfully
Based on your revised profile and specialty choice:
- Apply to a sufficient number of programs, including community and less competitive sites.
- Consider multiple geographic regions, not just highly desirable cities or states.
- If appropriate, include a dual-application strategy (e.g., Internal Medicine + Family Medicine, Psychiatry + Neurology), ensuring each has tailored materials.
Frequently Asked Questions (FAQ)
Q1: What should I do in the first 48 hours after learning I didn’t match?
Focus on immediate emotional support and information-gathering:
- Allow yourself to feel and name your emotions.
- Reach out to a trusted mentor, advisor, or dean’s office for guidance on SOAP eligibility and logistics.
- Review official NRMP and ERAS communications so you understand your options.
Avoid making major, irreversible decisions (like abandoning medicine) in this early emotional period.
Q2: How do I know if I should reapply to the same specialty or switch?
Consider:
- How your metrics (scores, grades, research) compare to matched applicants in that specialty.
- Honest feedback from faculty and program directors.
- Whether your core interests, personality, and long-term goals align better with another field.
If your passion for the specialty remains strong and advisors believe your profile can become competitive with a targeted gap year, reapplying may be reasonable. Otherwise, seriously explore alternative specialties that match your strengths and values.
Q3: Will being unmatched permanently harm my Medical Career?
Being unmatched is a setback, not a permanent label. Many physicians who initially didn’t match:
- Successfully matched on a second or third attempt
- Became respected attendings, program directors, researchers, and educators
- Gained resilience and insight that later benefited their patients and trainees
Your future colleagues are more interested in how you responded to adversity than in whether your path was perfectly linear.
Q4: Can I build a meaningful career in healthcare without completing residency?
Yes, though your practice options will be different. Some unmatched graduates choose long-term careers in:
- Clinical research and trials
- Pharmaceutical, biotech, and medtech companies
- Public health, policy, and health administration
- Medical writing, consulting, or medical education
While you may not practice as an independent physician without residency (depending on your region’s regulations), you can still have a significant impact on patient care and health systems.
Q5: How can I talk about being unmatched during future interviews?
Frame the experience as:
- A challenge that led to growth: improved clinical skills, research, or teaching.
- A catalyst for self-reflection and a clearer understanding of your goals.
- Evidence of resilience and persistence in pursuing your Medical Career.
Avoid blaming others or sounding bitter. Instead, be honest, concise, and solution-focused: what happened, what you learned, and how you’re now better prepared to succeed in residency.
Not matching is undeniably difficult, but it is also an inflection point—a moment to redefine your path, sharpen your skills, and reaffirm why you chose medicine. With thoughtful reflection, strategic action, and strong Mental Health Support, you can transform this setback into a powerful chapter in your journey toward a meaningful, impactful career in healthcare.






















