It is March 20th. Match Day has come and gone. Your name did not show up on a “Congratulations” email. The initial shock is fading, but now you are staring at the calendar doing the grim math: one year until the next Match.
You have two options. Drift for 12 months and send in basically the same application again. Or treat this as an actual reapplicant year—deliberate, structured, and frankly, aggressive.
Let us build the second path. Month by month.
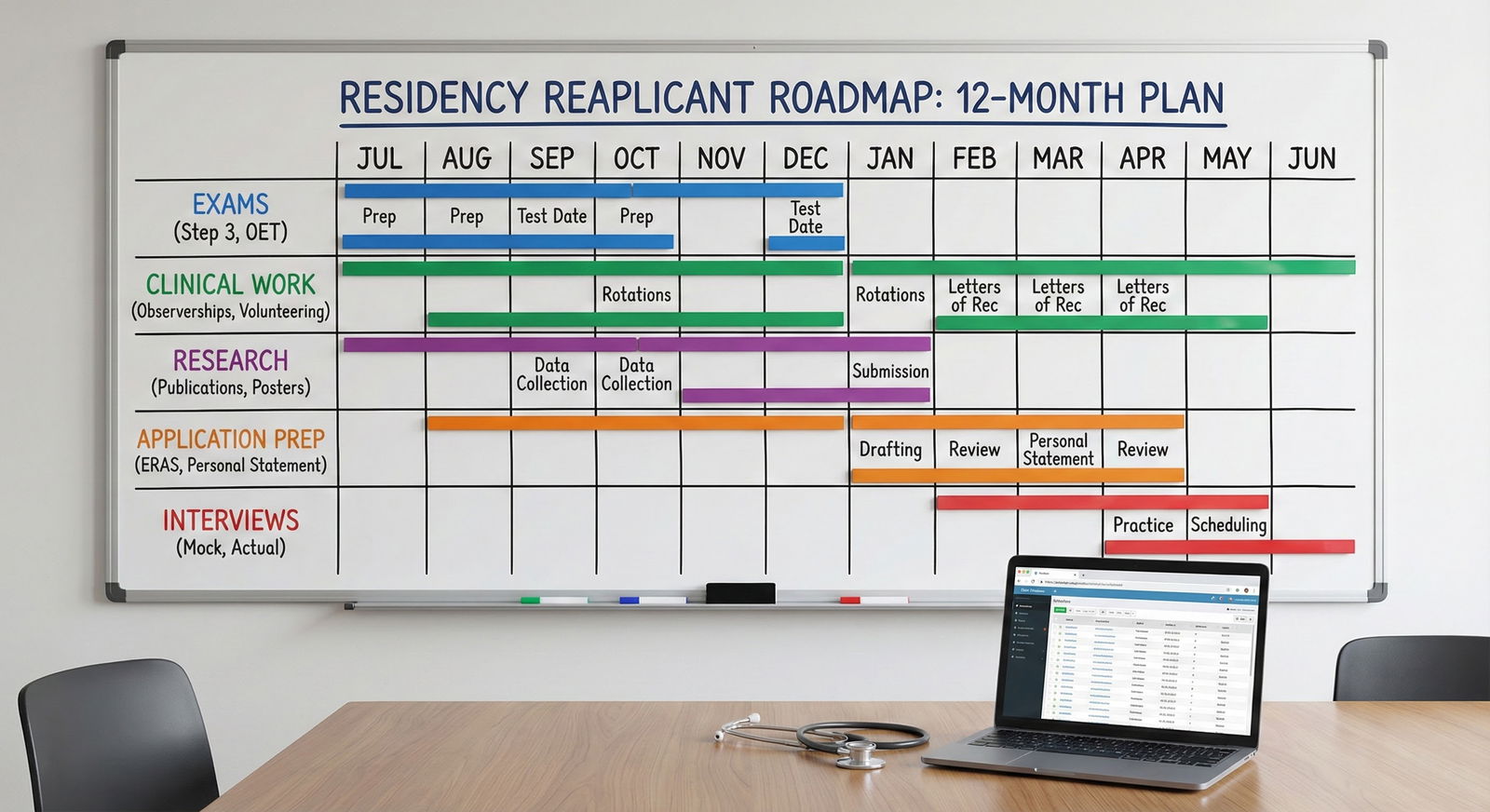
Big Picture: Your 12-Month Reapplicant Framework
Before we go month-by-month, anchor the year. A strong reapplicant plan usually hits four pillars:
- Clinical activity – recency, responsibility, strong letters
- Scores and exams – Step 2 CK, OET/IELTS for IMGs, outstanding failures
- Application quality – personal statement, experiences, program list, signaling
- Professional story – what you did with your “gap” year and why you are stronger now
Here is how the year typically breaks down.
