Most call schedules are designed to “cover the service,” not to protect humans or patients. That is the core design flaw.
Let me break this down specifically. You can often predict a residency’s burnout rate and safety profile from a single PDF: the call schedule. The patterns are there. Fragmented circadian rhythms, hidden workload stacking, fake “days off,” and mathematically impossible expectations baked into the calendar.
You are not “overly sensitive” if those patterns worry you. You are reading the system correctly.
This is a guide to those red flags. How to recognize them, why they matter physiologically and operationally, and what they say about the culture of a residency program.
1. The Fundamental Problem: Coverage-Centered, Not Human-Centered
Programs that get call wrong almost always share the same root mindset: call exists to fill gaps in coverage, and residents are the cheapest, most flexible patch.
The better programs flip that. They treat call as a high-risk, high-complexity function that demands:
- Stable sleep-wake patterns where possible
- Protected recovery time
- Predictable load relative to experience level
- Explicit safety margins
If you want a litmus test: ask yourself, looking at a schedule, “Is this designed around biology and patient risk, or around a spreadsheet of vacancies?”
Two Tells Right Away
- The schedule changes every month, with no consistent pattern.
- The night coverage model looks like someone took a bag of names and poured them onto a calendar.
If leadership cannot articulate a coherent philosophy of call design, it is almost always coverage-first, safety-last.
2. Circadian Chaos: Rotating Nights and “Flip-Flop” Schedules
This is one of the most reliable predictors of burnout. It is also one of the easiest to see.
The Classic Red Flag Patterns
- 24-hour call on Saturday, then regular 6 a.m. start on Monday
- Alternating day/night every 2–3 shifts (D–N–D–N)
- “Night float” blocks that are 3–4 days long instead of 1–2 weeks
- Month where you do: 5 days → 4 nights → 6 days → 3 nights
This is circadian violence. You do not “adapt” to it; you accumulate sleep debt and cognitive impairment.
Why This Predicts Burnout and Safety Events
Psychophysiology is not optional. If your schedule ignores it, your brain will fail you on its own schedule.
- Fragmented sleep and rapid time-shifts impair attention, working memory, and decision-making
- Reaction time and error rates after 24 hours awake rival moderate intoxication
- Mood changes (irritability, emotional blunting, hopelessness) are not character flaws; they are the system showing through
You see this clinically: the cross-cover resident who cannot recall the last set of vitals, the intern who forgets to reorder home anticoagulation, the senior who snaps at nursing and then cannot repair the relationship.
The red flag is not “night float” itself. The red flag is unstable nights.
What a Reasonable Pattern Looks Like
- Night float in 1–2 week blocks, fixed start time, consistent team
- At least 48 hours between switching from days to nights (preferably a transition weekend)
- No “oscillating” every few days between days and nights
If a program proudly tells you that “everyone shares nights equally” but the pattern flips back and forth constantly, they have not understood the real constraint: circadian stability.
3. Fake Days Off and the “Q3-Q4-Plus-Extra” Reality
Programs love to say “we’re compliant” and “you get days off.” The schedule often tells another story.
Here is what to look for.
