
As an international medical graduate (IMG) pursuing Addiction Medicine, the questions you ask programs are as important as the answers you give. Thoughtful, targeted questions not only help you evaluate fit and training quality—they also demonstrate insight, maturity, and true interest in the specialty.
This IMG residency guide (applicable for both fellowship and residency-style addiction medicine programs) will walk you through what to ask, who to ask, and how to use the answers to shape your rank list.
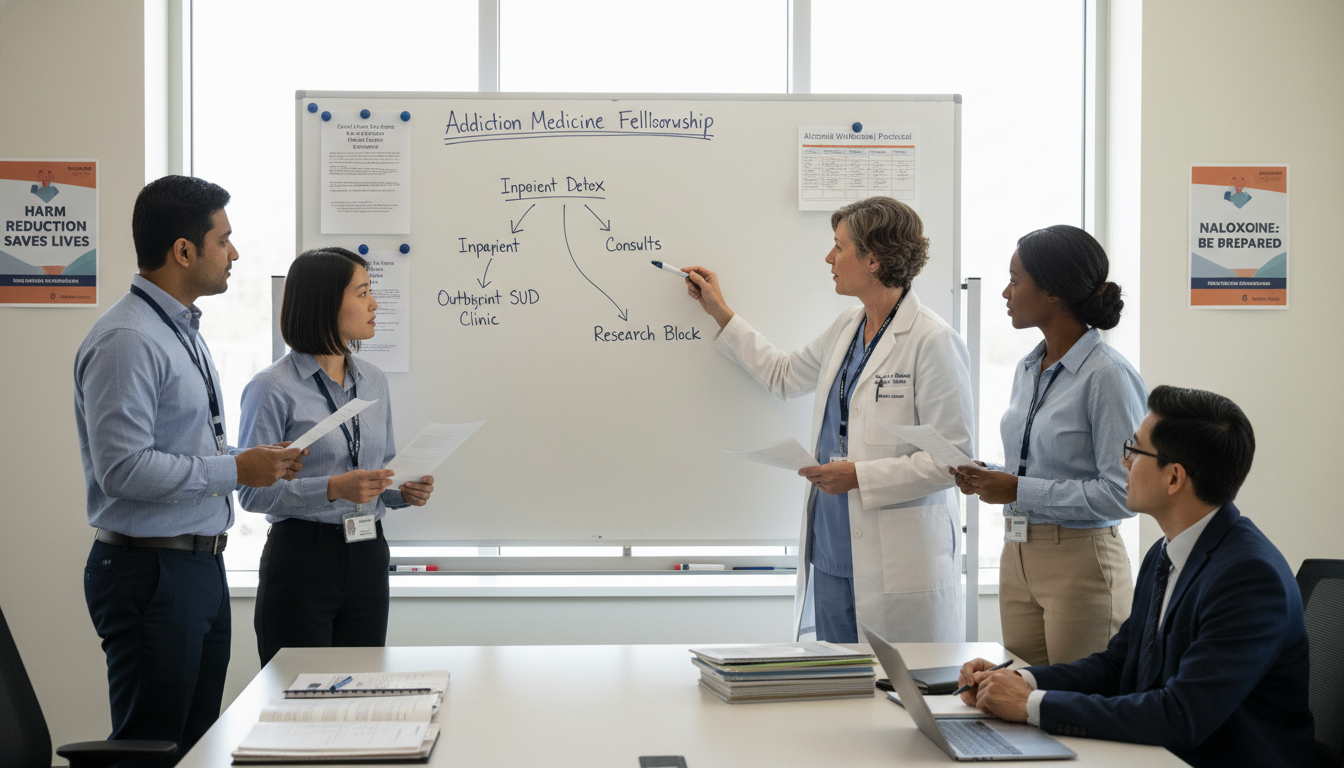
Understanding the Landscape: Addiction Medicine Training for IMGs
Before planning your questions, you need a clear picture of what Addiction Medicine training looks like for an international medical graduate.
