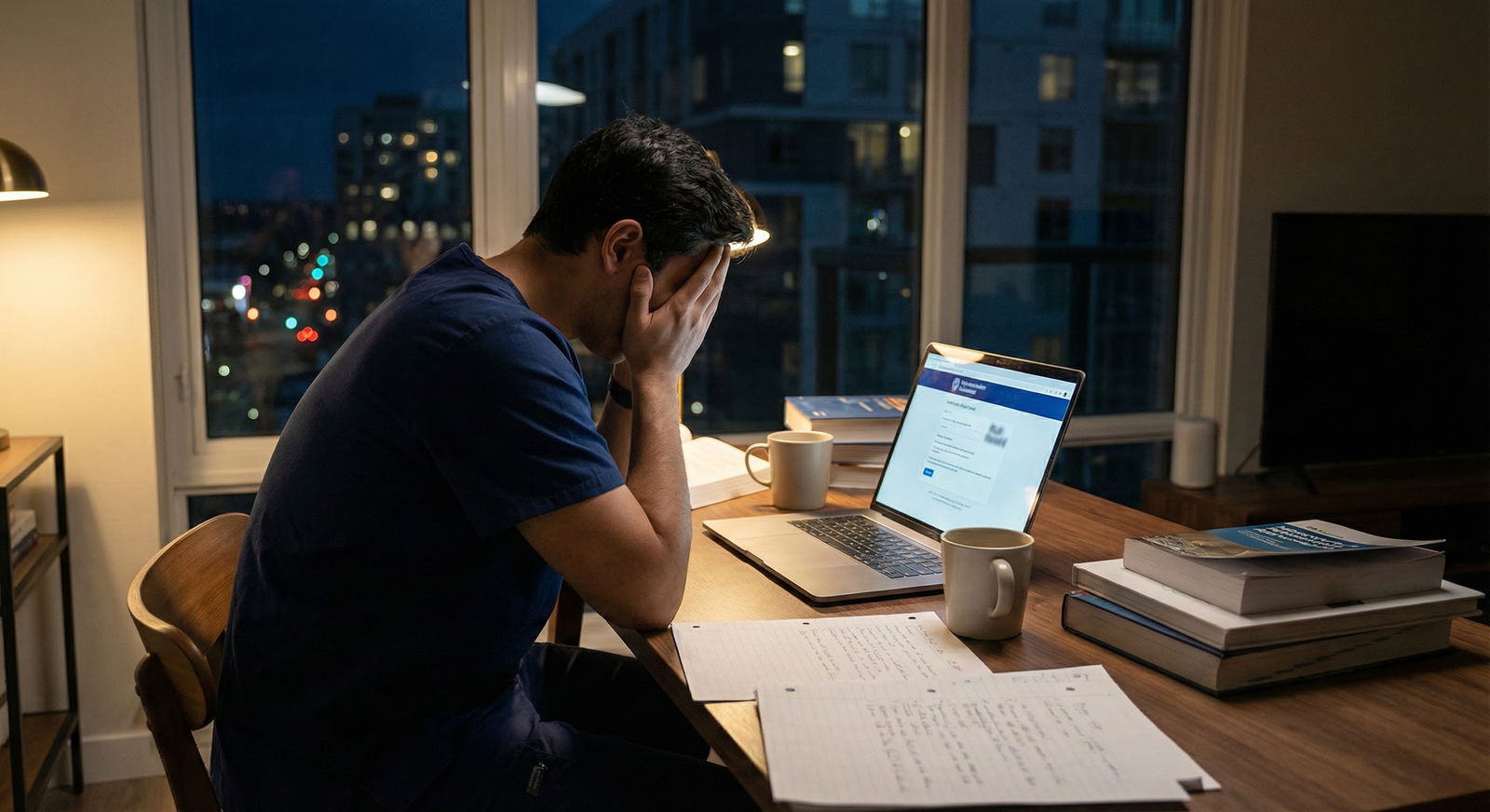
It’s late. Your ERAS portal is open. You’re staring at the “Education” and “Training Interruptions” section, cursor blinking over the months you stepped away from school. Your chest tightens just remembering it. The leave. The emails. The meetings. The evaluations that suddenly used words like “concern” and “support.”
Now you’re asking yourself the question you don’t really want answered:
“I took a mental health leave. Are residency program directors just going to slap ‘unreliable’ on my forehead and move on to the next applicant?”
