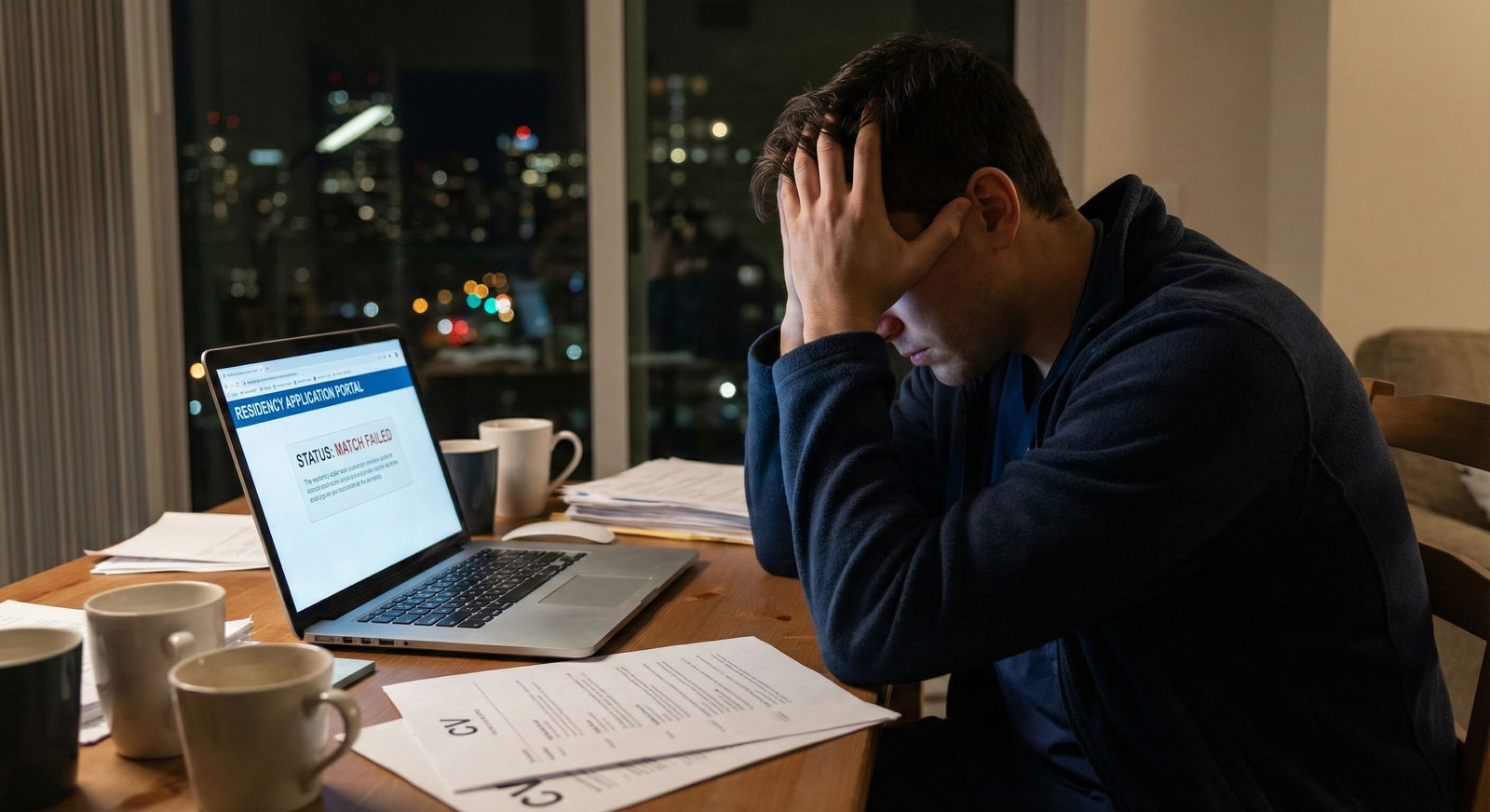
The biggest lie people tell unmatched applicants is: “If you want it badly enough and keep trying, it’ll all work out.”
Sometimes it doesn’t. And that’s exactly why you’re terrified.
You’re not just asking, “How do I improve my app?” You’re asking, “Am I delusional for still trying?” You’ve got multiple gaps, at least one failed Match, maybe more. You’ve watched classmates move on, get married, have kids, post “PGY-2 life” photos while you’re sitting there wondering if you’re just throwing good years after bad.
Let’s actually talk about that. Honestly. No fairy dust.
