Landing an integrated plastics match is about far more than test scores and case logs. Programs are also evaluating whether you understand what you need from training and whether you can ask thoughtful, informed questions. The questions you ask residency programs—especially in plastic surgery, where training environments vary widely—can profoundly affect both how programs perceive you and how well you assess fit.
This guide focuses on what to ask them: specific, targeted questions to ask program directors, faculty, and residents during plastic surgery residency interviews, virtual visits, and second looks. It’s tailored to the realities of plastic surgery training, where case mix, autonomy, and mentorship can shape your future practice for decades.
Why Your Questions Matter in Plastic Surgery Interviews
Plastic surgery is uniquely heterogeneous: one program might be heavily reconstructive and microsurgery-focused, another primarily aesthetic and hand, and others will balance all of the above. Because of that variability, your questions to ask residency programs are crucial for three reasons:
Signal maturity and insight
Programs want residents who understand what plastic surgery residency entails. Thoughtful questions show you’ve done your homework, understand the specialty, and are thinking beyond “just matching.”Help you compare very different programs
Numbers like case volumes or board pass rates are only part of the story. Deeper questions reveal culture, mentorship, expectations, and sustainability of the training.Guide your rank list realistically
The integrated plastics match is notoriously competitive. Many applicants end up with more than one “great” program on paper. Knowing what to ask program directors, faculty, and residents lets you differentiate between places that are “good in general” versus “good for you.”
A useful framework: for every interview day, plan a small set of core questions you ask everywhere plus a few program-specific questions informed by their website, social media, or away rotation experience.
Core Program Questions: Understanding the Structure and Philosophy
These are high-yield questions you can adapt to nearly every plastic surgery residency interview. They help you understand how the program is built and where it’s going.
1. Program Vision, Growth, and Identity
Who to ask: Program Director (PD), Chair, Associate PD
Goals: Clarify the “direction of travel” for the program—crucial when training spans six or seven years.
Sample questions to ask program directors:
- “How would you describe the identity or niche of your plastic surgery residency—what do you want your graduates to be known for?”
- “In the last 5–10 years, how has the program changed, and where do you see the biggest growth in the next 5 years?”
- “What recent initiatives are you most proud of—for example, new faculty hires, new rotations, or new collaborations?”
- “If I came back in ten years, how do you hope the program will be different or improved?”
Why these work:
These questions demonstrate that you’re thinking about long-term training quality, not just prestige. They also help you spot red flags (e.g., major instability, frequent leadership turnover) and highlight programs that are proactive and strategic.
2. Case Mix, Autonomy, and Clinical Breadth
Who to ask: PD, faculty, senior residents
Plastic surgery training can be disproportionately weighted—some programs are micro-heavy, others aesthetic, trauma, craniofacial, or hand-centric. You want enough breadth to keep doors open, even if you think you already know your future niche.
Questions to ask about case exposure:
- “How would you describe your balance among reconstructive, microsurgery, hand, craniofacial, and aesthetic cases?”
- “Are there any clinical areas where you’re actively trying to grow the volume or recruit additional faculty?”
- “How do you ensure residents achieve adequate exposure to aesthetic surgery, including private-practice settings, if applicable?”
- “How is operative autonomy structured—how does it change from junior to senior years?”
For autonomy specifically:
- “Could you walk me through what a typical day in the OR looks like for a PGY-2 vs. a chief resident?”
- “In which rotations do residents feel they have the most hands-on operative responsibility?”
Green flags:
Clear, concrete descriptions (e.g., “As a PGY-5, you’re first assist on nearly all free flaps and can be primary on certain reconstructions”) and transparent acknowledgment of any limitations (e.g., “We’re light on peripheral nerve cases, so we partner with X center to supplement”).

Clinical Training Details: Day-to-Day Experience and Operative Development
Beyond big-picture vision, you need to understand what your actual life as a resident would look like.