| Phase | Months | Primary Focus |
|---|---|---|
| Debrief & Triage | 1–2 | Autopsy of last cycle, immediate fixes |
| Build Capital | 3–6 | Clinical work, research, exams, letters |
| Polish & Position | 7–9 | Application materials, program strategy |
| Execute | 10–12 | Applications, interviews, updates |
Now we walk it forward.
Months 1–2: Post-Match Autopsy and Immediate Triage
It is late March to May. At this point you should know exactly why you did not match—not just guess.
Week 1–2: Emotional reset and basic logistics
You are still raw. Fine. Give yourself a few days, not months.
By the end of week 2, you should:
- Download and save your entire ERAS application as a PDF
- Save your personal statement(s) and all LoRs
- Make a spreadsheet of every program you applied to, interviewed at, and their outcomes
- If you scrambled into a preliminary position or non-categorical spot, clarify contract dates and expectations
Do not start rewriting your personal statement yet. You are too close and too upset.
Week 3–4: Honest diagnostic
Now comes the part most reapplicants skip: a cold, brutal review.
At this point you should:
- Score yourself on basic competitiveness:
- Step 1: Pass/fail; Step 2 CK: exact score
- Any exam failures or repeats
- Class rank, AOA, red flags (leave, probations, professionalism issues)
- Review your interview volume:
- 0–2 interviews: your file likely had a filter/competitiveness problem
- 3–7 interviews: borderline competitiveness and/or weak application presentation
- 8+ interviews, no match: ranking strategy or interview performance problem
If possible, schedule short, focused conversations:
- Your dean’s office or career advising
- A trusted attending who knows your work
- For IMGs: an advisor at your school or a reputable IMG advising service
Ask them directly:
- “If you were a PD in [my specialty], would you interview my file as is?”
- “Would you strongly recommend I reapply to the same specialty or pivot?”
Common failure patterns (and what they imply)

| Category | Value |
|---|---|
| Insufficient interviews | 40 |
| Low Step 2 CK | 25 |
| Weak letters | 10 |
| Poor interview | 15 |
| Overly competitive specialty | 10 |
If you recognize yourself in:
- Insufficient interviews (filter issues)
- Likely culprits: low Step 2 CK, late application, poor program list, visa status, weak school reputation
- Good number of interviews, no match
- Likely culprits: interview skills, ranking strategy (ranking too few or hyper-competitive programs), interpersonal red flags
- Nontraditional or IMG with no US clinical
- Core problem: PDs do not trust your readiness for their system
Write your primary problems down. Top 3. In plain language.
This list will drive your year.
Months 3–4: Decide Your Strategy and Start Building Substance
It is April–May. At this point you should be choosing your path, not just “seeing what happens.”
Step 1: Specialty decision (do not drag this out)
By end of April, you should have made a decision among:
- Reapply same specialty, same strategy – Rarely wise unless you were very close (e.g., 10+ interviews, narrowly did not match).
- Reapply same specialty, stronger application – Most common scenario. You improve letters, CK, clinical year.
- Pivot to a less competitive specialty – IM → FM, gen surg → prelim → another field, derm → IM, etc.
- Dual apply – E.g., IM + FM, Anesth + IM. Risky but sometimes necessary.
Here is the blunt truth: if you had <5 interviews and a sub-220 Step 2 CK (or equivalent) for a competitive specialty (derm, ortho, plastics, neurosurg, ENT, ophtho, integrated IM, etc.), you probably need to pivot or dual-apply.