First: You’re Not Crazy for Being This Worried
You know what drives me nuts? The “just keep trying!” crowd who never once had to SOAP, never once saw their name not show up on Match Day.
Your brain is doing math you can’t turn off:
- Gap(s) after graduation
- Failed Match (maybe more than one)
- Maybe a Step failure or low score
- Maybe no recent clinical work
- Visa issues, no “home program,” weak letters…
So now every time you think, I’ll try again, a second voice says:
“What if I end up 35, still unmatched, broke, and totally unemployable?”
That’s not drama. That’s a legitimate fear.
Let me say something clearly:
You are not obligated to keep chasing residency just because you went to med school. Quitting is not failure. Blind persistence isn’t bravery if the odds are brutal and the plan is vague.
But also: a failed Match and some gaps don’t automatically mean you’re done.
The hard part is figuring out which camp you’re in.
What “Multiple Gaps + Failed Match” Actually Signal to Programs
Programs aren’t sitting there thinking, “Wow, what a terrible person.” They’re thinking in risk language. You feel rejected; they see risk.
Here’s what your red flags translate to in their heads:
Multiple gaps after graduation
“Why the gaps? Burnout? Competence issue? Visa? Can they still function clinically? Are they rusty?”Failed Match (especially >1)
“Why didn’t anyone pick them? Bad interviews? Low scores? Weak letters? Unprofessionalism? Personality fit?”Older year of graduation (YOG)
“Is their knowledge outdated? Will they adapt to EMR? Are they going to be a remediation headache?”
They don’t have time to investigate every story. So they filter hard.
The unspoken rule:
The farther you are from graduation + the more times you’ve tried and failed + the fewer things you’ve done to actively fill those gaps = the more “radioactive” your app looks.
That sounds harsh. But you need the brutal version to decide if there’s still a path or if it’s time to pivot.
Step 1: Stop Asking “Should I Give Up?” and Ask Better Questions
“Should I give up?” is too vague. It keeps you in a spiral.
Ask these instead:
Is there objective evidence that my application has improved since my last failed Match?
Not “I want it more.” Things like:- New clinical experience with strong letters
- New USMLE/COMLEX pass/improvement
- Research, publications, or meaningful QI projects
- US clinical experience if you’re an IMG
Has anyone in my situation, recently, actually matched?
Not rumor. Real people: same YOG, similar scores, same number of attempts, similar citizenship/visa situation, similar specialty.Can I realistically fill my gaps over the next 12–18 months?
There’s “I’ll try to do observerships somewhere” and then there’s “I already emailed 200 hospitals, got 3 bites, and start in May.”What am I risking if I keep going?
Years? Money? Mental health? Relationships? Immigration status?If I walked away today, what would my life actually look like in 3 years?
Not just the fear version. The realistic version: job options, income, training in something else.
Those questions hurt. But they’re the ones that get you out of the vague fog.
Step 2: Do a Ruthless Audit of Your Application
You probably already know your weak spots, but let’s lay them out like a program director would.
| Area | Strong / Weak / Red Flag |
|---|---|
| Step/COMLEX scores | |
| Attempts/failures | |
| Year of graduation | |
| Number of Matches | |
| US clinical exp. | |
| Letters of rec. | |
| Gaps explained? |
Fill that in honestly. No optimism padding.
If multiple boxes are “Red Flag,” the question shifts from “Can I match?” to “Can I reduce enough of these flags in the next 1–2 years to give myself a real shot?”
Because here’s the uncomfortable truth:
If your app looks basically the same as last cycle, programs will treat you exactly the same. Or worse, because now you’re another year out.
That’s where so many repeat applicants get stuck—they reapply with:
- Same PS and CV with slightly different dates
- No new letters
- No new clinical work
- No major testing change
and pray for different results. That’s not perseverance. That’s magical thinking.
Step 3: Understand What’s Fixable and What’s Not
You don’t control everything. But not everything is doom either.
Things you can still improve
Recent clinical experience
Observerships, externships, research with some patient-facing work, scribe roles, maybe prelim/TY if you can swing it. You want recency (last 6–12 months) and strong letters that comment on your current performance.Narrative for your gaps
If you’ve had mental health struggles, family illness, financial disaster, Step fail—there’s a way to frame it that shows:- Insight
- Growth
- Stability now
“I disappeared and played video games for two years” is obviously harder to spin, but even then you can start building a new narrative from now.