3. Rotation Schedule and Workflow
Who to ask: PD, chief residents, mid-level residents
Rotation content:
- “How is the integrated plastics residency structured across the PGY-1 to PGY-6 years?”
- “Which off-service rotations do you consider most valuable, and have you made any recent changes based on resident feedback?”
- “How much time is spent at outside hospitals or private practice sites, and what is the value of those rotations?”
Day-to-day workflow:
- “What does a typical day look like for a PGY-1 on plastics versus as a senior resident?”
- “How often are residents in clinic versus the OR versus on call?”
These interview questions for them demonstrate that you’re thinking about how training actually happens, not just what’s listed on the curriculum chart.
4. Call Structure and Workload
Call can significantly influence your quality of life and your learning—particularly in specialties that cover trauma and emergent issues.
Questions to ask about call:
- “How is call structured—home vs. in-house, plastics-only vs. shared, and how does it change as you progress through training?”
- “On average, how many nights per month are residents on call at each level?”
- “What kinds of operative cases commonly occur at night, and how often do juniors get to be in the OR for them?”
- “How does the program monitor for duty-hour compliance and resident burnout?”
Ask residents:
- “Do you feel call is fair and sustainable?”
- “When you’re on call, do you feel supported by attendings and more senior residents?”
You’re looking for honesty and specificity. A program that addresses workload thoughtfully is more likely to support you when things get hard.
5. Resident Autonomy and Graduated Responsibility
Plastic surgery is technique- and judgment-heavy; meaningful autonomy is crucial.
Targeted autonomy questions:
- “How do attendings here balance supervision with allowing residents to take the lead in the OR and clinic?”
- “Can you give an example of a case type that is typically resident-run by the time you are a chief?”
- “Are there formal expectations or milestones for operative independence at different PGY levels?”
Ask residents to validate:
- “Do you feel you’re operating at an appropriate level for your training?”
- “Have there been times you wanted more autonomy, and if so, how did faculty respond?”
If you hear consistent, confident answers from both faculty and residents, that’s a good sign that their philosophy of autonomy is clear and genuinely implemented.
Culture, Mentorship, and Wellness: The “Invisible Curriculum”
The culture of a program often matters more than the brochures and statistics. Your questions to ask residency programs about culture can help you distinguish between supportive environments and toxic ones.
6. Mentorship, Feedback, and Professional Development
Plastic surgery careers are highly individualized—academic microsurgeon, private-practice aesthetic surgeon, hand specialist, global surgery, and more. Robust mentorship is essential.
Questions on mentorship and advising:
- “How are mentors assigned—formally, informally, or both? Can residents change mentors if their interests evolve?”
- “How often do residents meet with a faculty mentor or the PD for structured career advising?”
- “Does the program have dedicated mentorship for residents interested in specific paths (e.g., craniofacial, hand, gender-affirming surgery, global surgery)?”
For feedback and evaluation:
- “How frequently do residents receive formal feedback, and what does that process look like?”
- “How transparent are evaluations—do residents have access to written feedback and ways to respond or create improvement plans?”
These questions show you’re invested in growth and professionalism, not just surviving residency.
7. Resident Cohesion and Program Culture
Who to ask: Residents at all levels, chief residents, sometimes PD
Culture-oriented questions for residents:
- “How would you describe the resident culture here, both inside and outside the hospital?”
- “What characteristics make a resident successful in this program? Who tends to struggle?”
- “How does the program handle conflict, whether between residents or between residents and faculty?”
- “Do you feel comfortable asking for help—from co-residents, faculty, or administration—when you need it?”
For authenticity:
- “What’s something you wish you could change about the program?”
- “If you had to decide again, would you choose this program?”
You’re not looking for perfection, but for alignment: can you realistically see yourself in that group for six or more intense years?
8. Wellness, Support, and Life Outside of Training
Plastic surgery residents are at high risk of burnout, given long hours and high expectations.
