It is 11:42 p.m. You are still in the hospital. Your last patient just finally got a bed. Your co-intern is starting another admit “because it is easier for you to finish the workup.”
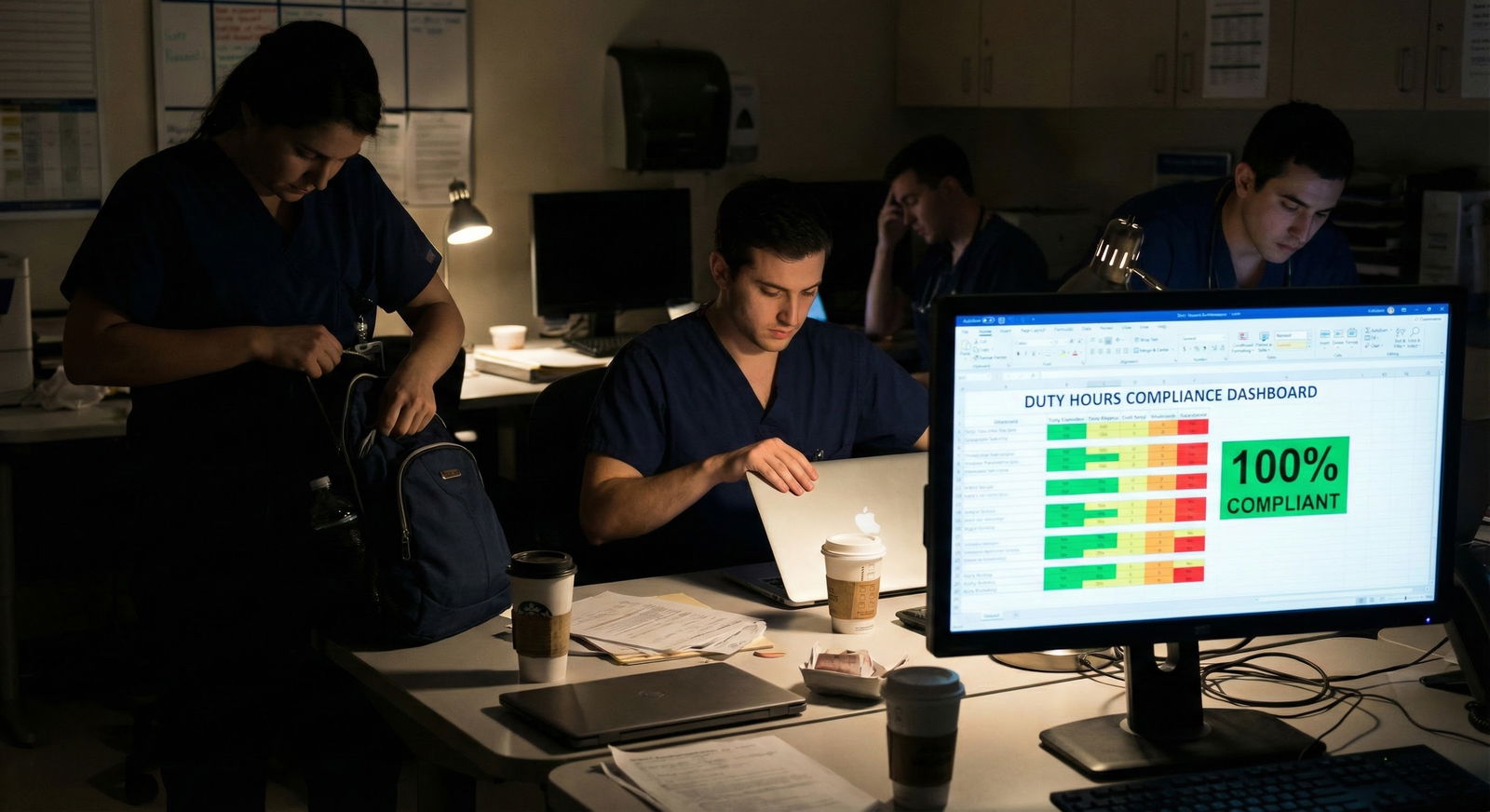
Your duty hours for the day? Already logged as 6 a.m. to 7 p.m. Clean. Compliant. Fiction.
If this sounds familiar, your program almost certainly has a duty hour “culture” problem. And under that umbrella sit a bunch of very specific, repeatable tricks programs use to appear compliant while systematically violating the rules.