Many Addiction Medicine positions in North America are structured as:
- Addiction Medicine fellowship after:
- Internal Medicine, Family Medicine, Psychiatry, or other primary specialty
- Addiction Psychiatry fellowship (psychiatry-based)
- Transitional or combined training (e.g., internal medicine with strong substance abuse training focus, or psychiatry programs with integrated addiction tracks)
As an IMG, your concerns may include:
- Visa sponsorship (J-1, H-1B)
- Board eligibility (ABPM/ABPN, or equivalent)
- Previous clinical experience outside the U.S./Canada
- Transition to U.S. healthcare systems
- Comfort with substance use disorders (SUDs), stigma, and complex psychosocial contexts
Your questions should be tailored to clarify:
- Training quality – Will you truly become an expert in addiction diagnosis and treatment?
- IMG support – Do they understand your unique needs as an international medical graduate?
- Career outcomes – Do graduates obtain good positions in academic, community, or global addiction medicine practice?
- Program culture – Is it supportive, inclusive, and safe for you to train in?
Strategy: How to Approach Questions During Interviews
You will have multiple opportunities to ask questions:
- Formal interviews with:
- Program Director (PD)
- Associate Program Director (APD)
- Faculty
- Resident/fellow meetings (often without faculty present)
- Program coordinator / GME office
- Virtual open houses, information sessions, or second looks
General Principles for Asking Strong Questions
- Be specific, not generic. “Tell me about your program” sounds unprepared. Instead: “How does your program ensure fellows gain competency in managing co-occurring psychiatric and substance use disorders?”
- Show you did your homework. Reference something from their website or brochure.
- Prioritize depth over quantity. A few well-framed questions are better than a long list you rush through.
- Avoid questions easily answered online. For example, basic salary, start dates, or location details—unless you need clarification.
- Adapt your questions to the person. Save visa, contract, and policy questions for program leadership or GME; ask trainees about day-to-day life and culture.
Below, you’ll find categorized interview questions for them—with explanations and examples tailored for an IMG in Addiction Medicine.
Core Clinical Training: Questions to Ask About Curriculum and Substance Abuse Training
Your primary goal is to gain robust, evidence-based substance abuse training that prepares you to treat complex patients. These questions help you assess how strong the core Addiction Medicine experience is.
Questions for the Program Director or Faculty
“Can you walk me through the structure of the Addiction Medicine curriculum over the year?”
- What you’re looking for:
- Balanced exposure to inpatient consults, outpatient treatment, community programs
- Time allocated to didactics, supervision, research, scholarly activities
- What you’re looking for:
“How much supervised experience will I have in prescribing medications for opioid, alcohol, and tobacco use disorders (e.g., buprenorphine, methadone, naltrexone, varenicline)?”
- Why it matters:
- You need hands-on experience with pharmacotherapy for SUDs
- Ask if you can gain DEA X-waiver–related competencies (or equivalent, depending on country and regulatory changes)
- Why it matters:
“What are the major clinical sites, and how do the patient populations differ between them?”
- Look for:
- Variety: academic hospital, community clinics, methadone programs, residential rehab, ED consults, primary care integration, possibly correctional settings
- Exposure to diverse socioeconomic and cultural backgrounds
- Look for:
“How is co-occurring psychiatric illness integrated into the training?”
- Addiction rarely exists in isolation—programs should teach:
- Assessment and management of depression, anxiety, psychosis, PTSD in SUD populations
- Collaboration with psychiatry, psychology, social work
- Addiction rarely exists in isolation—programs should teach:
“What opportunities are there to work with specific populations—pregnant women, adolescents, people experiencing homelessness, or patients with HIV/hepatitis C?”
- This reveals the breadth of training and possible future niche interests.
“How is the balance between inpatient consults and outpatient longitudinal care?”
