The Hidden Impact of Extended Medical School Duration on Your File
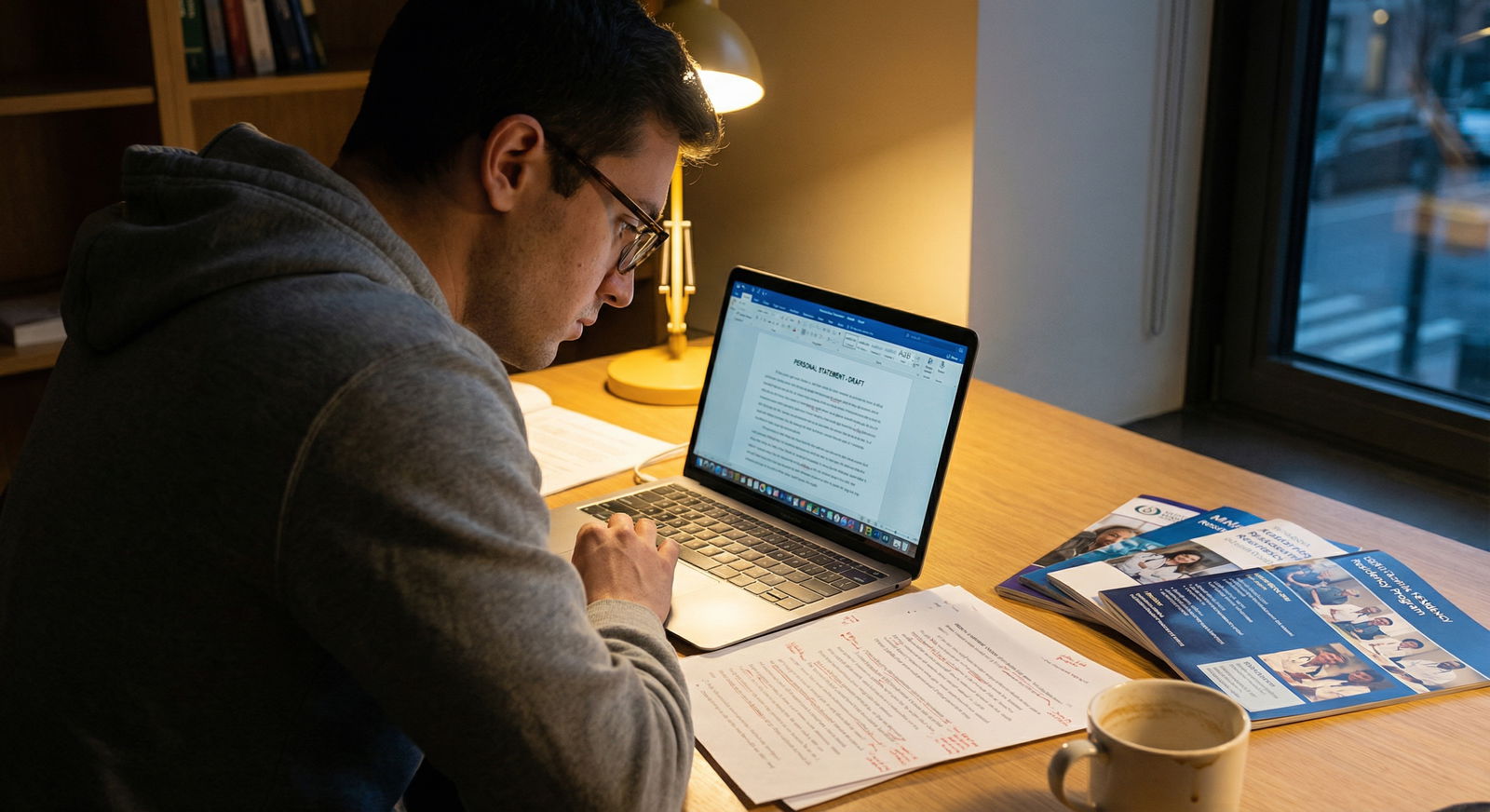
It’s January. You’re updating ERAS or pre-writing for next cycle, staring at that “Education” section and doing the mental math you hope nobody else is doing.