Application strategy
Specialty choice, number of programs, community vs big-name academic, geographic flexibility, DO vs MD programs, prelim-only positions. Many people sabotage themselves by aiming too high or too narrowly with red flags.Personal branding (I hate the term, but it matters)
Your story has to hang together: This is who I was, what happened, what I did about it, and who I am clinically now.
Things you can’t change
- Scores already taken and passed
- Old failures on record
- Year of graduation
- Citizenship/visa category
You can work around those, but you don’t erase them.
If your whole “plan” relies on the universe forgetting your red flags, that’s not a plan.
Step 4: Harsh Reality – When It Might Be Time to Let Go
You don’t want sugarcoating, so here’s when I start thinking, “Continuing might be self-destructive”:
- You’re >7–10 years out from graduation with no consistent recent clinical experience and no path to get it.
- You’ve failed to Match 3+ times and your last cycle showed almost no interviews, despite:
- Applying broadly
- Targeting realistic programs/specialties
- Getting decent advising
- You can’t secure any meaningful clinical role (even unpaid observerships) despite months of trying.
- Your mental health is deteriorating with each cycle, and you’ve started losing function—can’t work, can’t sleep, all identity tied to Match.
- Financially, you’re at the point where another year of fees, exam registrations, travel, and opportunity cost is going to trap you.
Does this mean “you will never match”? No. There are unicorn stories. Someone knew someone; a random prelim year opened; an attending fought for them.
But as a strategy, “I’m praying to be a unicorn” is brutal.
Step 5: When There’s Still a Rational Path Forward
On the flip side, I’d seriously consider one more push if:
- You’re ≤5–7 years out from graduation
- You have at least one cycle with interviews, not just silence
- You can secure new, real clinical exposure in the next year (USCE if you’re IMG)
- You’re willing to pivot to less competitive specialties and less desirable locations
- You have a clear, specific improvement plan, not just “I’ll reapply and hope”
And you’re mentally able to say this to yourself:
“If I give it one more structured, all-in, no-excuses attempt and it still doesn’t work, I will pivot and not destroy myself over it.”
That boundary matters. Because this process will happily chew up 10 years of your life if you let it.
Step 6: Alternatives That Aren’t “Failure”
I know, your brain says: “If I don’t become a resident, I wasted my entire life and I’m a failure.”
That’s the perfectionist med-student brain talking. The one that only respects MD/DO + residency.
But out in the real world, people:
- Change careers in their 30s, 40s, 50s
- Use their med background in other fields
- Make decent money, have families, build actual lives
And nobody cares they didn’t match IM in 2019.
Real options people take:
- Non-residency clinical tracks in some countries (if immigration/personal life allows)
- Clinical research careers (coordinator → manager → maybe PhD or industry roles)
- Pharma / biotech / med device (medical affairs, safety, regulatory, MSL)
- Healthcare consulting / quality improvement / hospital admin
- Public health / MPH programs → NGOs, government roles
- Medical education (simulation centers, curriculum design, tutoring, prep companies)
Are these emotionally easy? No. You’ll probably grieve. You actually should grieve. It’s a loss of a specific future you imagined.
But it’s not the same as “I’ll be miserable forever.” That’s your anxiety telling stories again.
A Harsh but Weirdly Comforting Truth
There isn’t going to be a moment where someone “in charge” says:
“Yes, you should stop. You are officially not allowed to pursue residency anymore.”
No committee. No cutoff letter. No red stamp of “Done.”
You could keep applying at 45 if you pay the fees and meet basic requirements.
Which means the decision point is internal: How many more years of your 20s and 30s are you willing to trade on a possibility?
Not infinite. Not zero. An actual number.
“Two more cycles with real improvements, then I pivot.”
Or
“One more year to get strong USCE and letters, then one final all‑in cycle.”
You set the boundary. Or the process will never stop taking.
A Mini Framework to Decide (Not Perfect, But Better Than Vibes)
Look at this as a rough guide, not scripture.

| Category | Value |
|---|---|
| Years Since Grad | 7 |
| Number of Failed Matches | 3 |
| Recent Clinical Experience | 4 |
| Interview History | 5 |
| Ability to Improve Within 1 Year | 6 |
Think of each factor on a 1–10 scale (1 = very favorable, 10 = very unfavorable). If you’re stacking 7–10s across the board and nothing is moving, that’s your signal.
If you’re more mid-range and see clear ways to shift numbers downward (more recent clinical, better strategy, improved interviews), then there’s still rational space for another attempt.