- A strong Addiction Medicine fellowship typically includes:
- Acute stabilization and withdrawal management
- Longitudinal follow-up to understand chronic disease management and recovery trajectories
- A strong Addiction Medicine fellowship typically includes:
“Do fellows receive formal training in behavioral interventions such as motivational interviewing, contingency management, or cognitive behavioral strategies?”
- Addiction Medicine is not only about prescribing; structured behavioral training is vital.
“How are fellows trained in harm reduction approaches, such as syringe services, overdose prevention, and naloxone distribution?”
- Modern, patient-centered programs should embrace harm reduction and community-based strategies.
Questions About Call, Workload, and Supervision
“What does a typical week look like for a fellow in terms of clinical hours, call responsibilities, and didactics?”
- Clarify:
- Number of clinical sessions
- Night or weekend call frequency
- Time protected for conferences and teaching
- Clarify:
“How is supervision structured during high-acuity scenarios, such as severe withdrawal, intoxication with agitation, or complicated overdose cases?”
- This is especially important for IMGs adjusting to new practice environments.
- Programs should describe clear backup and escalation pathways.
- “How does your program monitor and prevent burnout among fellows, especially given the emotional intensity of addiction work?”
- Look for:
- Wellness resources
- Reasonable duty hours
- Debriefing after traumatic cases or patient deaths
IMG-Specific Questions: Visas, Support, and Integration
As an international medical graduate, you must directly address your unique situation—even if it feels uncomfortable. Programs are used to this; your clarity demonstrates professionalism.
Visa, Licensing, and Credentialing
Ask these primarily to the Program Director or Program Coordinator, and sometimes the GME office.
“What types of visas do you sponsor for international medical graduates in this program (J-1, H-1B, other)?”
- Clarify:
- Whether H-1B is possible (often requires successful USMLE Step 3 and institutional policy)
- Any history or constraints around visa changes
- Clarify:
“How familiar is your GME office with visa processing and support for IMGs?”
- A robust IMG-friendly institution will:
- Have a dedicated international office or immigration specialist
- Provide clear timelines and help navigating the process
- A robust IMG-friendly institution will:
“Are there any licensing or board certification issues specific to international medical graduates I should be aware of for Addiction Medicine here?”
- You want:
- Assurance about eligibility for ABPM/ABPN or local certifying bodies
- Clear path to independent practice after training
- You want:
“Do IMGs ever face delays in onboarding due to credentialing or verification of international training, and how does the program manage that?”
- This reveals:
- Program’s experience with foreign medical schools
- Their flexibility and communication around potential delays
- This reveals:
Clinical and Cultural Transition Support
“What kind of orientation or support do you provide to fellows who are new to the U.S. or Canadian healthcare systems?”
- Strong programs may offer:
- EMR training
- Systems navigation
- Policies on documentation, billing, confidentiality, and mandatory reporting
- Strong programs may offer:
“Have you had previous international medical graduate fellows in Addiction Medicine, and what has helped them succeed here?”
- Ask for:
- Specific examples of support
- Any mentoring or pairing with senior IMGs
- Ask for:
“How does your program address communication skills and patient interaction styles for trainees who trained outside the U.S.?”
- They might mention:
- Communication workshops
- Direct observation with feedback
- Support for accent and language adaptation, if needed
- They might mention:
“What support exists if there are challenges related to cultural differences, bias, or discrimination?”
- You’re gauging:
- Institutional commitment to diversity, equity, and inclusion
- Policies and safe reporting structures
- You’re gauging:
Questions to Ask Residents and Fellows: Culture, Fit, and Day-to-Day Reality
Trainees will give you the most candid picture of what life in the program is truly like. Prepare separate questions to ask residency or fellowship trainees compared to what you ask leadership.
Work Environment and Team Dynamics
“How would you describe the culture of this program in three words?”
- Then ask for examples to support those words.
“Do you feel comfortable asking for help when a case is complex or emotionally draining?”