How Fake Days Off Show Up
- Post-call days listed as “OFF,” but you worked until 10 or 11 a.m. and still have charting to do
- “Golden weekend” that is actually Friday PM post-call + Saturday off + Sunday 24-hour call
- The day before a 24-hour call is a full clinical day (so your “weekend off” is 1 true day)
- “Jeopardy” days that are theoretically off but routinely used as coverage without any post-hoc adjustment
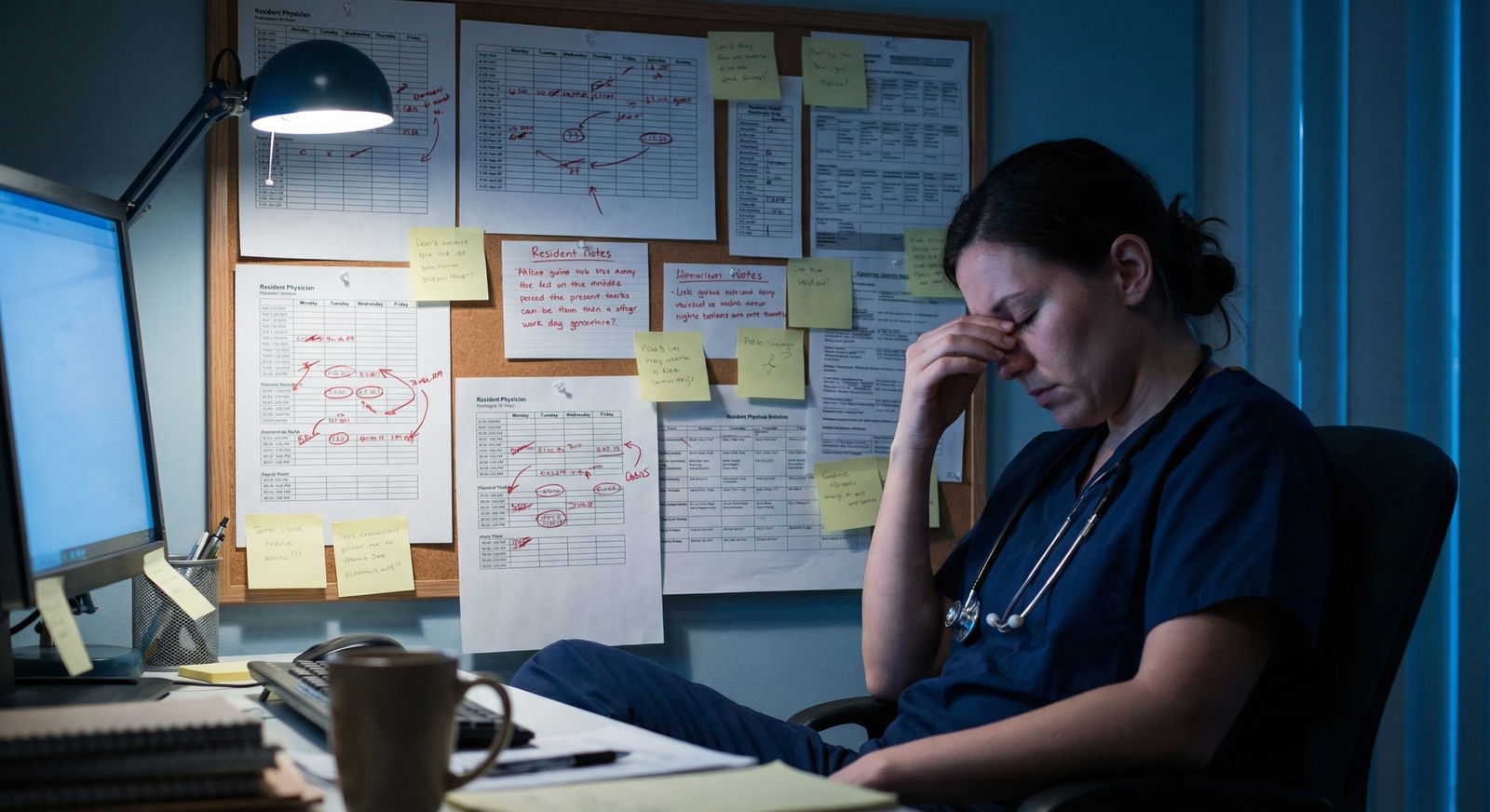
The emotional burnout comes from the mismatch between label and reality. When the schedule calls something a “day off” and your body experiences it as survival and cleanup, you stop believing what leadership says.
Safety Angle
Residents who never truly detach:
- Keep a running mental to-do list that leaks into non-working time
- Have chronic attention fatigue and tunnel vision on shift
- Are more likely to miss soft signs of deterioration or early sepsis because they are “just trying to survive until sign-out”
If you see a pattern where every week is effectively 6+ days of real work, expect burnout by mid-year and errors by late winter.
How to Read the Calendar Critically
Do this honestly:
- Count only days where you have zero clinical expectation (no call start, no post-call, no required teaching) as off.
- Look at any four-week block and count true days off.
- If that number is under 4, you are not in a safe system. You are in a slow-boil environment.
4. Hidden Workload: Non-Clinical Duties Stacked On Call
This is subtler, and it separates average from genuinely bad programs.