Step 2: Lock in what you will be doing for the next year
By early May, you should be actively securing one of the following:
- Transitional/prelim year you already matched into
- Research year (ideally in your target specialty or at least internal medicine)
- US clinical work:
- Paid: hospitalist extender, clinical research coordinator, scribe in specialty clinics
- Unpaid: observer, extern, post-doc with patient exposure
- Teaching or academic roles: chief year, teaching fellow
You want activities that:
- Generate strong letters
- Show current clinical engagement
- Make sense in your narrative (“I spent this year deepening my skills in X”)
If you currently have nothing for the upcoming year, your immediate weekly checklist should include:
- Sending targeted emails to program coordinators and faculty asking about:
- Research assistantships
- Gap-year positions
- Observerships / externships
- Using alumni networks and cold-emailing with a clear 1-page CV and direct ask
Months 5–6: Build Clinical and Academic Capital
It is June–July. Next cycle opens in September. This is where many reapplicants blow it—they assume that since they only have a few months before ERAS, nothing they start now will matter.
Wrong. Programs care deeply what you did this year. Even if the letter comes later, the activity itself counts.
At this point you should be:
Firmly in a structured role
- Research assistant in cardiology working on retrospective chart reviews
- Full-time scribe in an ED seeing high-volume US clinical practice
- Non-categorical intern showing you can handle inpatient work
- IMG in back-to-back US clinical rotations
Setting up new letters of recommendation
- Tell your attending up front: “I am a reapplicant planning to apply in [specialty] this fall. I will be asking for a letter at the end of this rotation. I hope to demonstrate sustained improvement in [X, Y].”
- Ask for concrete feedback mid-rotation. You want to know if they will actually support you strongly.
Addressing exam issues
- If Step 2 CK is weak and you are allowed a retake or Step 3 before applications, schedule it.
- For IMGs, handle OET/IELTS or any licensing exam early.
Timeline for exam work

| Category | Value |
|---|---|
| Mar | 0 |
| Apr | 10 |
| May | 30 |
| Jun | 60 |
| Jul | 80 |
| Aug | 95 |
| Sep | 100 |
Interpretation:
- March–April: Assess whether you even need more exams
- May–July: Active prep phase (content + question banks)
- August: Take Step 3 or language exams if relevant
- September: Results ideally in by or shortly after ERAS opening
Months 7–8: Rebuild Your Application Core
It is August. ERAS opens in a few weeks. At this point you should be deep in material overhaul, not just touch-ups.
Week 1–2 of Month 7: Rewrite, do not “edit,” your personal statement
Your previous PS was attached to a failed cycle. Do not recycle.
This year your PS must:
- Explicitly but briefly acknowledge the gap / reapplicant year:
- One sharp sentence is usually enough: “After not matching last year, I committed myself to…”
- Highlight what changed:
- New responsibilities, fresh clinical experience, research, exam improvements
- Match the specialty: if you pivoted, your narrative must justify that pivot without sounding like you “gave up”
Common mistake: three paragraphs of “I learned resilience from not matching.” No. One paragraph at most. Then show your growth through concrete work.
Week 3–4 of Month 7: Rebuild your experiences and CV
At this point you should:
- Add every meaningful responsibility from this year:
- “Clinical Research Coordinator, cardiology clinic – coordinated care for 50+ heart failure patients…”
- “Non-categorical surgery intern – managed 10–15 inpatients daily…”
- Trim filler:
- Drop ancient, low-impact undergrad clubs that clutter your story
- Update each entry with:
- Scope (numbers, frequency)
- Your specific role
- Outcomes (papers, QI projects, improved systems)
Your most recent year should clearly be your strongest.
Month 9: Program List, Signals, and Strategy
It is early September. ERAS is opening. This is where strategy wins or loses your reapplication.
At this point you should have:
A realistic program list
- If you are a reapplicant with an average profile, 80–120 programs in IM/FM is not insane. For competitive specialties, more targeted but still broad within reason.
- Heavy emphasis on:
- Community programs
- Mid-tier academic centers
- States that traditionally take more IMGs or reapplicants (for IMGs)
A clear geographic and “tier” distribution Avoid the trap of:
- 30 applications to hyper-competitive coastal academic centers
- 10 to realistic community programs
Your distribution should be flipped.
