The way a program writes its moonlighting rules will tell you more about its finances and staffing than any glossy brochure or smiling program director ever will.
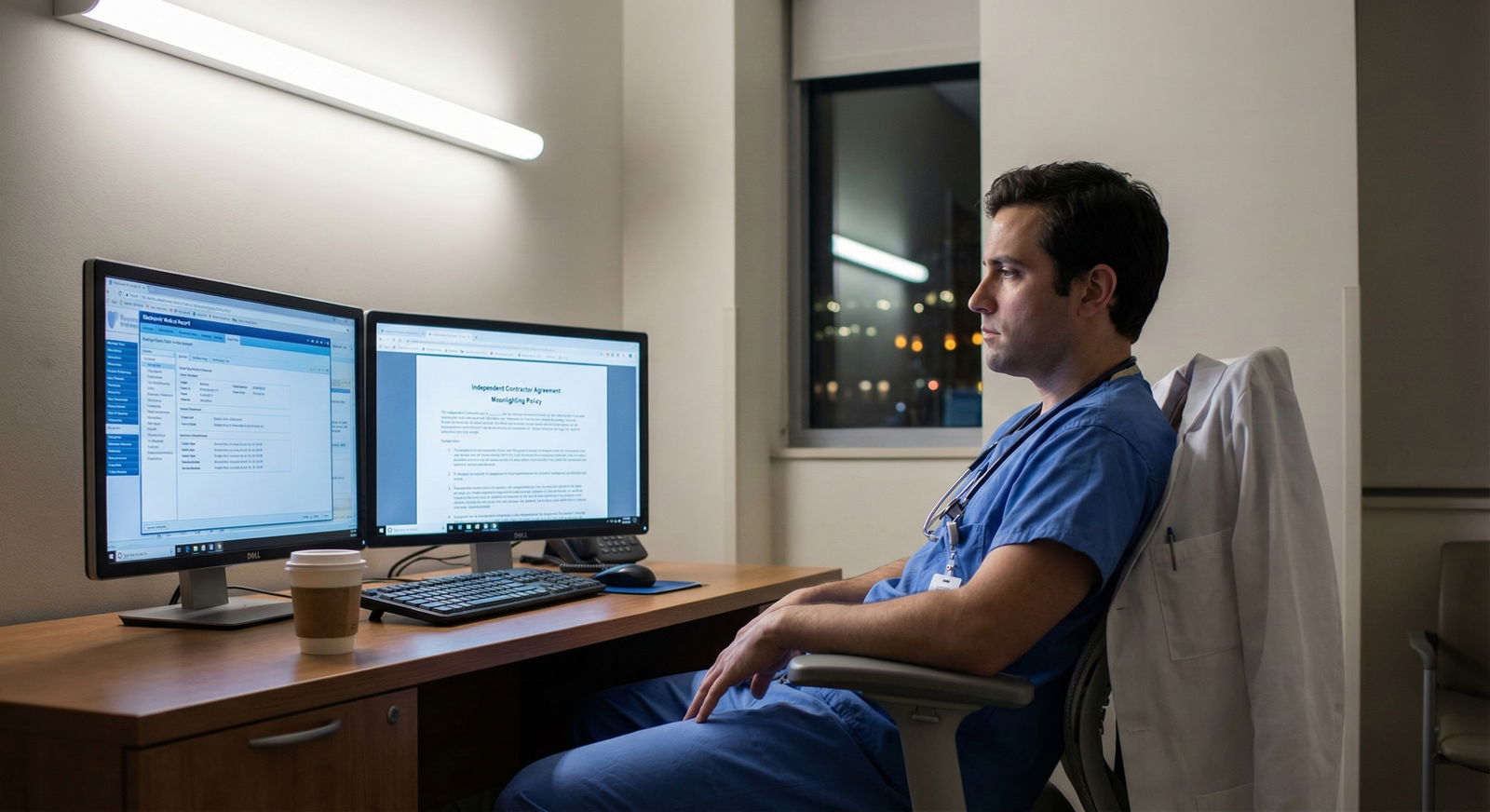
Most residents barely look at moonlighting policies. They skim: “Is it allowed? How much?” Then they move on. That is a mistake. The wording, the structure, and the work types that show up in that policy are some of the clearest red flags that a hospital is short on money, short on staff, or quietly depending on trainees as cheap, flexible labor.