Matriculated: 2018.
Expected graduation: 2025.
Seven years. Maybe eight if things slip.
You can feel it: that line on your CV is louder than any LOR you have. You’re wondering how bad this actually looks. You’ve heard rumors. “More than 4 years is a red flag.” “Anything over 6 is unmatchable.” Your dean gave you some vague reassurance that “programs will understand.”
Let me tell you what really happens on the other side of the screen.
What Program Directors Actually See When They Open Your File
Here’s the part nobody tells you: the first thing many PDs and selection committee members check is not your personal statement, not your letters, not your Step scores. It’s the dates.
Medical school start date.
Medical school graduation date.
Any gaps in between.
I’ve watched this play out in selection meetings at multiple programs. The script is eerily similar.
“US MD. Step 1 pass, Step 2 243. Research, decent letters.”
…scrolls a bit…
“Wait, why is this a 7-year med school?”
The room pauses. Then one of three things happens:
- Someone shrugs: “LOA for family, research year, looks explained. Fine.”
- Someone raises a skeptical eyebrow: “Multiple leaves, some vague. Why?”
- Someone flat-out says: “Too messy. We have 600 more apps. Next.”
Extended duration itself is not an automatic death sentence. But it is a trigger. It forces a conversation. And the outcome of that conversation depends heavily on three things:
- The length of extension
- The reason (and how well you’ve framed it)
- The pattern (one clean, well-documented LOA vs serial issues and failures)
Let’s lay out the rough bands most PDs use mentally, even if they don’t say it out loud.

| Category | Value |
|---|---|
| 4 years | 70 |
| 5 years | 55 |
| 6 years | 35 |
| 7+ years | 15 |
That chart is not match-rate data; it’s roughly how comfortable programs feel continuing to review the file, based on the years alone. The longer you go, the more they demand a clear, compelling story.
The Truth About “How Many Years Is Too Many?”
Here’s the unofficial, rarely published reality for US MD/DO applicants:
| Total Duration | Common Interpretation | Risk Level |
|---|---|---|
| 4 years | Standard | Low |
| 5 years | Single LOA / research | Low-Moderate |
| 6 years | Significant LOA / issues | Moderate-High |
| 7+ years | Chronic problems / major disruption | High |
Notice I said “interpretation,” not fact. They don’t know your life. They’re pattern-matching.
Now, how they actually think about different reasons:
1. Pure Research or Funded Degree (MD/PhD, MPH, MBA, etc.)
If your extra time is clearly structured and documented—“2019–2021: NIH research scholar; returned to M3 2021”—most academic programs don’t blink. They like it, especially in IM, neuro, rad onc, radiation, pathology, some surgical subs.
What raises flags is not time for research itself, but sloppy timelines:
- “6 years in med school, 3 ‘research experiences,’ none clearly full-time, no degree earned.”
- “Took ‘time off for research’ but no abstracts, no posters, no letters from mentors.”
Result: PDs assume “unstructured floundering” instead of “focused scholarship.”
2. LOA for Health, Family, Burnout, or Personal Crisis
This one is delicate, and this is where the public messaging and the private thinking diverge.
Public messaging from schools:
“Take the time you need, programs will understand, wellness is important.”
Private reality in selection committee:
“We need to know if this is likely to recur under residency stress.”
When they see:
- LOA for a single, time-limited issue, with clean performance before and after → many programs are okay with this, especially in primary care oriented specialties.
- Multiple LOAs, vague language, and an uneven transcript → most competitive departments quietly move on.
They’re not heartless. They’re risk averse. Residency is already a liability minefield. You represent months of onboarding, salary, and service coverage. They’re asking one brutal question: “If we invest in this person, will they be consistently present and safe with patients?”
3. Extended Duration from Remediation / Failures
This is the hardest to recover from, and I’ve seen it from both sides.