Signaling or preference strategies (if your specialty uses them)
- Use signals on places that might actually rank you
- Do not burn signals on brand-name reach programs that never interviewed your profile group before
- Leverage any existing connections (research, rotations, hometown)
Month 10: Application Submission and Early Season
It is late September to October. ERAS is in. At this point you should be proactive but not desperate.
Immediately after submission (Week 1–2)
- Send targeted update emails to:
- Programs where you rotated
- Programs where you have research connections
- PDs or APDs who explicitly invited updates
- Keep these short:
- 1 paragraph: who you are, connection to program
- 1 paragraph: succinct highlight of what is new this year
- Offer to send full CV
Do not send mass, generic “Dear Program Director” spam. That gets ignored.
Weeks 3–4: Interview invitations begin
This is where your reapplicant year starts to pay off.
At this point you should:
- Have your interview answers updated to incorporate your reapplicant story:
- “Tell me about yourself”
- “I see you are a reapplicant—what changed?”
- “Why this specialty / why now?”
- Practice saying, calmly and confidently:
- “I did not match last year. In response, I spent this year doing X, Y, and Z, which clarified my commitment to [specialty] and made me a stronger applicant.”
What you must avoid:
- Blaming previous programs, visa issues, or “the system”
- Sounding bitter
- Sounding like you are apologizing constantly
Months 11–12: Interview Season, Rank List, and Contingency Planning
It is November–February. You are in the thick of it again. This is where prior experience as an applicant should give you an edge.
During interviews (Month 11)
At this point you should:
- Be consistent with your story across programs
- Bring your year’s work into specific answers:
- “In my current role as a non-categorical intern, I have been managing…”
- “My current research in [X] has taught me…”
You will be asked about:
- Why you did not match previously
- What you learned
- How they can be confident it will not happen again
Have one clean, rehearsed, 60–90 second answer. Not a 7-minute saga.
Rank list strategy (Month 12)
When rank list opens, you must not repeat old mistakes.
Common reapplicant rank errors I have seen:
- Ranking only “dream” programs where you felt the day went well
- Leaving off solid community programs because your ego hated them
- Short lists (<8–10 programs) when you had more interviews
At this point you should:
- Rank every program where you would actually show up to work
- Not “game” the algorithm with strange permutations
- Be honest about where you are actually competitive
Special Cases: Prelim Year Reapplicants and Major Red Flags
If you are in a prelim or non-categorical year
Your task list is more intense:
- Excel clinically. You need your PD and attendings to say you are a top resident.
- Get at least one program director letter. These are gold.
- Do not get caught up in intern-year drama (lateness, notes unfinished, staff conflicts). PDs talk.
By mid-year (around January), you should:
- Have met with your PD and said clearly:
- “I am reapplying in [specialty]. I would appreciate your honest assessment and any support you can provide.”
If you have a major red flag (failure, professionalism issue)
This must be:
- Disclosed appropriately when asked
- Framed with:
- Ownership (no excuses)
- Specific actions you took to remediate
- Evidence of changed behavior over time
The reapplicant year is your proof of concept that the flag does not define you anymore.
One-Year Snapshot: How a Strong Reapplicant Year Looks
By the time you are submitting ERAS again, your narrative should be simple and believable:
- “Last year I applied with [X weaknesses].”
- “This year I have…”
- Completed [clinical/research role] with [specific responsibilities]
- Strengthened exams (Step 2/3, language, etc.)
- Earned new letters from US faculty who know my work well
- Clarified my specialty choice and can articulate why
Programs do not expect perfection. They do expect a trajectory. Flat lines do not match.
Today: Your First Concrete Step
Do not try to “fix the next 12 months” in one sitting. Start with one surgical move.
Today, right now:
- Open your old ERAS PDF and a blank document.
- Write down three specific reasons you believe you did not match—no euphemisms, no spin.
- Then, under each reason, write one concrete thing you will do in the next 3 months to attack it.
That one page becomes your reapplicant year roadmap. Print it. Put it above your desk.
You can refine the plan as you go. But the year only changes if you start directing it—today.






