You’re imagining them in some conference room scrolling through apps:
“She took a leave?”
“Yeah, too risky.”
“Pass.”
You’re wondering if your entire future is now just… permanently marked.
Let’s talk about what’s actually going on. Not the nightmare version in your head. The real version in PDs’ heads.
What PDs Actually Care About (Underneath the Judgement You’re Afraid Of)
Let me be blunt: program directors are not sitting there trying to sniff out who had a panic attack in M2.
They care about three things, more than anything:
- Will you show up and do the work?
- Will you be safe with patients?
- Will you be a headache for them (performance, professionalism, huge gaps, constant drama)?
That’s it. Everything else is noise.
A mental health leave plugs straight into your biggest fear: “They’ll assume I can’t show up, can’t handle stress, and will crumble.”
But that’s not automatically how it lands for them. What matters is:
- How long was the leave?
- Is there a clear resolution?
- How are you doing now?
- Did you finish strong after coming back?
If your record looks like:
- Took a leave → came back → passed boards → did fine or even better on rotations → got solid letters
…that’s a very different story than:
- Repeated leaves, failed multiple courses afterward, vague explanations, and a worried MSPE.
They’re not allergic to the word “leave.” They’re allergic to ongoing, unexplained risk.
Does a Mental Health Leave = Red Flag? Yes… and Also No.
You’re not imagining it: a leave can be a red flag. I’m not going to sugarcoat that.
But it’s not a giant red “X – never match” kind of flag. It’s more, “Okay, what happened here?” Some PDs barely blink. Others lean forward and start really reading.
Here’s how I’d categorize it:
| Situation | Typical PD Reaction |
|---|---|
| Short, clearly explained leave, strong performance after | Mild curiosity, usually not a dealbreaker |
| Longer leave, clear mental health reason, strong comeback | More questions, but can be neutral/ok if narrative is solid |
| Multiple leaves or combined with failures | Clear red flag, needs very strong explanation |
| Vague “personal reasons,” no context, spotty record | Big concern; often seen as risky |
The word “mental health” doesn’t automatically sink you. What scares PDs is uncertainty and unpredictability.
If you give them a coherent story:
- What happened
- What you did about it
- What’s different now
- Evidence that you’re stable
You shift from “unreliable mystery” to “human who went through something, took care of it, and is functioning.”
And yes, some PDs are still biased. Some are old-school, some are ignorant, some are quietly discriminatory even though they’d deny it. That’s real. But it’s not all of them, and it’s not permanent damnation.
The Worst-Case Scenario You Keep Imagining (and Why It’s Overblown)
You’re probably running some version of this in your head:
“I’ll submit ERAS, every PD will see the leave, assume I’m a ticking time bomb, and I’ll get 0 interviews. Maybe ever.”
Let’s blow that up with some reality.

| Category | Value |
|---|---|
| Clinical Performance & Letters | 35 |
| Board Scores | 30 |
| Interview Performance | 25 |
| Red Flags (including leaves) | 10 |
Is that exact percentage? No. But from what I’ve seen and heard from PDs:
- Your clinical performance and letters matter more than your leave.
- Your Step scores and overall trajectory matter more than your leave.
- Your interview—how you present, how stable you seem—matters more than your leave.
The leave is a context piece. It’s not the entire story. Unless you let it become the whole story.
What actually kills people’s cycles more often?
- Weak letters that say “meets expectations” and nothing else
- Failing Step 2 and not addressing it
- Terrible interviews where they come off defensive, vague, or in denial
- An MSPE full of quiet red-flag language: “required closer monitoring,” “needed multiple reminders,” “was frequently late.”
Your brain is zoomed in on the leave because it feels like a scarlet letter. PDs are zoomed out on the pattern.
How Much Detail Do I Have to Share About My Mental Health?
This is the part that makes your stomach twist: “Do I have to say depression? Anxiety? Hospitalization? Am I about to turn my personal crisis into ERAS content?”
Short answer: no, you don’t have to disclose diagnoses. You have to explain the impact on your training, and the resolution, not your DSM codes.
Think in layers:
- ERAS / MSPE: Very brief, factual mention if required.
- Personal statement (if you choose): Carefully chosen details only if it strengthens your story.
- Interview: Honest but boundaried.