- Failed multiple preclinical courses, repeated M1 or M2.
- Step 1 failure, then a long delay before retake.
- Repeat clerkships for professionalism or performance.
If your extension is tied to a trail of failures with no sustained, clean recovery period, programs read it as: “Chronic difficulty under pressure.” They worry the pattern will repeat with board prep, busy rotations, or licensing exams.
I’ve seen strong, likeable applicants with 6+ years and multiple failures get screened out at very reasonable community programs. Not because the PD disliked them. Because the committee literally had 50 safer choices with no remediation history.
4. “Life Happened” With No Paper Trail
This is the worst category: messy time with no structure.
Vague notes like “personal leave,” “time for reflection,” “travel,” “time to care for a friend” without any consistent narrative or documentation in your MSPE. PDs hate ambiguity. Ambiguity makes them imagine worst-case scenarios: substance issues, unprofessional conduct, legal problems.
You’re better off with a clear, appropriately framed explanation than a foggy mystery.
How Committees Actually Discuss Your Extended Timeline
Let me recreate a real conversation I’ve heard 100 times, modified only enough to protect identities.
“Next: US MD, 234 on Step 2, decent clerkship comments, some research.”
Scrolling.
“Hold on, started med school 2016, graduating 2024. That’s eight years. What happened?”
“Oh, MSPE shows LOA 2018–2020 for personal reasons, then another LOA 2021–2022 for academic remediation and Step 1 failure.”
“Any language about insight, growth, or being ready for residency?”
“Dean’s summary kind of waffles. Says ‘has made progress’ and ‘continues to develop study strategies.’”
[Long pause.]
Then somebody says the quiet part out loud:
“Look, we have 900 apps. Are you going to roll the dice on this one when there are 100 clean 4-year files with similar scores?”
That’s the reality. You are not being compared in isolation. You are always contrasted against “safer” files.
On the other hand, I’ve seen the opposite:
“US DO, 6-year med school. Why the gap?”
“Two-year NIH fellowship, 7 pubs, strong letter from a big-name PI, then honors in M3–M4.”
“Oh. Okay, bring them to interview.”
The extra years are not the problem. The story those years tell is.
Specialty-Specific Tolerance for Extended Duration
Not all specialties treat this the same way. Some are quietly more forgiving, some are shockingly unforgiving.
| Specialty | General Tolerance | Reality Behind Closed Doors |
|---|---|---|
| Family Med | High | Will look closely, but flexible if explained |
| Psychiatry | Moderate-High | Accepting of mental health LOAs if well-managed |
| Internal Med | Moderate | Academic IM more picky than community |
| Pediatrics | Moderate | Looks for stability and empathy narrative |
| General Surgery | Low | Multiple LOAs often fatal unless pure research |
| Ortho, ENT, Plastics, Derm | Very Low | Time = risk = usually no |
If you’re applying to highly competitive surgical fields with more than 5 years in med school and any academic red flags, the bar is brutally high. You’ll need near-perfect everything else and a compelling, airtight explanation.
For FM, IM (community), psych, peds—there’s more willingness to hear a story of struggle, recovery, and growth. But even there, extended duration plus multiple failures plus vague explanations? That gets quietly filtered out.
The MSPE and How It Can Quietly Save or Sink You
You’re obsessing over your personal statement and Step scores. PDs are obsessing over your MSPE timeline and “adverse academic events” section.
Here’s what they look for with extended duration:
- Are the leaves clearly dated and labeled? (e.g., “LOA 2019–2020 for health reasons.”)
- Is there commentary on performance after return? (“Returned to full-time curriculum and performed at or above class average.”)
- Does the dean endorse your readiness for residency in strong, unambiguous language?
Pay attention to that last one. Programs read hesitant language like tea leaves.
Strong:
“Student X is fully prepared for the challenges of residency and has demonstrated sustained academic and professional success upon returning from leave.”
Weak:
“Student X has made progress in addressing prior challenges and will benefit from close mentorship during residency.”
We all know what “will benefit from close mentorship” means. It means: “handle with care.”
