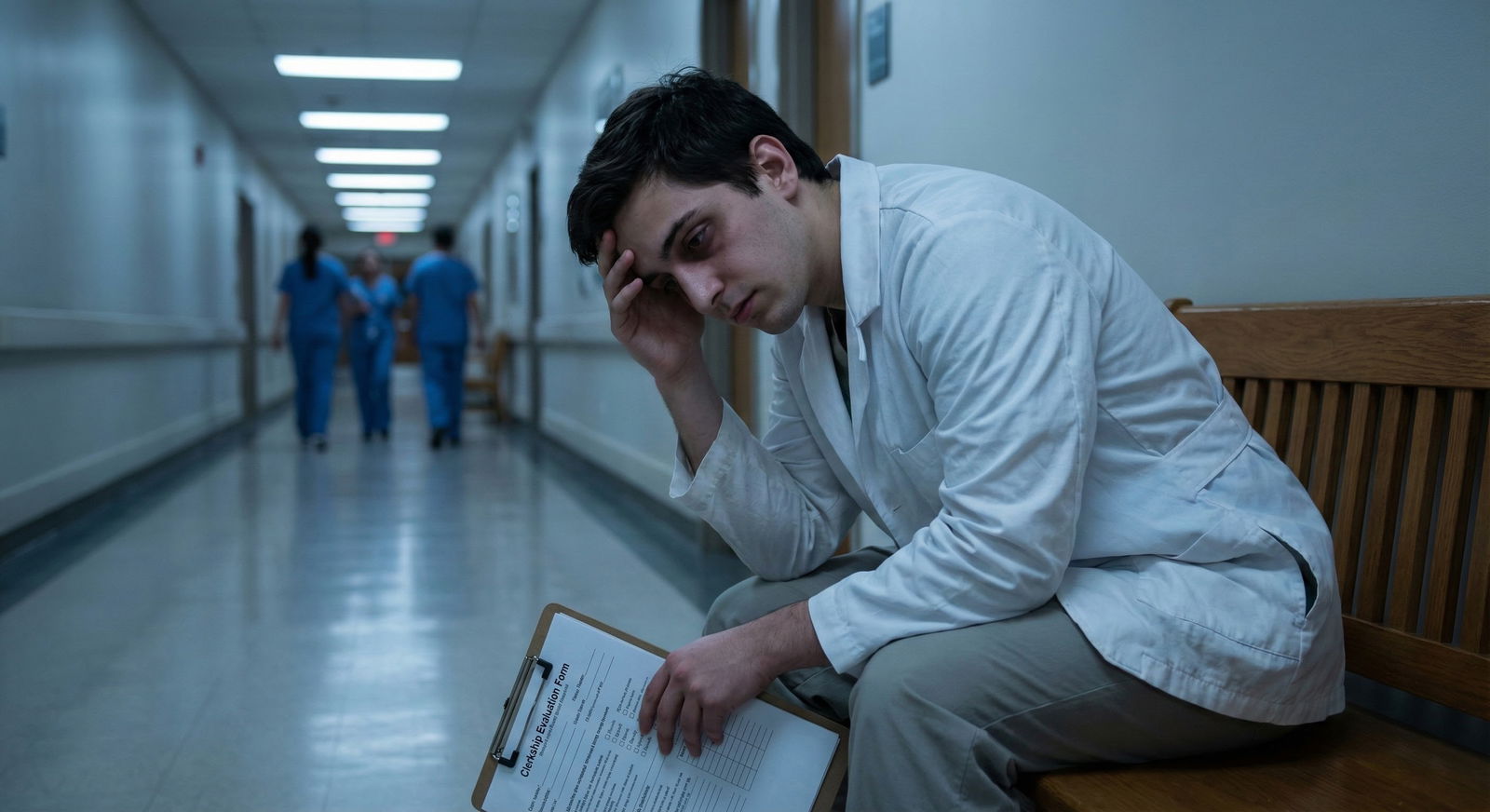
The biggest mistake students make after a remediated clerkship is pretending it never happened. Programs will see it. The question is whether it looks like a one-time stumble or the start of a pattern. Your rotation schedule is the evidence.
You are not just picking electives anymore. You are building your defense.
Below is how to structure the next 12–18 months chronologically so that, by the time your ERAS hits a PD’s inbox, the remediation reads as: “Handled it. Learned from it. Moved on.”
0–2 Weeks After You Learn You Must Remediate
At this point you should stop thinking about “How do I hide this?” and start thinking “How do I control the narrative?”
Week 0–1: Immediate triage
Get the facts in writing
- Exactly what will appear on your transcript and MSPE:
- “Remediated clerkship” vs “repeat required”
- Narrative language: “initially failed…” vs “required additional work…”
- Whether this delays graduation or only shifts rotation order.