Let me walk through the concrete patterns. Not vague “red flags.” Actual workflows, phrases, and data patterns that scream: this program is not honest about hours.
1. The Core Reality: How Duty Hour Dishonesty Actually Looks
Start with this: honest programs and dishonest programs often look identical on paper. Both will:
- Report 100% ACGME compliance most months
- Have a policy PDF that dutifully parrots the 80-hour rules
- Show you a smiling slide at orientation saying “We take duty hours very seriously”
The difference is not in the documents. It is in how people behave when those rules collide with reality.
There are a few recurring pressure points where programs decide whether they value compliance or optics:
- When a resident is clearly going to break 80 hours
- When sign-out time comes and the list is still a mess
- When a rotation is chronically understaffed
- When a resident speaks up about hours honestly
If the response at those moments is “log fewer hours,” “do your notes from home,” “just don’t put it in New Innovations,” you are not in a gray zone. That is falsification. People like to dress it up, but that is the bottom line.
2. Language Patterns: Exact Phrases That Signal Trouble
Programs rarely say, “We lie about duty hours here.” They say it sideways.
Here are specific phrases I have seen or heard that should light up your radar.
2.1 The “Fix It in the System” Phrases
These are used when your actual hours are inconvenient.
- “Just adjust your clock-out time so it doesn’t flag.”
- “You can’t log going over 80; it triggers a citation.”
- “If you put that in, it looks bad for the program.”
- “Don’t log separately for the conference—that is included in your shift.”
- “Put your PTO day as a workday so our reporting is consistent.”
Translated: “We care more about our Excel sheet than your life.”
A genuinely compliant program says things like:
- “If you are going over 80, you must log it so we can fix the schedule.”
- “We will get cited before we ask you to lie. Enter what actually happened.”
Very different vibe.
2.2 The “You Are the Problem” Phrases
The gaslighting scripts are almost word-for-word across programs.
- “Other residents don’t seem to be having duty hour issues.”
- “You need to work on your efficiency; that is why your hours are high.”
- “No one else is logging like this.”
- “Are you sure you understood the logging guidelines?”
Notice the pattern: individual blame, not structural reality.
If the ICU service has been overrun for 6 months and a program leader is still framing it as your personal inefficiency, they are not being honest. With you, or with themselves.
2.3 The “Off the Record” Coaching
The worst sign: informal “teaching” on how to game the system.
- “Most of us just log 6–6 no matter what.”
- “On nights we all put 13 hours, even if we stay longer.”
- “If you go over 80, just shave a couple of hours off your golden weekend.”
- “Don’t log at home call unless you physically come in.” (Which is wrong. ACGME: home call counts toward the 80, and in-house work after home call counts as in-house call.)
These are not misunderstandings. This is a culture of deliberate under-reporting.
3. Data and Patterns: What Falsified Duty Hours Look Like in the System
You can often see the dishonesty in the data. Even without direct access to the administrative back end.
Let me lay out the main fingerprints.
3.1 The 79–80 Hour Plateau Problem
If your program showed real data across the year for a busy service, it would look choppy—some weeks lighter, some weeks brutal, holidays, random disasters.
Instead, many show compliance curves like this:

| Category | Value |
|---|---|
| Week 1 | 78 |
| Week 2 | 79 |
| Week 3 | 80 |
| Week 4 | 79 |
| Week 5 | 80 |
| Week 6 | 79 |
| Week 7 | 80 |
| Week 8 | 79 |
If nearly every single “busy rotation” week clusters between 78–80 hours, for everyone, that is not real. Residents are not robots. Sick call happens. Admissions spike. Snowstorms occur. The distribution should be messier.
Red flag pattern:
- Nobody ever logs 82 or 84
- Very few weeks under 70 on services known to be malignant
- Different rotations with equivalent work but magically identical hours
It looks too clean because it is.
3.2 Uniform “Template Hours” for Everyone
Another common trick: using default hours or “expected” hours instead of reality.
Tell-tale signs:
- All interns on a rotation log exactly 6a–6p. Every single day.
- Night float is always 12 hours, even when you routinely stay late for sign-out.
- Everyone’s “weekend” day off is a perfect 0 hours, even though people come in for presentations, pre-rounding, or procedures.
If four different residents with different patients, attendings, and commute times all magically clock identical daily hours across the entire month, you are not looking at reality. You are looking at a template.