What You Can Actually Do Today (Instead of Spiraling)
You’re probably doom-scrolling on Reddit and Student Doctor, looking for that one person with 3 failed Matches, 5-year gap, low Step, who magically matched Derm. To prove it’s “still possible.”
You don’t need “still possible.” You need “reasonably likely with a clear plan.”
Here’s one concrete thing to do today:
Write a one-page brutal summary of your situation
Year of graduation, all board scores (with fails), number of Match attempts, number of interviews each time, gaps (with dates), current activities.Send that to 2–3 real advisors
Not just friends. Options:- Another resident or fellow in your target specialty
- A program director or APD (if you know one even remotely)
- A professional advising service (yes, it costs; sometimes it’s worth a one-time consult)
- A faculty mentor from med school
Ask them directly:
- “If I improve X, Y, Z in the next 12–18 months, do you see a realistic path to residency?”
- “If not, where do you see me having the best chance of building a career with my background?”
You want people who aren’t emotionally tied to your dream. Who can say, “This is very unlikely” without worrying they’ll hurt your feelings.
It’ll sting. But at least you’ll be choosing your next step with data, not just fear or hope.

| Step | Description |
|---|---|
| Step 1 | Current Situation: Gaps + Failed Match |
| Step 2 | Explore non-residency careers |
| Step 3 | High risk of endless cycles and burnout |
| Step 4 | Plan 1 more structured cycle |
| Step 5 | Secure recent clinical experience |
| Step 6 | Revamp application + apply strategically |
| Step 7 | Start residency |
| Step 8 | Any realistic way to improve in 12-18 months? |
| Step 9 | Willing to set a hard limit on attempts? |
| Step 10 | Matched? |
FAQ (You’re Not the Only One Thinking These)
1. I’ve failed the Match twice with almost no interviews. Is a third try pointless?
Not automatically pointless—but if you apply a third time with basically the same profile, you’re very likely to get the same silence. A third try is only justifiable if you can clearly show: new recent clinical work, stronger letters, improved strategy (different specialty/program tiers), and ideally some evidence you can actually attract interviews (like feedback from someone who screens apps). If your app hasn’t changed meaningfully, a third try is usually emotional, not strategic.
2. How many years after graduation is “too old” to match?
There’s no hard line, but once you’re >5 years out, especially as an IMG, many programs just auto-screen you out. Some community programs and certain specialties are more flexible, but if you’re 8–10+ years out with no consistent recent clinical work, the odds drop sharply. Can people still match? Rarely, yes. Is it common enough to bank your entire life on without a stellar plan and strong connections? No.
3. Do multiple gaps automatically kill my chances?
No—but unexplained or unproductive gaps are lethal. A 1-year gap where you cared for a sick parent, then did 6 months of research and got a strong letter? Manageable. Three years of scattered part-time work with no clear clinical involvement or explanation? Much harder. What matters now is: what are you doing in the present and next 12 months to show you’re active, clinically engaged, and stable.
4. If I give up on residency, was med school a waste?
Emotionally it’ll feel like that for a while. Logically, no. You still have deep clinical knowledge, experience with complex systems, and a credibility most people don’t. Those translate into other roles—research, pharma, public health, consulting, informatics, education. The sunk cost fallacy is vicious here. You’re allowed to decide that protecting your future 30 years matters more than “getting full value” out of the last 8.
5. Should I switch to a less competitive specialty just to improve my odds?
Only if you can honestly see yourself doing that specialty for years. Yes, switching from something like Derm, Ortho, or EM to FM/IM/Psych can help. But if you secretly hate the alternative, you’re signing up for a different kind of misery. That said, if your dream specialty is already borderline impossible with your record, and you’d be okay in a more general field, then yes—strategic pivoting is smart, not weak.
6. What’s one immediate step I can take if I’m completely lost after a failed Match?
Today, not next week: write that one-page brutally honest summary of your situation and send it to at least two people who actually understand residency selection. Ask them for unfiltered feedback and what they would do in your shoes, given your exact stats. Then, based on that, commit to either: (1) designing a 12–18 month improvement plan with a final-attempt boundary, or (2) spending the next month seriously mapping non-residency career options. No more floating in maybe-land.
Open a blank document right now and start that one-page brutal summary of your path, scores, attempts, gaps, and current work. If seeing it all in one place makes you wince, that’s fine—at least you’ll finally be deciding your future with your eyes open instead of guessing in the dark.






