If you have extended duration, you should be meeting with your dean/senior advisor well before MSPE season to make sure:
- The facts are accurate
- The story is consistent across documents
- The language reflects your real recovery, not just your timeline
Do not leave this to chance. I’ve watched students get hurt by a bland, non-defensive MSPE that did not match the strength of their actual comeback.
How to Frame Your Story Without Oversharing or Sounding Dangerous
Programs want three things from your explanation:
- Clarity (what actually happened, in broad strokes)
- Evidence of insight and growth
- Reassurance that it won’t derail residency
They do not want:
- Trauma dumps
- Graphic personal details
- Overly emotional narratives with no concrete evidence of stabilization
- Blame-shifting (“My school screwed me,” “Administration was unfair”)
Here’s the internal rubric PDs use, even if they don’t admit it:

| Category | Value |
|---|---|
| Clear & concise | 85 |
| Vague | 40 |
| Overly detailed | 30 |
| Blaming | 15 |
You want to be in the “clear & concise” category.
For example, let’s say you had a major depressive episode that required hospitalization and prolonged treatment, extending your med school by 1.5 years.
Bad version (seen in real applications):
“I struggled with serious mental health challenges that nearly cost me everything. I hit rock bottom and felt completely lost. I took time off because I could not function…”
That makes committees nervous. They picture you falling apart on night float.
Better version (and yes, this is the level of detail that actually works):
“During my second year, I experienced a significant mental health condition that required a leave of absence and structured treatment. With support from my care team and school, I returned to the curriculum, passed all subsequent coursework and clerkships on schedule, and have remained stable under ongoing care. This experience reshaped how I approach wellness, boundaries, and supporting colleagues who struggle silently.”
Then your MSPE backs this up with:
“Student X returned from LOA and completed M2–M4 without any further academic or professionalism concerns.”
Now the PD can tell themselves a story:
Yes, there was risk. It appears well-managed. There is a clear before/after. They’ve been stable under conditions similar to residency.
That’s the bar.
What You Need in Place If Your Med School Took 6+ Years
If you’re already at 6 or 7+ years, you cannot go back and fix the timeline. But you can change how it lands.
Here’s what I look for in an extended-duration file that makes me say “Okay, we can interview this person” instead of “Too risky”:
At least 18–24 months of clean, consistent performance
No failures, no professionalism incidents, no new leaves. You need a stretch of normal.A Step 2 score that shows you can handle medical knowledge
If you had prior failures, a solid Step 2 (for many fields, >230 for MD, >220 for DO; higher for competitive specialties) helps calm people down.Strong, specific letters that mention reliability
Not just “hardworking.” Things like:
“Never missed a shift.”
“Consistently calm under pressure.”
“One of the most dependable students I’ve worked with.”A clean, consistent narrative across documents
Your personal statement, ERAS experiences, MSPE, and interviews should all tell the same story. If details shift, committees start doubting your honesty.A specialty choice that matches your risk profile
Applying ortho with 7 years, multiple LOAs, and Step 2 barely passing is masochism. Applying FM/IM/psych with a solid recovery story is realistic.
What Actually Helps vs What’s Just Noise
People waste energy on the wrong fixes. Here’s the blunt version.
Things that actually move the needle for extended-duration applicants:
- A rock-solid final 1–2 years of med school
- Step 2 performance significantly better than your weakest points
- Deans and letter writers who explicitly “vouch” for your readiness
- Applying broadly and realistically, with a smart mix of academic and community programs
- Being prepared to talk calmly and briefly about your extra years in every interview
Things that do not magically erase the red flag:
- A dramatic personal statement hoping to “inspire” programs
- Vague “growth mindset” language with no concrete performance proof
- A scattershot application to 80 programs in ultra-competitive specialties
- Pretending it never happened and hoping nobody asks (they will)
How You Should Talk About It on Interview Day
You will get this question. Directly or indirectly.
“Can you walk me through your medical school timeline?”
“I noticed you took some time away—what would you like me to know about that?”