Questions to assess wellness support:
- “What specific resources or initiatives does the program have to support resident wellness and mental health?”
- “How does leadership respond when residents are struggling personally or professionally?”
- “Is there flexibility for major life events—childbirth, illness, caregiving—while still keeping on track for graduation?”
Practical life questions:
- “How do residents typically live—do most rent nearby, buy homes, or commute from farther out?”
- “Are there childcare resources or institutional support for residents with families?”
Talking to residents off-camera or in small groups (especially in virtual cycles) is invaluable for honest answers.
Research, Aesthetics, and Career Outcomes: Preparing for Life After Residency
Given the competitiveness of plastic surgery fellowships and aesthetic practices, you’ll want to understand how programs prepare you for the next step.
9. Research Infrastructure and Scholarly Support
Integrated plastics residents are often heavily involved in research. Programs differ in expectations and support.
Research-focused questions:
- “What are the expectations for resident research productivity here? Is there a target number of projects or publications?”
- “Is there protected research time built into the schedule, and how is it used in practice?”
- “What type of research is most common—clinical outcomes, translational science, basic science, global surgery, education, health policy, or device development?”
- “Are there internal grants, statistician support, or partnerships with other departments to facilitate research?”
Ask senior residents:
- “How many projects or publications did you complete during residency, and what helped you be productive?”
- “Was it feasible to do meaningful research while maintaining a reasonable work-life balance?”
If you’re planning a heavily academic career, dig deeper:
- “Have residents been able to pursue advanced degrees (e.g., MPH, PhD, MBA) during or around residency, and how did the program support that?”
10. Aesthetic Surgery Exposure and Private Practice Perspective
Many integrated plastics residents ultimately work in private practice or aesthetic-heavy environments—even those who match fellowships first.
Questions to ask about aesthetics:
- “How is aesthetic surgery integrated into the curriculum here—for example, chief resident cosmetic clinics, private practice rotations, or on-campus med spa affiliations?”
- “How much direct hands-on experience do residents have with aesthetic procedures (both surgical and nonsurgical)?”
Look for concrete details like:
- Resident-run cosmetic clinic with graduated independence
- Structured aesthetic rotations with high case volume