- You’re assessing:
- Approachability of attendings
- Psychological safety
- You’re assessing:
“How does the team respond when someone makes a mistake or is struggling?”
- Strong programs:
- Focus on learning and systems improvement, not blame
- Have formal and informal support channels
- Strong programs:
“Can you describe the relationship between Addiction Medicine fellows and other departments such as Psychiatry, Internal Medicine, Emergency Medicine, and Primary Care?”
- Collaboration is key in SUD treatment.
- Listen for:
- Respectful interdisciplinary relations
- Shared decision-making
Realistic Expectations and Workload
“What does an average clinical workload look like, and does it feel manageable?”
- Ask for:
- Typical number of consults or patient visits per day
- Time for documentation and learning
- Ask for:
“How does the program respond if the workload becomes overwhelming—for example, in surges of overdose cases or high inpatient volumes?”
- Look for:
- Backup systems
- Adjustments to schedules or staffing
- Look for:
“Are there rotations or sites that most fellows find particularly challenging, and how do you get through them?”
- This reveals:
- Pain points of the program
- Practical coping strategies and program responsiveness
- This reveals:
Support for IMGs and Personal Life
“As an IMG (if they are one), what has your experience been here? What support did you wish you had earlier?”
- Target this to international trainees when possible.
“How easy is it to establish a life outside the hospital—housing, transportation, community, cultural or religious groups?”
- Particularly important if you’re moving countries and have no local network.
“Do you feel the program leadership is receptive to feedback from fellows? Can you give an example of a change made because of trainee input?”
- This helps you judge how responsive and progressive the program is.

Career Development, Research, and Long-Term Goals
Addiction Medicine is a growing field with opportunities in academia, public health, integrated primary care, correctional health, and global health. As an IMG, you should be explicit about your long-term goals and see whether the program can support them.
Questions on Career Preparation
“What types of positions do graduates from your program typically obtain after training?”
- Ask for:
- Academic vs. community distribution
- Addiction-only vs. combined practices
- Geographic spread, including if any return to their home countries
- Ask for:
“Do graduates feel well prepared for independent practice in addiction medicine, including complex co-morbidities and systems-level issues?”
- A program confident in its training will:
- Provide concrete examples of alumni roles
- Highlight board pass rates and career trajectories
- A program confident in its training will:
“For international medical graduates, what has been the typical pathway to employment after training, considering visa and licensing constraints?”
- Critically important for your planning:
- J-1 waiver possibilities
- H-1B sponsorship by future employers
- Any alumni stories similar to your background
- Critically important for your planning:
“Is there structured mentorship around choosing an academic vs. community-focused career in Addiction Medicine?”
- Assess:
- Availability of mentors in different sectors
- Yearly career planning or individual development plans
- Assess:
Research, Quality Improvement, and Teaching
“What research or quality improvement opportunities are available in addiction medicine here?”
- Look for:
- Ongoing clinical trials
- Implementation science, health services research
- Overdose prevention, policy work, or public health collaborations
- Look for:
“Is scholarly activity required for graduation, and how are fellows supported to complete it (protected time, mentorship, statistical support)?”
- Clarify:
- Expectations vs. realities
- Whether previous fellows have presented at conferences or published
- Clarify:
“Are there opportunities to teach residents, medical students, or other disciplines about substance use disorders?”
- Teaching experience:
- Enhances your CV, particularly if you plan an academic career
- Deepens your own understanding of addiction principles
- Teaching experience:
“How does your program prepare fellows to become leaders in addiction medicine—through policy work, guideline development, or community engagement?”
- Leadership training is particularly valuable for IMGs who may aim to influence addiction care systems in their home countries.
Practical “What to Ask Program Director” Checklist
In the stress of interview season, it’s easy to forget key topics. Use this shortlist as a quick reference for what to ask the Program Director of an Addiction Medicine program as an IMG:
Training and Curriculum
- “What differentiates your program’s substance abuse training from others?”