“I see your training extended beyond four years; how has that shaped you?”
You need a 60–90 second answer. Calm, matter-of-fact, rehearsed but not robotic. Something like:
“Sure. I started medical school in 2017. During my second year, I experienced [brief category: a medical issue / a family crisis / a mental health condition] that required a leave of absence. I worked with my physicians and the school to address it, and returned to the curriculum in 2020. Since then, I’ve completed all coursework and clerkships on schedule, passed Step 2, and really focused on building sustainable habits for residency. It was a hard period, but it’s changed how I think about resilience and asking for help early. I’m happy to answer anything specific that would help you understand where I am now.”
Then stop. Let them ask if they want more. Most won’t.
If you had academic failures:
“I struggled early in med school and failed two preclinical courses. I didn’t yet have the right study strategies or support in place. I remediated those classes, worked closely with our learning specialists, and since then I’ve passed all remaining courses and clerkships on first attempt, and did well on Step 2. That experience changed how I learn and how I approach struggling teammates. I feel prepared for the volume and pace of residency now.”
They’re listening for ownership, stability, and how recent the problems are. They’re not trying to punish you for your past. They’re trying not to get burned in the future.
What Actually Happens If You Try to “Hide” Things
Students sometimes ask, “What if I just don’t bring it up?”
You can’t. ERAS has the dates. The MSPE has the leaves. PDs know how to read between the lines. If you dodge the topic, you look dishonest. Dishonesty is a bigger red flag than an LOA.
I have watched committees give grace to someone with:
- 7-year med school
- A mental health LOA
- A Step 1 failure
…because that person was transparent, stable now, and had a clean last 2 years.
I’ve also watched committees blacklist someone who tried to minimize or fudge the story. Residents talk. Faculty talk. If there’s a major discrepancy between what you say and what your dean wrote, that gets around.
Own it once, cleanly. Then move on to everything that makes you strong.
FAQ
1. Is a 5-year medical school automatically a red flag?
No. A single extra year—especially for research, a structured degree, or a clearly explained life event—does not automatically hurt you. Many PDs barely flinch at a 5-year timeline if your performance before and after is solid and the reason is clear. It becomes a problem when the fifth year is unstructured, undocumented, or paired with multiple academic issues.
2. How long do I need to show “clean performance” after a leave or failure?
Aim for at least 18–24 months of stable, successful performance—no new leaves, no failures, no professionalism issues. That usually means your full core clinical year and into sub-Is. Committees want to see that you’ve already handled something residency-like in intensity without falling apart again.
3. Should I disclose mental health details specifically, or keep it general?
Keep it general. You don’t need diagnoses, hospital names, or specifics. A brief phrase like “a significant mental health condition that required a leave and treatment” is enough. The key is to pair it with evidence of stability: returned to full-time curriculum, passed everything on first attempt, doing well for the last couple of years. Too much detail can make programs nervous; too little makes them suspicious. Controlled, concise transparency is the sweet spot.
4. Can a strong Step 2 score “erase” a long med school duration?
It helps, but it doesn’t erase. A strong Step 2 (especially after earlier weaknesses) tells programs you can handle the medical knowledge under pressure. That can push some PDs from “no” to “maybe.” But if your timeline is packed with multiple LOAs and failures and your MSPE language is weak, Step 2 alone won’t save you—especially in competitive specialties.
5. If I’m at 6–7+ years, should I give up on matching?
Not automatically. You should give up on fantasy matches—ultra-competitive surgical subspecialties with spotless applicant pools. But many people with extended timelines match every year, usually into FM, IM (especially community), psych, or peds. The key is: realistic specialty choice, honest but tight explanation, a demonstrably stable recent track record, strong letters, and a broad, strategic application list.
Years from now, you won’t remember every anxious refresh of your inbox or every late-night spiral about your extra year (or three). What will stick with you is whether you faced your story head-on, told it cleanly, and backed it up with who you became afterward. That part’s still in your hands.






