Red-flag schedules do this: they treat call as “just another shift” and stack normal program expectations on top of it.
Common examples:
- Mandatory noon conference attendance after overnight call
- Academic half-days that always fall the morning after 24-hour call
- Continuity clinic not rescheduled for post-call days (“you can power through 4 half-days a month…”)
- Resident-led QI meetings scheduled at 7 a.m. after night coverage
I have watched a PGY-2 fall asleep standing up during morning report, then get passive-aggressively called out for “engagement.” The schedule had him on 24-hour call every 4th night with required 7 a.m. conference every weekday. That is not a professionalism problem. That is an engineering failure.
Why This Is A Safety Problem
Cognitive load is not just patient volume. It is also:
- Teaching preparation
- Documentation backlogs
- QI and committee work
- Studying for boards
When those are layered onto already heavy call blocks, you end up with:
- Residents charting after 28–30 hours awake
- Critical tasks (reconciling meds, handoffs) done while rushing to meet non-clinical obligations
- Blame placed on individuals rather than on the design that made failure predictable
A well-run program will visibly carve out protected spaces. A red-flag program will say “everyone else did it, you will be fine.”
5. Unsafe 24-Hour Call Variants
The issue is not just 24 hours. It is what rides on top of it.
Look for these specific design flaws:
1. “24 + Morning Rounds + Clinic”
You see this all the time in medicine and surgical subspecialties.
The schedule shows:
- Call: Saturday 7 a.m. – Sunday 7 a.m.
- Then “Ward” Sunday 7–11 a.m.
- Then Monday 7 a.m. start like nothing happened
Mathematically, you get:
- 28+ continuous hours on duty
- Minimal ability to sleep overnight because admissions, cross-cover, and pages continue until 3–4 a.m.
- Less than 24 hours total between the start of one serious hospital commitment and the next
Board scores and clinical outcomes both correlate with cognitive performance. You will not be at full capacity in that state. Nobody is.
2. 24-Hour Call With Orphaned Teams
Another red flag is a call system where:
- The “on-call” resident covers multiple services they do not routinely rotate on
- Handoffs are group, verbal, and rushed—no structured tool, no written backup
- Nurses do not know who to call, so they shotgun-page everyone until someone picks up
What happens: the on-call resident is cognitively overwhelmed by context-switching across 30–60 patients they barely know. Decision quality drops. Near-misses become normal.
3. 24-Hour Call On Services With No Night-Float Help
Trauma, OB, ICU, and busy medicine services sometimes still run 24s with no targeted additional support at peak times. Schedules where a single resident:
- Admits new patients
- Cross-covers a huge census
- Responds to all rapid responses and codes
- Accepts transfers
- Answers all floor pages
That is not “challenging.” It is unsafe by design.
6. Number of Calls Is Less Important Than Their Distribution
Programs love to quote “you only have X calls per month.” The real question is: how are those calls spaced and what do they surround?
Let me show you a useful way to think about it.
| Pattern Type | Example Block | Risk Profile |
|---|---|---|
| Clustered, then true rest | Call on 1, 4, 7; full weekend off after | Moderate |
| Even Q4, honest post-call | Call on 2, 6, 10, 14, etc. | Low–Moderate |
| Irregular, no buffer | Call on 1, 3, 9, 12, 18, 21 | High |
| Call before/after nights | Days → 24 → Nights | Very high |
The worst schedules stack stressors: a 24, then a single day “off,” then right into nights. Or multiple calls in the span of 5–6 days with non-clinical duties inserted between.
Signs Of Thoughtful Distribution
- No more than 2 high-intensity shifts (24s or nights) in any rolling 5 days
- Intentional pairing of lighter clinics/rotations around call-intense blocks
- Stable pre-call and post-call routines: same sign-out time, same team structure
If you see a pattern where a program “dumps” call on certain months (e.g., intern medicine + ICU + nights all within 4 months), expect those cohorts to be worn down early and more error-prone.
7. Cross-Cover Design That Guarantees Errors
Cross-cover is unavoidable. How you structure it is a choice.