- “How do you ensure fellows become comfortable addressing both addiction and complex medical/psychiatric co-morbidities?”
Support for IMGs
- “What has been your experience training international medical graduates in this program?”
- “How do you support IMGs through visa, cultural transition, and differences in prior training backgrounds?”
Supervision and Safety
- “How do you monitor that fellows are progressing appropriately and not being pushed beyond their competence?”
- “What mechanisms are in place if a fellow feels unsafe, overwhelmed, or under-supported in a particular rotation?”
Career Outcomes
- “Can you share specific examples of recent graduates’ career paths, particularly any IMGs?”
- “How do you help fellows prepare for board certification and the job market?”
Program Evolution
- “What changes have you made to the Addiction Medicine curriculum in the past 3–5 years, and why?”
- “Where do you see this program going in the next few years in terms of clinical sites, research, or community engagement?”
These questions are both substantive and signal that you are thinking beyond the immediate year—about the quality, trajectory, and integrity of your training.
Putting It All Together: Using Answers to Shape Your Rank List
As you proceed through interviews and ask these questions, document responses carefully. After each interview day, reflect on:
Clinical Exposure
- Did the program offer broad, well-supervised, and modern addiction training?
- Were harm reduction, co-occurring disorders, and diverse patient populations well represented?
IMG Friendliness
- Did they demonstrate experience and comfort with international medical graduates?
- Were visa and licensing questions answered clearly and confidently?
Program Culture
- Did trainees seem genuinely supported and not burned out?
- Did you sense respect for Addiction Medicine from other departments?
Career Fit
- Could you see yourself practicing the way their alumni do?
- Did research, teaching, or leadership opportunities match your aspirations?
Gut Feeling
- Did you feel respected and heard when asking your questions?
- Did responses feel transparent—or rehearsed and vague?
By combining structured questions with honest reflection, you move from “I hope they choose me” to “Is this the right place to train as an Addiction Medicine specialist and as an IMG?”
Frequently Asked Questions (FAQ)
1. As an IMG, is it acceptable to ask detailed visa questions during the interview?
Yes. Programs expect international medical graduates to clarify visa and licensing issues. Frame questions professionally, such as, “To ensure I can plan realistically, could you tell me what types of visas your institution typically supports for Addiction Medicine fellows, and whether there have been any recent changes in policy?” Avoid overly personal financial questions, but be very clear about visa type, timing, and institutional experience.
2. Which questions should I avoid asking during Addiction Medicine interviews?
Avoid:
- Questions easily answered on the website (salary, basic schedule, location)
- Questions that sound like you’re prioritizing lifestyle over patient care (e.g., “How little can I work and still finish?”)
- Overly aggressive or confrontational wording about program weaknesses
You can still explore challenges by asking, “What areas of the program are you actively working to improve, and how are fellows involved in that process?”
3. How many questions should I prepare for each interview?
Prepare a core list of 10–15 questions, but expect to use about 3–5 per individual conversation (PD, faculty, fellows). Some will be answered spontaneously during presentations. Prioritize:
- 2–3 questions on clinical training/substance abuse training
- 1–2 questions on IMG support and culture
- 1–2 questions on career development and outcomes
Have a few backup questions in case earlier sessions already cover your main points.
4. Are virtual interviews different in terms of what to ask programs?
The content of your questions is similar, but in virtual settings:
- Be especially deliberate in asking about program culture, since you can’t “feel” the place physically.
- Ask trainees, “What’s one thing about this program I would only notice if I were here in person?”
- Clarify logistics of remote work, tele-addiction services, and how the program adapted during crises (e.g., COVID-19), which also reveals flexibility and innovation.
Using this structured approach to questions to ask programs will help you, as an international medical graduate, identify Addiction Medicine training environments where you can thrive clinically, professionally, and personally—setting a strong foundation for a meaningful career addressing substance use disorders worldwide.






