Let me walk you through what I actually look for when I review a program’s moonlighting setup with residents. Because the patterns are remarkably consistent.
1. Start With The Core Question: Why Does This Moonlighting Exist?
Legitimate moonlighting exists to give you optional extra income and experience.
Exploitative moonlighting exists to plug holes in a failing staffing model.
That is the frame. Everything else is just variations on that theme.
There are three basic “why” patterns I see:
True elective moonlighting
Extra ED shifts at a different hospital, inpatient nights at an outside community site, weekend coverage that is clearly above and beyond any resident duty line. Usually:- Not required
- Paid at or above fair-market locums rates for the region
- Cleanly separated from your educational schedule
Blended “we say it is elective, but it really covers our holes” moonlighting
The service cannot function safely without someone in that slot, but the hospital refuses to fund an attending or NP/PA. So they dangle “moonlighting” at weak rates and hope desperate residents take it. You see rules like:- “Moonlighting residents are used to ensure adequate coverage for the service.”
- “Primary coverage for X service is provided by residents and moonlighters.”
Pure desperation coverage
These are the “we lost three hospitalists, the ICU is understaffed, the ED is drowning” setups. You know them when you see them: large numbers of required moonlighting slots, heavy clinical responsibility, and a bad combination of low pay plus high risk.
The point: The more critical the moonlighting role is to basic hospital functioning, the worse the underlying financial or staffing situation usually is.
2. Structural Red Flags In The Written Policy
Stop thinking about the content (“ICU nights,” “floor cross-cover”) for a second. Look at how the policy is structured. The meta is revealing.
a. “Required” Moonlighting Or Quasi-Required Language
If you see anything remotely like:
- “Residents are expected to participate in moonlighting to meet departmental coverage needs.”
- “Each resident is required to complete X moonlighting shifts per year.”
- “Senior residents shall cover Y service on a moonlighting basis…”
That is not moonlighting. That is unfunded mandatory service disguised as “opportunity.”
True moonlighting is:
- Optional
- Resident-initiated or at least resident-selective
- Not tied to promotion, graduation, or evaluation
If your survival to PGY-3 somehow “assumes” you will pick up certain moonlighting blocks, the program is plugging budget holes with your exhaustion.
b. Moonlighting That Occurs Inside Your Own Residency Service
Internal moonlighting is inherently higher-risk for exploitation than external moonlighting.
Examples that are usually fine:
- PGY-3 in IM doing weekend nocturnist shifts at a small outside community hospital, fully licensed, well supervised by phone
- EM resident working at an urgent care across town, separate credentialing
Examples that often smell bad:
- “Senior residents may moonlight as cross-cover for the same medicine floors they cover during regular duty hours.”
- “Night float may be supplemented by moonlighting residents covering additional units.”
If the “moonlighting” is literally you doing the same job, in the same building, sometimes on the same patients, just with a different cost center code in payroll, that is a staffing and financial red flag. The hospital does not want to fund real FTEs.
c. No Explicit Protection Of Education Time
Smart programs spell this out clearly:
- No moonlighting during required conferences
- No moonlighting that overlaps with continuity clinic
- No moonlighting that reduces time on core rotations below ACGME minima
Weak or exploitative programs leave this vague. Or worse, they quietly schedule “moonlighting” during hours they are supposed to be giving you didactics because those hours do not directly generate revenue.
If the policy does not explicitly fence off educational time and clinics from moonlighting, assume the hospital’s financial pressure came first, your training second.
3. Financial Red Flags: Pay, Rates, and Who Actually Benefits
Follow the money. If the economics make no sense for you, they make sense for someone else.
a. Unusually Low Hourly Rates Compared To Market
If a resident is a fully licensed physician in that state, doing independent billable work, they should be compensated somewhere in the neighborhood of a junior attending or locums rate, discounted somewhat for supervision/overhead.
When I start seeing rates like:
- $55–70/hour for high-acuity night coverage in a major metro
- Flat fees that work out to <$60/hr for true admitting or cross-cover roles
- “Stipend” language that is much lower than what local locums firms pay
I know exactly what is happening: the hospital discovered it is cheaper to underpay residents than to hire hospitalists, nocturnists, or additional ED coverage.