- Whether your school labels it “concern for professionalism,” “clinical performance,” or both.
- Exactly what will appear on your transcript and MSPE:
Meet three people (separately)
- Clerkship director
- Ask: “What specifically led to the remediation?”
You want bullets, not vague impressions:- Missed notes
- Poor fund of knowledge
- Slow on the wards
- Documentation issues
- Feedback not implemented
- Ask if they would support you doing another rotation in that specialty later to demonstrate growth.
- Ask: “What specifically led to the remediation?”
- Dean of students / academic affairs
- Clarify: impact on:
- graduation date
- away rotations
- Step 2 timing
- eligibility for couples match / leaves
- Clarify: impact on:
- Trusted faculty mentor
- Preferably someone who knows how PDs think (former PD, APD, or core clerkship faculty).
- Show them your full likely timeline (Step dates, rotations left, career goals).
- Clerkship director
Decision point: keep or change intended specialty
- If the remediated clerkship is:
- In your intended field (e.g., internal medicine for someone aiming IM) and
- Due to clear performance/professionalism problems
→ you should at least consider pivoting if you were aiming at a very competitive specialty.
- If it is:
- In a different field (e.g., OB/GYN for a future psychiatrist), or
- Clearly a single-scenario mismatch (bad team, noted personal crisis)
→ you likely can stay the course, but you must build a strong recovery story.
- If the remediated clerkship is:
You do not need to decide your entire future this week. But you do need clarity on: What exactly went wrong, and how is it recorded?
Month 1–3: Stabilize, Remediate, and Rebuild Foundations
At this point you should be treating your remediation period as a controlled re-audition. Every day is data for future letters and your dean’s note.
During the remediation block
Daily / weekly behavior checklist:
- Show up early, not just “on time.”
- Volunteer for:
- Extra notes
- Follow-up calls
- Discharges
- Ask for mid-rotation feedback and write it down.
- Use a simple loop:
- Day 1: Ask attending, “One thing I can do better tomorrow?”
- Day 2: Tell them, “Yesterday you said X; today I did Y to adjust.”
- Track concrete improvements:
- “Initial H&P time: 75 mins → 45 mins by week 3”
- “Note rewrites: 3–4 → 0–1 per day”
- “Shelf practice: UWorld block scores from 45% → 70%”
You are collecting receipts to reference later in your personal statement and interviews.
Academic recovery plan (Months 1–3)
If the deficiency was knowledge-based:
- Set a minimum weekly question goal:
- 100–150 questions/week in that subject area (UWorld, AMBOSS, etc.).
- Simple schedule:
- Mon–Fri: 20–25 questions/day + 30–45 minutes review.
- Sat: 40–50 questions + content review.
- Sun: Light reading; consolidate “missed concept” notebook.
If it was professionalism / organization:
- Lock in:
- A task tracking system (Notion, paper planner, phone reminders—whatever you will actually use).
- A sign-out template and daily to-do list structure.
- Fixed habits: laying out clothes, commute buffer, backup alarms.
You are not “waiting for next year.” You are already in your repair phase.
3–6 Months Before ERAS Opens: Reordering Your Upcoming Rotations
This is where strategy matters most. At this point you should design your schedule so the 12 months after the remediation show:
- No new concerns.
- Clear upward trajectory.
- Strong performance in your target specialty early enough to secure letters.
Step 1: Map your remaining requirements
Sit down with your school’s scheduling system and literally list:
- Required core rotations left (if any).
- Sub-internships (“acting internships”).
- Electives at home.
- Time windows for away rotations.
- Research / lighter months.
- Vacation blocks.
Then overlay:
- Step 2 CK study window.
- ERAS open date (mid-June).
- MSPE release date (Oct 1).
- Likely letter request deadlines (July–September).
| Milestone | Typical Timing |
|---|---|
| Step 2 CK | Apr–Aug (before MSPE) |
| ERAS Opens | Mid-June |
| First ERAS Submission | Late June |
| MSPE Release | October 1 |
| Interview Season | Oct–Jan |
Your goal: front-load strong, letter-generating rotations before ERAS while keeping enough bandwidth for a solid Step 2 score to counterbalance the red flag.
Step 2: Key scheduling principles after a remediated clerkship
Put a strong Sub-I in your chosen field before August
- This is non-negotiable.
- It should be:
- In your chosen specialty.
- At your home institution (unless your home program is nonexistent or toxic).
- With faculty who are known to write detailed letters.
Avoid back-to-back high-burnout blocks before ERAS
- Example of a bad sequence (post-remediation):
- July: Sub-I (IM)
- August: ICU
- September: Surgical Sub-I
You will be exhausted, your Step 2 studying will suffer, and any small slip may look like “pattern of inconsistency.”
- Better:
- June: Ward month in intended field (lighter than Sub-I).
- July: Sub-I.