A safe structure you can use:
- There was a health issue (you can say “health” or “mental health,” your choice).
- You recognized you were struggling and sought help.
- You took a leave in coordination with your school.
- You got effective treatment / support.
- You returned to school and have performed reliably since.
- You learned specific things that help you function better now.
You don’t need to share:
- Specific medications
- Exact diagnosis
- Hospitalizations (unless they directly shaped training interruptions in a way that’s already documented)
- Every low moment of your life
You are allowed to protect yourself. You are also allowed to be real.
How to Frame Your Leave So You Don’t Sound Like a Walking Risk
Here’s where a lot of people screw this up: they either overshare and trauma-dump, or they under-share and sound evasive.
You want “honest, concise, grown-up.”
Think like this:
“During my second year, I experienced a mental health episode related to a combination of personal and academic stress. In partnership with my school, I took a brief leave to get treatment and focus on recovery. I returned the following semester, completed my coursework on time, and since then I’ve consistently performed at a high level clinically. That experience pushed me to build sustainable coping strategies, a solid support system, and better boundaries around sleep and workload. I’m now in a much more stable place and proud of the growth that came from it.”
That’s the vibe.
Notice what it does:
- Names that something happened
- Frames it as responsible (“in partnership with my school”)
- Shows closure (“returned,” “since then…”)
- Points to function, not feelings (“completed coursework,” “performed at a high level”)
- Pulls one or two lessons into the present
If your leave was longer or more complicated, the same structure still works. You may just say “extended leave” and focus strongly on what the last year or two have looked like.

What PDs Really Think When They See “Mental Health Leave”
Let me translate some reactions I’ve heard behind closed doors.
When they see a clearly explained single leave with a strong comeback:
- “Okay, they had a rough patch. Looks like they handled it.”
- “They took care of it and came back stronger—that’s actually a good sign.”
- “We’re all human. As long as they’re stable now.”
When they see vague language, no explanation, and shaky performance:
- “What is going on here?”
- “Is this going to blow up at 2 a.m. on night float?”
- “Do I want to take this risk when I have 500 other apps?”
You want to make it very easy for them to land in the first category.
Also—and this is important—many PDs, attendings, and current residents have had their own mental health struggles. Burnout, depression, therapy, meds. They’re not immune. Some are quietly grateful you took care of yourself instead of falling apart in front of patients.
Does bias still exist? Yes.
Is there generational variation? Yes—older PDs can be more skeptical, younger ones often more open.
But is “mental health leave = unreliable forever” the dominant belief? No. That’s your worst-case brain talking.
Specialty Matters (Annoying but True)
You’re also probably wondering, “Does it matter that I’m applying to [insert specialty]?”
Yeah. A bit.

| Category | Value |
|---|---|
| Psychiatry | 90 |
| Family Med | 80 |
| Internal Med | 70 |
| General Surgery | 55 |
| Neurosurgery | 45 |
Higher number = more likely to be open to nuanced stories and less freaked out by mental health.
This is not exact science, but from what I’ve seen:
- Psych, FM, peds, and some IM programs tend to be more humane about this.
- Highly competitive, high-intensity surgical subspecialties can be more rigid and less forgiving, especially if the leave was recent or long.
Does that mean “don’t even try” if you want ortho or neurosurg? Not necessarily. But you need:
- Absolutely rock-solid recent performance
- Impeccable letters
- A very clean, confident narrative
And maybe a Plan B that doesn’t depend on all of them being perfect human beings.

How Much Will This Follow Me Once I Match?
Another thing you’re probably quietly spiraling about: “Is this going to be whispered about forever? Will attendings on day one already know I’m ‘the one who took a leave’?”
Usually? No.
Here’s reality:
- PDs are busy. By July 1, they care way more about how you’re doing now than your M2 meltdown.
- Most faculty have never read your full ERAS. They may not even know you took a leave unless it affected your graduation significantly.
- Residents definitely don’t know unless you tell them.
The people who might know your backstory:
- PD / APD
- Maybe a core faculty member or mentor
- Occasionally chief residents, especially if they’re involved in recruitment
What lives on is not “took a leave.” It’s “is this resident dependable?”
You can absolutely rewrite your reputation with how you show up every day once you’re there.
The label in your head—“unreliable forever”—is not a permanent sticker in theirs unless you keep proving it true.