| Category | Value |
|---|---|
| Resident Moonlighting | 70 |
| Local Locums | 140 |
| Full Hospitalist | 115 |
If the gap between resident moonlighting pay and local locums pay is massive, you are subsidizing the hospital. Not the other way around.
b. Opaque Billing And “You Get A Fixed Stipend” Models
Another classic pattern: the hospital bills attending-level professional fees on work done by licensed moonlighting residents, pays you a flat low stipend, and keeps the margin.
You may see lines like:
- “Moonlighting residents receive a flat per-shift stipend; billing is handled by the department.”
- “All professional fees are retained by the department to support educational activities.”
Does that necessarily mean theft? No. Does it mean your work is being monetized and you are not seeing any of the upside? Very likely.
Ask directly:
- Who bills for the work I do while moonlighting?
- Do I get any portion of collections or is it flat stipend only?
- How were these stipend rates determined?
Dodging those questions is a financial red flag.
c. “Compulsory But Underpaid” As Part Of A Supposedly Strong Program
There is a special flavor of red flag where the program markets itself as “top tier,” “academic powerhouse,” but the internal moonlighting looks like this:
- PGY-3+ expected to cover open hospitalist nights at $65/hour
- ED residents “strongly encouraged” to staff low-acuity pods at embarrassing rates
- Surgical residents running entire ICU nights on a “moonlighting stipend”
That disconnect between prestige branding and bargain-basement staffing tells you exactly where the hospital’s priorities are: protecting margins, not you.
4. Staffing Red Flags: Where The Holes Actually Are
Now let us move from money to manpower. The actual clinical roles moonlighting fills are not random. They map almost one-to-one to structural problems.
a. Moonlighting On Core Safety-Critical Services
Flag this immediately if you see moonlighting used to cover:
- ICU nights as primary in-house coverage
- Cross-cover for all medicine or surgery inpatients overnight
- ED fast-track or even main ED coverage without full attending presence
- House officer / rapid response codes for the entire hospital
These are services that, in a well-resourced system, are covered by:
- Dedicated hospitalists
- Nocturnists
- Intensivists
- Emergency physicians
- Or at least a robust NP/PA team with clear attending backup
If instead you see: “Senior residents may moonlight as the in-house provider for ICU and cross-cover with attending available by phone,” that is not an “opportunity.” That is a staffing failure.

b. Moonlighting That Functionally Replaces Faculty
Here is the test: if you removed all moonlighting residents tomorrow, what would the hospital have to do?
- Cancel elective surgeries?
- Close an ICU bed tower?
- Put the ED on divert nightly?
- Hire hospitalists urgently at market rates?
If the answer is yes, the moonlighting pool is not “nice to have” backup. It is core staffing. That is a big red flag for financial strain and future burnout.
Programs that are truly stable might use resident moonlighting for:
- Extra elective coverage during flu season
- Giving residents the option to work an outside ED or community hospital
- Filling rare unexpected holes
Programs under pressure use residents as the primary pressure release valve. Eventually, that valve fails – usually in the form of exhausted seniors and quietly unsafe nights.
c. High Volume Of Shifts, Chronic “Open Slots,” and Guilt Trips
Talk to current residents. They will tell you if this is a problem in 30 seconds.
Warning signs in what they say:
- “Yeah, there are almost always open moonlighting shifts; the chiefs keep emailing about them.”
- “We are told that if we do not cover X, the service will be unsafe.”
- “They show the schedule at conference and ask who can pick up more shifts.”
High volume plus chronic begging equals structural understaffing. That will not magically resolve in the next few years unless the hospital dramatically changes its hiring and compensation strategy.
5. Duty Hours And Safety: Where “Moonlighting” Becomes Illegal Work
Moonlighting is allowed only if it fits inside ACGME duty-hour rules. Many programs treat this as a suggestion rather than law. That is not just a red flag; it is a compliance risk that can blow back on you.
a. Policies That Ignore the 80-Hour Rule
The rule is simple: all internal and external moonlighting counts toward your 80-hour limit, averaged over four weeks. It is not optional. It is not “if you self-report.”
If the written policy says things like:
- “External moonlighting does not need to be reported to the program.”
- “Residents are responsible for their own duty-hour compliance while moonlighting; the program does not monitor these hours.”