- Exposure to practice management (billing, marketing, consultations)
You can also ask:
- “Do faculty or alumni offer teaching about the business side of aesthetic practice—contracts, building a practice, financial literacy, marketing?”
Exposure to the realities of practice management is an underappreciated but critical part of successful transition to independent plastic surgery practice.
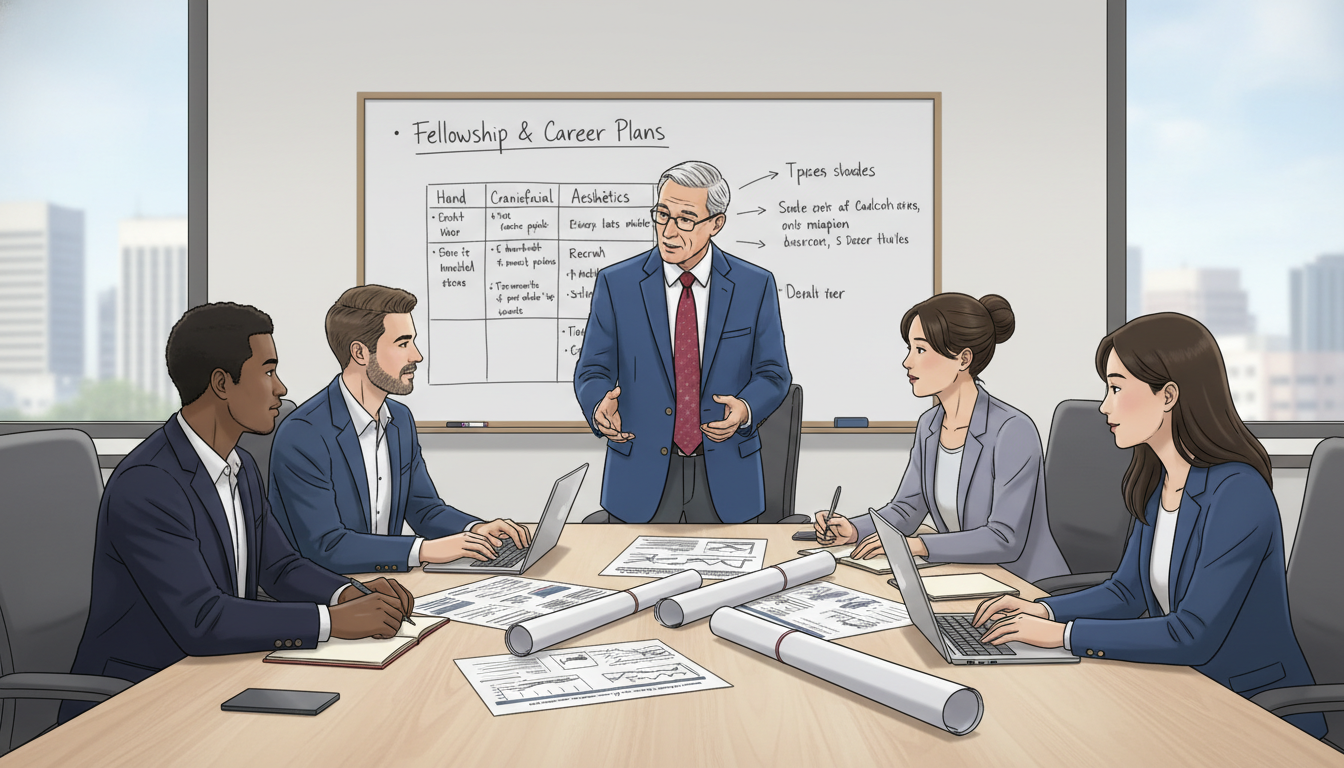
11. Fellowship Placement and Career Outcomes
For many applicants, a major lens for program evaluation is: “Where do your graduates go?”
Outcome-focused questions:
- “Over the past 5–10 years, what proportion of graduates have pursued fellowship training, and in which subspecialties?”
- “Where have residents matched for fellowship, and what kind of careers are they in now?”
- “How does the program support residents during the fellowship or job search—mock interviews, networking, letters, or institutional connections?”
You might also ask:
- “For residents not pursuing fellowship, what types of positions have they taken (academic vs. private, geographic spread, etc.)?”
- “How closely involved are faculty in helping residents align their training with their long-term career goals?”
Programs that can provide detailed, recent examples (not just a generic “our residents do well”) are usually more organized and supportive.
Tactical Interview Strategy: Who to Ask, When, and How
Even outstanding questions can miss the mark if they’re asked at the wrong time or to the wrong person. Strategize your question list for each interview day.
12. Matching Questions to the Right Audience
Program Director / Chair
Use this time for high-level questions about:
- Program vision and culture
- Program changes, leadership philosophy
- Evaluation, remediation, and long-term goals
- Institutional support and resources
Example “what to ask program director” questions:
- “What qualities do you most value in residents who thrive here?”
- “What changes have you made based on resident feedback in the last few years?”
- “If your own family member wanted to become a plastic surgeon, what aspects of this program would you emphasize to them?”
Faculty (especially subspecialists)
Great for specific content like:
- Subspecialty training (hand, craniofacial, gender-affirming, microsurgery, etc.)
- Aesthetic surgery and private practice exposure
- Research mentorship and collaboration
Residents (junior and senior)
Ideal for granular, honest details:
- Call, workload, and day-to-day routine
- Real culture, support, conflict management
- Logistics: housing, commute, cost of living
- Hidden strengths and weaknesses of the program
Have at least 2–3 resident-specific questions lined up for every breakout or social event.