3.3 Mysterious “Disappearances” of Peak Weeks
Watch for what happens after truly awful stretches.
You have a week with:
- Three codes
- Two overnight OR emergencies
- Day team staying late to help nights
- Cross-cover disasters
Everyone is wrecked.
Then at the end of the pay period, leadership casually says, “Remember to double-check your duty hours so we don’t get dinged.”
And afterward, you hear this:
- “Oh yeah, I just did 6–6 all week. Everyone does.”
- “I only logged until 10 p.m. even though I stayed till midnight.”
If your worst weeks never show up as violations, they are being scrubbed. By design or by fear.
4. Structural Tricks: How Programs Build Schedules to Hide Overwork
Dishonesty is not just about what gets typed into New Innovations or MedHub. It shows up in how schedules are engineered.
4.1 “Paper Compliance” Rotations
Some rotations are specifically structured to clean up the numbers rather than improve education.
Patterns to look for:
- A mysteriously light “clinic” or “research” week appears right after the heaviest ICU block, to bring the rolling 4-week average back under 80
- A random “admin week” exists that is mostly pager coverage and catching up on documentation—still work, but logged as lighter duty hours
- Home call rotations that are marketed as “light” but function like full in-house call, with the expectation that you come in almost every night
On paper, the 4-week average looks fine. In reality, you lived through 3 weeks of 95–100 hours followed by 1 week of 50 hours where you still worked and did not really recover.
That is rule-lawyering, not protecting you.
4.2 The “Work-from-Home” Shell Game
I see this constantly now: using EHR remote access to offload charting, notes, and inbox management to “home time,” then pretending that is not work.
Specific patterns:
- Pre-rounding charts and writing full notes from home at 4:30–6:30 a.m., but logging start time as 6 or 7 a.m.
- Finishing 1–3 hours of notes at home after leaving the hospital and not counting that as work
- Being paged or called by attendings in the evening to update plans, but documenting without logging the time
ACGME is clear: any clinical work counts as duty hours, regardless of location.
But programs that worship optics will talk about “maximizing in-hospital efficiency” then quietly pretend home work does not exist.
If the expectation in your program is, “[insert EHR name] access from home is just part of being a good resident,” that is a problem.
4.3 The “You Are Off… But Not Really” Trick
Residents will recognize this pattern instantly.
- Your schedule shows a post-call day as “OFF”
- In practice, you are expected to:
- Present QI projects
- Attend mandatory didactics
- Join noon conferences
- Respond to “just one thing” patient questions or notes
Programs then count this as a day off to meet the “1 day in 7 free of clinical duties” rule. Reality: it is a pseudo-day-off infected with work.
5. Behavioral Red Flags: How People React When You Tell the Truth
The culture really shows itself when someone actually enters true hours.
5.1 The “Compliance Meeting” That Is Really a Warning
You log your actual hours for a terrible ICU month. You hit 90–95 hours for a couple of weeks. Suddenly you are summoned.
The meeting sounds like:
- “We noticed some outlier logging patterns.”
- “Your duty hours are much higher than your peers.”
- “We need you to adjust to meet ACGME expectations.” (Revealing: they mean your data, not your schedule.)
- “We do not want the RRC on our backs over logging inaccuracies.”
Notice what is not happening:
- No change to staffing
- No adjustment of admission caps
- No genuine workload analysis
- No temporary schedule relief or help
They are not addressing the work. They are addressing the spreadsheet. That is a classic sign the program is more afraid of external citations than internal burnout.
5.2 Peer Pressure from Senior Residents
Sometimes the pressure does not come from faculty. It comes from seniors who have absorbed the culture and are now enforcing it.
Behaviors that should make you pause:
- Seniors telling interns: “Do not log over 80. It hurts all of us.”
- Chiefs privately messaging: “Please fix your hours; this rotation is supposed to be compliant.”
- Residents bragging about “never breaking 80” on services where everyone is a zombie
This is how malignant patterns perpetuate. New interns walk in, see everyone else under-reporting, and assume they are the weird ones for being honest.
5.3 Passive-Aggressive Retaliation
If someone consistently logs accurately and leadership responds by:
- Pulling them from desirable rotations
- Excluding them from elective opportunities
- Making comments on evaluations about “time management” or “efficiency” with no specifics
- Labeling them as “not a team player”
that is not accidental. That is punishment for telling the truth.
You will sometimes hear thinly veiled threats:
“Well, fellowship directors will see if you are not able to handle the workload.”