Red-flag schedules put residents into cross-cover roles where:
- They are responsible for 60–90 patients across multiple floors
- They do not have access to a real-time, updated list with priorities
- Day teams sign out “FYI” after “FYI” and no triage is enforced
- The same resident is simultaneously covering codes/rapid responses
What you end up with:
- Delayed responses to pages about truly sick patients
- Low-yield calls (pain meds, diet changes) overwhelming the serious ones
- Residents forced to cut corners on real evaluations because the queue never dries up
A simple structural design change—limiting cross-cover ratios, structured sign-out, separating code coverage when feasible—can cut errors down. When leadership does not do that, you are seeing their actual risk tolerance.
8. Violations Hidden Behind Technical “Compliance”
ACGME duty hours created an entire subculture of “gaming the system.” Programs proudly say they “never violate,” yet residents are obviously exhausted and cynical. The schedule often reveals how.
Common patterns:
- “Voluntary” pre-rounding before your official start time
- Unwritten expectations to stay late, chart from home, or “finish the work” off the clock
- Pre- and post-call hours manipulated on paper to appear compliant (“just log 24, everyone does it”)
- Moonlighting encouraged in PGY-2+ without adjusting base schedule
If you see a schedule that is barely under the 80-hour limit each week, that is a red flag in itself. Real life always adds overhead: transit, charting, family calls, educational sessions.
What This Means Culturally
A culture comfortable with paper compliance and real-world violation will:
- Blame residents personally when mistakes happen (“be more careful”)
- Be hostile to raising safety concerns (“we all went through it”)
- Punish honesty in duty-hour reporting
That is not just unpleasant. It is dangerous. Near-misses never become data. The system never learns.
9. Transitional Rotations: Emergency, ICU, and Night-Heavy Blocks
Certain rotations amplify any design flaws in your call system.
ICU And Night Design Flaws
In ICU rotations, I watch for:
- Alternating weeks of days and nights without transition time
- No break before starting a heavy ICU night block
- Schedules where juniors are on nights alone, with remote attending coverage and in-house senior stretched thin across multiple units
Those are perfect conditions for missing subtle trends: rising lactate, early delirium, insidious respiratory failure. Exhausted residents tunnel on the obvious emergencies and miss the slow burns.
Emergency Department Schedules
Emergency medicine can be done well or terribly.
Red flags:
- “Clopening” shifts—late evening followed by early morning
- Frequent isolated night shifts sprinkled through mostly day shifts
- No predictable pattern—schedule comes out late and changes often
- High-intensity trauma/critical care shifts placed at the end of long runs
If you see an ED schedule that looks like a random-number generator drew your shift times, expect chronic sleep debt. And ED decisions under sleep debt can go very wrong very quickly.
10. How Call Schedules Predict Future Program Behavior
This is the meta-point: the call schedule is not just about fatigue. It is a window into how a program thinks.
Programs that treat call as:
- A necessary evil to be minimized and buffered → usually healthier, more sustainable
- A “rite of passage” or test of toughness → usually dismissive of burnout and safety
- A solved problem they no longer revisit → often stuck in outdated patterns
You can also infer how responsive they are to feedback.
Ask current residents: “Has the call schedule changed meaningfully in the last 3 years based on resident feedback?”
If the answer is no, or you get a smirk and “we keep asking,” believe them. You are looking at a rigid culture that tolerates avoidable harm.
11. What A Safer, Saner Call Design Actually Looks Like
To make this concrete, here is a rough picture of a program that takes this seriously.

| Category | Value |
|---|---|
| Week 1 | 3 |
| Week 2 | 2 |
| Week 3 | 3 |
| Week 4 | 2 |
You see:
- Nights in 1–2 week blocks with stable start/end times
- No 24-hour call followed immediately by another full workday
- Cross-cover ratios capped, with clear backup when the census spikes
- True protected recovery days after intense call sequences
- Non-clinical expectations lightened or waived on post-call/peak call weeks
And crucially: they audit themselves. They use:
- Fatigue-related incident reviews
- Anonymous resident feedback on call intensity
- Adjustments across academic years, not once-a-decade restructures
When you see that, do not underestimate it. It is rare. Programs that manage call thoughtfully tend to be better at everything else: feedback, wellness, teaching, remediation.
12. How To Evaluate A Program’s Call During Interviews
You will not get the full, ugly picture on a tour, but you can get close.