What You Should Do Right Now About This Leave
You don’t need another vague pep talk. You need concrete moves.
1. Get clarity from your dean / advisor
Ask them directly:
- How is my leave described in my MSPE?
- Is there any concerning language?
- How do you recommend I explain this in ERAS and interviews?
If the MSPE makes you sound like a walking crisis, push (politely but firmly) for more neutral language.
2. Decide your disclosure level
You need a plan you won’t freeze on:
- One or two lines for ERAS (if required in the interruption section)
- A 2–3 sentence explanation for interviews if asked
- Optional: a brief mention in your personal statement only if it clearly strengthens your story, not just to confess.
Practice saying it out loud until it doesn’t make you choke. It’ll still be uncomfortable, but at least it’ll be coherent.
3. Lean hard on what came after the leave
You need to make it visually obvious on your application that you stabilized:
- Strong Step 2 (or at least not another red flag)
- Consistent clerkship performance
- Letters that say words like “reliable,” “mature,” “excellent follow-through,” “team player”
If you have a letter writer who knows about your leave and can honestly say “they came back and crushed it,” that’s gold.

You’re Not the Only One. You’re Just Convinced You Are.
I’ve lost track of how many people I’ve seen match after:
- A semester-long leave for major depression
- An inpatient psych stay
- A year off due to crippling anxiety and panic attacks
- Burnout so bad they almost quit medicine completely
The ones who did best had a few things in common:
- They didn’t treat their leave like a dirty secret but also didn’t overshare
- They stabilized for real—therapy, meds, boundaries, actual change, not just “white-knuckle and pretend I’m fine”
- They owned the story: “This is part of my journey, not the whole plot.”
You’re terrified PDs will see you as unreliable forever. Some might. A few. You’ll never meet them because they won’t invite you.
But a lot of them? They’ll see someone who went through hell, paused, got help, and came back. Honestly, that looks a lot more stable than the person who’s clearly falling apart but refuses to stop.
FAQ: Mental Health Leave and Residency (The Questions You’re Afraid to Ask)
1. Do I have to disclose that it was for mental health, or can I just say “medical leave”?
You’re not required to name your mental health diagnosis. You can say “medical leave” or “health-related leave.” If they ask more directly in an interview, you can say “It was primarily for mental health reasons” and still keep it high-level. The key is not sounding evasive. You’re protecting details, not pretending nothing happened.
2. Will programs see me as a liability for call, nights, or high-stress rotations?
Some will worry about that if your story is unclear or your recent performance looks shaky. If you show that you’ve handled tough rotations since—like ICU, surgery, nights—without incident, that concern shrinks. You want to be able to say, “Since returning, I completed [X, Y, Z] and did very well on them.” That’s what calms them down.
3. Should I talk about my leave in my personal statement?
Only if you can do it cleanly and briefly—and only if it clearly supports your narrative. If your entire PS becomes a therapy journal entry, it’ll backfire. One short paragraph is plenty: what happened in broad strokes, what you learned, and how it shaped the kind of resident you’ll be. If you can’t do that without spiraling into oversharing, skip it and address it verbally if asked.
4. What if a PD directly asks, “Are you going to need another leave?” in the interview?
You answer calmly and directly: “I’ve put structures in place—treatment, support, and better habits—that have helped me stay stable and high-functioning. Since returning, I haven’t needed any additional leave, and I’ve handled full clinical loads and high-intensity rotations. I don’t anticipate needing another leave, and I’m committed to seeking help early if I feel myself slipping.” You’re not promising you’ll never struggle again. You’re showing insight and responsibility.
5. Is it ever better to delay applying a year after a leave?
Sometimes, yes. If your leave was very recent, your performance since returning is minimal, or you’re still not stable, taking extra time can help you build a stronger, more convincing “I’m okay now” story. A full year of clean performance, research, or an MPH with strong work can do more for your application than rushing into a cycle where you look fragile. It sucks to wait, but it’s better than faceplanting into a match cycle you weren’t ready for.
Open your ERAS draft right now and find the spot where your leave will show up. Write a 2–3 sentence explanation using the structure you saw above—rough, ugly, whatever. Just get a version down. You can edit later. But stop letting the blank space and your imagination be the loudest voice in this story.






