Translation: “Stop complaining, or we will frame you as weak.”
6. During Interviews and Rotations: How to Detect the Pattern Early
You do not want to figure this out 3 months into intern year. So let us talk about what you can pick up before you sign.
6.1 Questions That Expose Duty Hour Culture
Ask residents questions that force specific answers, not generic reassurances.
Examples:
- “On your busiest rotation, what is the earliest you typically start working on patient care (including from home) and the latest you usually finish?”
- “How many times in the last year do you think you personally went over 80 hours in a week if you count all the home work honestly?”
- “What happens here if someone logs more than 80 hours for several weeks in a row?”
- “Do people ever get called in to change their logged hours?”
Watch for hesitation, side-eye glances, or the “off the record” comment after the group Q&A:
“Ask me later, not in front of them.” That tells you exactly what you need to know.
6.2 Contradictions Between Leadership and Residents
One of the most reliable patterns:
- Program leadership: “We almost never have duty hour violations.”
- Residents, privately: “We all just log 6–6.”
Or:
- PD / APD: “We strongly encourage honest logging; we have no tolerance for falsification.”
- Reality: multiple residents tell you about meetings where they were asked to “reconsider” entries.
| Situation | Healthy Program Response | Toxic Program Response |
|---|---|---|
| Repeated 80+ hours logged | Adjust staffing/schedule | Ask resident to change entries |
| Home charting common | Count as duty hours, try to reduce | Pretend it is personal choice |
| Resident flags chronic overwork | Joint problem-solving | Blame efficiency/attitude |
| Interview questions about hours | Specific, candid answers | Vague, overly polished reassurances |
6.3 Sub-Internship Reality Check
If you do a sub-I or visiting rotation, you can watch this in real time.
Look for:
- What time people actually show up versus what time they say they log
- Whether seniors openly joke: “Make sure you log out by 6” as you drag yourself out at 8 p.m.
- How chiefs respond when a call night goes off the rails—do they say, “Log what you worked, we’ll fix the next call schedule,” or “Try not to put too much in the system”?
Sub-Is are where programs slip. Residents forget to maintain the polished script and just talk like they usually do. Listen.
7. Institutional Red Flags: When the Problem Is Baked In
Some duty hour dishonesty is not local. It is systemic.
7.1 Chronic Under-Staffing Without Structural Solutions
If a program:
- Has been short 2–4 residents for multiple years
- Lost a chunk of faculty or merged services
- Added new clinical responsibilities (e.g., extra hospitalist service)
and the primary fix has been “work harder” instead of hiring more people or revising caps, then you can be confident duty hours are being patched with dishonesty or burnout. Usually both.
You will hear: “We are a hardworking program; that is why our graduates are so strong.”
Translation: “We are normalizing unsafe workload and wrapping it in pride.”
7.2 Dismissals and Remediation Quietly Tied to “Professionalism”
You may never get the whole story about dismissed residents. But patterns leak:
- Rumors that someone got in “professionalism trouble” for “complaining a lot”
- Vague stories about a resident “not being a good fit” after raising concerns about workload
- Whisper networks saying, “Do not put that in writing; they will use it against you”
If multiple cohorts recall versions of this, the message is clear: speak up at your own risk.
7.3 PD and DIO Messaging
Sometimes leadership reveals a lot in how they talk about ACGME and oversight.
Watch for:
- Dismissing ACGME as “out of touch” or “not understanding real clinical life”
- Joking about surveys being “our annual performance exam” where residents should “give us good grades”
- Telling residents explicitly, “Do not air our dirty laundry on the ACGME survey”
That last one is a bright, flashing red sign. If programs are coaching residents to sanitize anonymous responses, you can safely assume they are also coaching duty hour entries.
8. Why Programs Do This (Even the Ones That “Mean Well”)
Let me be blunt: some leadership know exactly what they are doing and simply do not care.
But many are trapped in a bad system:
- Hospitals depend on resident labor to run unprofitable services
- Hiring more NPs/PAs or residents costs money
- ACGME citations put accreditation and hospital marketing at risk
- Administrators push for “no violations” dashboards as KPI metrics
So leaders, especially mid-level (chiefs, APDs), start bending:
- “We are not actually making you lie, just… interpret home work differently.”
- “We need to show improvement this year; please help us out.”
Intentions aside, the effect is identical: unsafe hours, dishonest paperwork, and residents who learn that truth-telling is punished.