Use very specific questions:
- “Can I see a real call schedule from this month for interns on medicine/ICU/OB?”
- “How are nights structured—fixed blocks or scattered?”
- “What does a typical post-call day actually look like? What time do people go home?”
- “What changed about your call schedule in the last 2–3 years based on resident feedback?”
- “On your busiest call rotation, how many true days off does an intern get in 4 weeks?”
And then: watch their faces. If they dodge, joke, or get vague, you have your answer.
For yourself, when looking at a schedule PDF or photo, run this quick mental flow:

| Step | Description |
|---|---|
| Step 1 | Look at 4 week block |
| Step 2 | High risk - circadian chaos |
| Step 3 | Moderate to high risk - fake days off |
| Step 4 | Lower risk - thoughtful design |
| Step 5 | High risk - chronic overwork |
| Step 6 | Nights stable blocks? |
| Step 7 | Post call true off? |
| Step 8 | Reasonable days off count? |
Most of the time, you will know inside of 60 seconds where this program falls.
FAQ (Exactly 6 Questions)
1. Is 24-hour call always a red flag, or can it be done safely?
24-hour call can be done in a relatively safe way if three conditions are met: first, the post-call day is a true off day with no hidden expectations; second, workload overnight is capped or at least realistically matched to staffing so some sleep is actually possible; third, the frequency is reasonable and the calls are spaced sensibly (for example, Q4–Q6 with lighter rotations buffered around them). When those constraints are violated—no real post-call, consistently brutal nights, or calls stacked tightly—24-hour call shifts from “difficult but manageable” to a structural safety hazard.
2. How many nights in a row is “too many” from a circadian standpoint?
Short answer: toggling between days and nights every 1–3 shifts is worse than doing a solid block. From a circadian biology perspective, 5–7 consecutive nights is usually the window where you can at least partially adapt. The real problem is discontinuity: 2 nights on, 2 days off, back to days, then random nights again. That destroys sleep architecture and never allows alignment. A program that insists on rapid-flip schedules because “it spreads the pain” is ignoring well-established fatigue science.
3. What is an acceptable number of true days off in a heavy call month?
In a genuinely heavy inpatient month with call, I start to worry when residents have fewer than 4–5 true days off in 4 weeks—days with no call start, no post-call hangover, and no mandatory teaching or clinic. Getting to 6–8 true days off is far healthier and absolutely achievable if the program is intentional about it. Anything below that lives in a chronic partial-recovery zone, which is where burnout and error rates climb.
4. Are night float systems always better than traditional call?
Not automatically. Night float trades single very long shifts for more frequent moderately long ones. If night float is stable (same hours, same days, same team, in 1–2 week blocks) and buffered with recovery before and after, it is usually superior—residents are less acutely impaired. But if a program sprinkles isolated night shifts throughout the month, or sandwiches short night blocks between full-blast day rotations with no buffer, then night float simply becomes a different flavor of circadian abuse.
5. How can residents push back on unsafe call schedules without retaliation?
You never have a guarantee of zero backlash, but tactically there are smarter ways to do it. Anchor your concerns in patient safety and accreditation standards rather than personal preference. Use specific, recent examples of fatigue-related near-misses. Bring proposals, not just complaints—suggest concrete changes, like clustering nights or adjusting post-call expectations. And go as a group. A unified resident council or class carries more weight and is harder to dismiss than an isolated individual viewed as “not resilient.”
6. For applicants, what is the single biggest call-related red flag during interview season?
The biggest single red flag is inconsistency between what leadership says and what residents quietly describe. If the PD talks about “protecting wellness” and “modern schedules,” but residents pull you aside and say, “The call months are brutal; we just survive them,” believe the residents. Especially if the actual printed schedule you see shows scattered nights, 24s with no real post-call, or 4-week blocks where you can only find 2–3 genuine days off. That mismatch tells you exactly how the program will treat your time, your brain, and ultimately your safety.
Key points: the pattern of call—not just the total hours—predicts burnout and safety risk; unstable circadian design and fake days off are the most telling structural flaws; and a program’s willingness to revise call in response to data and feedback is one of the clearest indicators of whether it is worth your years and your health.






