- August: Lighter elective + Step 2 studying.
- September: Away elective or another home elective.
- Example of a bad sequence (post-remediation):
Place the remediated field strategically
- If the remediated clerkship is in a field you are not pursuing:
- Do not schedule another full clerkship there immediately before ERAS.
- You can place a short elective later in the year to show “I can function fine here,” but do not crowd your pre-ERAS window with it.
- If it is in your intended field:
- You want a later repeat exposure (Sub-I or advanced elective) in that same specialty with a different team that can explicitly comment on your improvement.
- If the remediated clerkship is in a field you are not pursuing:
6–9 Months Before ERAS: Building the “Comeback” Rotation Sequence
At this point you should lock in a 3–4 rotation run that tells a clear story: “I am now performing at or above the level for my intended specialty.”
Ideal 4-rotation block (Feb–May for a typical ERAS cycle)
Assuming ERAS in June and MSPE in October.
Rotation 1: Solid core or elective in your intended field
- Goal: show consistent, reliable performance.
- Ask explicitly for informal feedback mid-rotation: “Do you see any major concerns that would worry a residency PD?”
- If the answer is yes, you must address that immediately.
Rotation 2: Sub-I in your intended field (home)
- This should be April–June for most.
- Target:
- Work like a reliable intern.
- Run a small list.
- Own communication with nurses and consultants.
- Get at least one strong letter from attending and ideally a supportive comment from the senior resident.
- Ask 7–10 days before end: “Based on my performance, would you feel comfortable writing a strong letter for residency?”
If there is any hesitation, find another writer.
Rotation 3: Lighter or complementary elective
- Good choices:
- Outpatient clinic in your specialty.
- Consult service with good teaching but manageable hours.
- Research month with some clinical exposure.
- Use this block to:
- Finish personal statement drafts.
- Nail Step 2 studying.
- Meet with mentors about your narrative.
- Good choices:
Rotation 4: Either an away rotation or another Sub-I / advanced elective
- If you have a remediated clerkship, an away can help but only if:
- You are already stable and consistently strong.
- You have fixed the issues that led to remediation.
- Do not use an away as your first test case after remediation. You do not want to struggle under a microscope at another institution.
- If you have a remediated clerkship, an away can help but only if:

| Category | Value |
|---|---|
| High-intensity clinical | 40 |
| Moderate clinical + Step 2 | 30 |
| Light elective + Applications | 20 |
| Personal time | 10 |
Specific Scenarios and How To Sequence Rotations
Let me be blunt: different combinations of red flags demand different levels of caution. A remediated clerkship paired with a low Step score is not the same as a single clerkship blip with strong boards.
Scenario 1: Remediated clerkship + borderline Step 1 (now P/F but noted problems, or old numeric score)
At this point you should prioritize a high Step 2 score and a clean recent clinical record.
- 6–9 months before ERAS:
- One strong core or elective to confirm improvement.
- Then 4–6 dedicated weeks for Step 2 (with a light elective or research).
- 3–6 months before ERAS:
- Sub-I in target field.
- Second strong elective with letter potential.
- Step 2:
- Ideally taken before your Sub-I so you can focus on pure clinical performance, or right after a clinically rich month when your knowledge is fresh.
Scenario 2: Remediated clerkship due to professionalism (lateness, documentation issues, communication)
Programs take these more seriously. Your schedule must give you many chances to demonstrate reliable, boringly consistent professionalism.
- Months 1–3 after remediation:
- Take at least one moderate-intensity core or elective where you can show:
- No lateness.
- No missed notes.
- No missed pages.
- Ask attendings to comment specifically in feedback on your reliability.
- Take at least one moderate-intensity core or elective where you can show:
- 3–6 months before ERAS:
- Sub-I on a team with a reputation for being strict but fair.
- Schedule a follow-up visit with your dean or advisor mid-year:
- Show them your evaluations.
- Make sure they are comfortable writing that the concerns are resolved in the MSPE.
Using Time After ERAS Submission (Aug–Jan) To Your Advantage
Many students mentally stop planning after September. You cannot afford that.
At this point (post-ERAS), your rotations serve two purposes:
- Generate late but valuable updates.
- Prevent any new problems from sabotaging your interview season.
September–December rotations
Strong choices:
- Another Sub-I or advanced elective in your chosen field
- Even if the letter will be “late,” you can:
- Ask for a short email update to PDs.
- Bring it up in interviews.
- Include it in post-interview communication.
- Even if the letter will be “late,” you can:
- Electives that broaden your competency
- For IM: ICU, cardiology, nephrology consult.
- For EM: anesthesia, MICU, trauma surgery.
- For psych: neurology, addictions, consult-liaison.
Rotations to avoid if possible:
- Brand new high-intensity field where you might struggle again.