This is how you end up with residents falling asleep while driving home, missing their own medical appointments, and considering quitting medicine, all while the program proudly shows 100% ACGME compliance slides at the Clinical Competency Committee meeting.
9. The Future: Tracking, EHR Data, and Less Room for Games
The future is going to make this harder to hide. Slowly.
9.1 EHR and Badge Data vs Logged Hours
Hospitals already track:
- Badge swipes in and out of clinical areas
- EHR log-in and log-out times
- VPN access times for remote charting
It does not take a genius to compare these with logged duty hours. Some institutions have quietly done exactly that and discovered extreme under-reporting.

| Category | Value |
|---|---|
| Resident A | 12 |
| Resident B | 10 |
| Resident C | 15 |
| Resident D | 8 |
(Values above could represent “extra unlogged hours per week” based on login analysis. The key is the discrepancy pattern.)
Once this type of analysis becomes routine (and it will), the “we did not know” defense collapses. Either programs fix the work or they become indefensible.
9.2 Resident-Driven Transparency
You are already seeing more:
- Anonymous social media threads calling out malignant programs by name
- Residents screenshotting directives like “please adjust your hours” and sharing them widely
- Applicants cross-checking internal reputations against the shiny websites
Programs that double down on dishonesty will eventually struggle with recruitment, retention, and accreditation. It may be slow, but it is coming.
10. What You Can Actually Do If You Are Living This Now
I am not going to pretend everyone in a toxic duty hour culture can just whistleblow and walk away unscathed. There is risk. You know that.
But there are some practical moves.
10.1 Document Reality For Yourself
Keep a private record of:
- Actual start and stop times (including home work)
- Specific days you were asked or pressured to change entries
- Phrases used, who said what, dates of those conversations
This is not about being dramatic. It is about having specifics if you ever need to talk to the DIO, ombuds, or ACGME.
10.2 Find Out if You Have Any Safe Channels
Some institutions genuinely have:
- A functional GME office that will back residents
- An ombuds or trainee advocate outside the program
- Anonymous reporting processes that have led to real changes in the past
Ask senior residents you trust: “Has anyone ever actually used [X channel] and gotten help without retaliation?” The answer will tell you how much risk you are taking.
10.3 Protect Your Own Line
At some point, it becomes a basic safety issue. If you are routinely:
- Over 90–100 hours a week
- Doing complex procedures exhausted
- Driving home half-asleep
you need to start prioritizing survival over politeness.
That might mean:
- Logging the truth even if you get called in
- Saying, “I am not safe to take more admissions” when you are clearly past the line
- Using the ACGME resident survey very deliberately to describe patterns
No article can remove the power imbalance. But pretending the tricks are normal or harmless just feeds the machine.
11. One Visual: How the “Compliance” Culture Actually Feels
Sometimes it helps to see the mismatch drawn out.

| Step | Description |
|---|---|
| Step 1 | Real Clinical Workload |
| Step 2 | Resident Exceeds 80 Hours |
| Step 3 | Log True Hours |
| Step 4 | Adjust Schedule and Staffing |
| Step 5 | Pressure to Change Entries |
| Step 6 | Underreported Hours |
| Step 7 | ACGME Dashboard - 0 Violations |
| Step 8 | No Structural Change |
| Step 9 | Program Culture |
That loop on the right—underreported hours, fake clean dashboard, no structural change, same overwork—that is exactly what you are trying to detect and avoid.
12. The Bottom Line: How to Recognize the Tricks Quickly
Let me distill this down.
Listen to the language.
“Adjust your hours,” “do not log that,” “it looks bad for the program,” “everyone else manages” — those are not minor comments. They are code for: your honesty is inconvenient.Look at patterns, not one-off weeks.
Perfectly clean 79–80 hour weeks for everyone, template logging, brutal months that never generate violations—those are not flukes. They are fingerprints of systemic under-reporting.Trust the off-the-record conversations.
Residents pulling you aside to say “We all just log 6–6,” chiefs warning you not to put certain things in the system, leadership coaching you to “be careful” on surveys—believe that. That is the real program, not the orientation PowerPoint.
If you remember nothing else: honest programs get duty hour violations sometimes. That is what happens when you care more about resident safety than your accreditation report. A program that is “always perfectly compliant” on paper, despite brutal workloads, is not actually compliant. It is just very good at lying.






