13. Balancing Depth with Time Constraints
On busy interview days, you might only get time for 1–2 questions in a particular session. Plan ahead:
- Tier 1 (“must ask”) questions
These are core questions that truly affect how you rank programs (e.g., autonomy, case mix, wellness, aesthetics exposure). - Tier 2 (“nice to ask”) questions
These add nuance but aren’t deal-breakers (e.g., local extracurriculars, minor curriculum details).
Also:
- Avoid asking questions answered clearly on the website unless you’re seeking clarification or expansion.
- Rephrase questions to show insight. Instead of “What’s your call schedule?”, say:
“I saw on your website that call transitions from in-house to home at the senior level—how does that feel in practice for residents?”
14. Question Pitfalls to Avoid
- Overly aggressive or critical questions
Example: “I heard your residents are overworked. Is that true?”
Better: “How does the program monitor and respond to resident workload, especially on high-volume rotations?” - Excessive focus on vacation or time off early in the day
These are fair questions, but don’t lead with them. Ask once you’ve covered education and culture. - Asking, ‘So… do you think I’ll match here?’
It puts interviewers in a difficult spot and can come across as naive or inappropriate.
Focus on professional, insightful dialogue. Let your questions reflect your curiosity and seriousness about plastic surgery training.
Putting It All Together: Crafting Your Personal Question List
Use this framework to prepare your own set of interview questions for them before each interview:
- Non-negotiables
- What aspects of training are truly essential to you (e.g., strong micro, robust aesthetics exposure, geographic needs, wellness focus)?
- Program-specific curiosities
- From their website, social media, or away rotation: are they building a new microsurgery program? Recently recruited a craniofacial surgeon? Starting a gender-affirming surgery service?
- Standard comparison set
- Have 5–7 “standard” questions that you ask nearly everywhere, so you can directly compare programs later.
A sample core list might include:
- “How would you describe the program’s identity and the kind of plastic surgeons you aim to train?”
- “How is operative autonomy structured from junior to senior years, and in which rotations do residents gain the most independence?”
- “What are the strengths of your case mix, and are there any areas you’re actively working to grow?”
- “How does the program support resident wellness and respond when someone is struggling?”
- “What have your graduates done in the last 5–10 years in terms of fellowships and practice types?”
- “What changes have you made recently in response to resident feedback?”
With this foundation, you’ll walk into each interview ready to engage meaningfully, assess programs clearly, and present yourself as a mature future colleague in a highly competitive integrated plastics match.
FAQ: Questions to Ask Programs in Plastic Surgery
1. How many questions should I ask in each plastic surgery interview?
Aim for 1–2 focused questions per interviewer and several for resident sessions. It’s better to ask a few thoughtful questions than to rush through a long list. Prioritize questions that truly affect your ranking decisions (autonomy, culture, case mix, outcomes).
2. Is it okay to ask residents different questions than faculty or the program director?
Yes—and you should. Ask faculty and the PD about program vision, curriculum, and philosophy. Ask residents about real lived experience: call, workload, support, and culture. Slightly different versions of the same question to both groups can reveal important insights or disconnects.
3. Can I ask direct questions about board pass rates and fellowship placement?
Yes, as long as you phrase them professionally. For example:
- “Would you be willing to share your board pass rates over the past few years?”
- “Could you describe your graduates’ recent fellowship matches and career paths?”
Programs expect these questions and should be transparent with data and context.
4. How do I remember each program’s answers when making my rank list?
Right after each interview day, spend 15–20 minutes jotting down:
- Key phrases or impressions from your questions (e.g., “Strong micro, limited aesthetics but residents rotate with local private practice group”)
- Pros/cons related to your non-negotiables
- Any red or yellow flags that arose from answers or from how questions were handled
Organize these notes in a simple spreadsheet or document. When it’s time to certify your rank list, you’ll have more than vague impressions—you’ll have a structured comparison based on the questions you deliberately asked.






