- Multi-site, poorly structured electives with chaotic supervision where things can go sideways and evaluations get messy.

| Period | Event |
|---|---|
| Early Recovery - Month 1-2 | Remediation block + feedback |
| Early Recovery - Month 3-4 | Solid core/elective, rebuild foundation |
| Pre-ERAS - Month 5-6 | Sub-I in intended specialty |
| Pre-ERAS - Month 7 | Lighter elective + Step 2 study |
| Pre-ERAS - Month 8 | Away or advanced elective |
| ERAS & Interviews - Month 9 | ERAS submission |
| ERAS & Interviews - Month 10-13 | Interviews + strong electives |
How To Talk About Your Schedule and Remediation
Rotations alone do not tell the story. You will be asked:
- In your personal statement.
- In your dean’s letter.
- On interview day: “Tell me about this remediated clerkship.”
Your schedule must give you truthful talking points.
Build a clean narrative backed by your timeline
Structure:
Brief acknowledgment
- “During my third-year OB/GYN clerkship, I initially did not meet the expectations for clinical documentation and efficiency, which required a period of remediation.”
Insight + action
- “My evaluations highlighted that I struggled with managing competing tasks on busy inpatient teams. I began meeting weekly with my clerkship director, adopted a structured task system, and sought additional feedback on my notes.”
Evidence of change, tied to later rotations
- “On my subsequent internal medicine rotation and later my medicine Sub-I, I was consistently recognized for organized sign-outs and timely documentation, and I received strong evaluations that reflected this improvement.”
Your schedule makes #3 possible. Without that sequence of stronger rotations, your explanation sounds hollow.
Concrete Month-by-Month Sample Timelines
Let me give you two sample one-year timelines after a remediated clerkship. Adjust dates to your school’s calendar, but keep the structure.
Example A: IM applicant, remediated surgery, strong Step 2 focus
- January–February
- Finish remedial surgery block.
- Weekly feedback sessions. Document improvements.
- March
- Core internal medicine wards (not Sub-I yet).
- Goal: rock-solid performance; request feedback mid-rotation.
- April
- Dedicated Step 2 study + light outpatient elective (e.g., rheum clinic).
- May
- Take Step 2 early–mid May.
- Short reading elective or research for recovery.
- June
- IM Sub-I at home.
- Ask at least one attending and one senior resident for letters.
- July
- Cardiology or ICU elective (moderate intensity).
- Draft personal statement; meet mentor to review.
- August
- Lighter inpatient consult service; finalize ERAS.
- September
- Away IM elective (if advisors agree) or second home IM elective.
- Start interviews.
- October–January
- Mix of:
- Another advanced IM elective.
- Non-malignant electives with good teaching.
- Mix of:

| Category | Value |
|---|---|
| High-intensity wards | 12 |
| Sub-I | 4 |
| Light electives | 16 |
| Step 2 study | 6 |
Example B: Psych applicant, remediated internal medicine, professionalism concerns
- January–February
- Remediate internal medicine.
- Daily self-check on punctuality, communication, documentation.
- March
- Neurology core clerkship.
- Ask faculty to specifically comment on reliability.
- April
- Psychiatry core (if not done) or advanced psych elective.
- Identify potential psych letter writers.
- May
- Light psych outpatient elective + Step 2 focused study.
- June
- Take Step 2.
- Research month in psychiatry (good for another letter).
- July
- Psych Sub-I / Inpatient psych at home.
- Request letters from at least two attendings.
- August
- Addiction psych or CL psych elective.
- Finalize ERAS, personal statement directly addressing growth from remediation.
- September–December
- Mix of:
- Outpatient psych clinic.
- Neurology or primary care electives that show you function well in non-psych environments.
- Mix of:
Final 4–6 Weeks Before ERAS Submission
At this point you should already have:
- At least one outstanding evaluation post-remediation documenting improvement.
- A clear Sub-I in your intended specialty either completed or in progress with strong feedback.
- A Step 2 plan that will not crash into your heaviest rotations.
Checklist:
- Print or save all evaluations from the last 12 months.
- Confirm letter writers and deadlines.
- Meet with your dean or advisor:
- Review how your remediation and subsequent performance will be described in the MSPE.
- Make sure the language reflects resolution and not ongoing concern.
Key Takeaways
- A remediated clerkship is a red flag only if it looks like the start of a pattern. Use your next 12 months of rotations to build a clear, chronological story of recovery and strength in your chosen field.
- Schedule your Sub-I and strongest letter-generating rotations before ERAS, but avoid stacking multiple high-intensity blocks that could trigger new problems. Protect time for Step 2.
- Every rotation after remediation is part of your evidence file. Choose settings and sequences where you can reliably perform, get detailed feedback, and point to concrete growth when programs ask, “What happened, and what did you do about it?”






