That is a program signaling they prefer not to know how much you are working because they need the shifts filled. They are incentivizing under-reporting. That is a patient safety and legal risk.
| Policy Phrase | Interpretation |
|---|---|
| All moonlighting must be logged as duty hours | Generally safe, compliant |
| External moonlighting need not be reported | Red flag for under-the-table work |
| Residents self-attest but no auditing | Weak enforcement, risk for overwork |
| Program reviews logs and may restrict shifts | More protective of resident safety |
b. No Clear Cap On Number Of Moonlighting Hours Or Shifts
Reasonable policies will specify something like:
- Maximum X shifts per month
- No moonlighting on post-call days
- No back-to-back overnight moonlighting and regular day shifts
Exploitative environments leave it vague: “Residents are responsible for assuring adequate rest between moonlighting and scheduled duties.”
Translation: If you fall asleep driving home, that is on you. We just needed the bed staffed.
c. Cultural Minimization Of Fatigue
Listen closely during interviews or internal meetings for lines such as:
- “Our residents are warriors; they like to stack shifts and get it done.”
- “If you are efficient, you can easily do your 60–70 hours and still moonlight.”
- “The seniors routinely do a 24-hour call then a moonlighting night the next day – they handle it.”
That culture is the real red flag. Once the norm is “just push harder,” you are one bad night away from a serious medical error or car accident.
6. Licensing, Insurance, and Malpractice: The Quiet Landmines
This section many residents ignore until they almost get burned.
a. Moonlighting Before Full Licensure (Or On Questionable Licenses)
If a program has residents moonlighting:
- Before they have an unrestricted state license
- On a training license not clearly approved for outside or independent work
- With “the attending signing your notes so it is fine”
You are shouldering personal liability with a questionable legal foundation. The hospital is getting revenue and coverage; you are getting risk and a small check.
Before you touch a moonlighting shift, you need clear answers:
- Do I have the correct license for the type of moonlighting described?
- Does my trainee malpractice cover moonlighting, or is there a separate policy?
- Who is the named provider on the billing and malpractice – me, the attending, or the hospitalist group?
If they cannot answer directly, or they say “do not worry, this is how we have always done it,” that is another huge red flag.
b. Malpractice Coverage That Is Thin Or Inconsistent
Hospitals under financial stress sometimes skimp on coverage details.
You might see:
- Claims-made policies with no clear tail coverage discussion
- Moonlighting that technically falls under a separate corporate entity with different coverage limits
- Requirements that you obtain your own malpractice at your expense
If the moonlighting environment is risky (ICU, ED, hospitalist nights) and the malpractice details are vague, you are effectively providing cut-rate specialty coverage without robust legal protection.
7. How To Read Between The Lines During Interviews
You will not see “We use moonlighting to paper over chronic understaffing” written in any brochure. You have to extract it.
a. Targeted Questions That Expose Red Flags
Ask very specific questions. Vague questions get rehearsed answers.
Examples:
- “Are any services functionally dependent on residents or moonlighters for baseline coverage? For example, if no one moonlighted, what would have to close or be on divert?”
- “Over the past year, how often have moonlighting shifts gone unfilled, and what happens when they are unfilled?”
- “What proportion of residents actually moonlight here, and what is the average number of shifts per month?”
- “Has the volume of moonlighting opportunities gone up or down over the last 3–5 years?”
- “What is the hourly rate, and how does that compare with what outside locums get for similar work in the region?”
Pay attention less to the exact numbers and more to hesitation, deflection, or chiefs jumping in to “clarify” in a way that sounds like damage control.
b. Listen To How Senior Residents Talk About It When The PD Is Not In The Room
Every resident-only Q&A quickly reveals the truth if you stop asking “Is moonlighting allowed?” and instead ask “What does it feel like?”
Red-flag phrases:
- “Honestly, it is hard to say no because they really rely on us for those shifts.”
- “I do it because I want to help the team, but it is draining.”
- “The money is not great, but if we did not do it, nights would be unsafe.”
- “They do not force it… but you feel bad if you do not pick up any.”
Healthy phrases:
- “Some people never moonlight; totally fine.”
- “They actually limit how much we can do so we do not burn out.”
- “It is nice extra money, but the hospital would run fine without it.”

| Step | Description |
|---|---|
| Step 1 | Resident considers moonlighting |
| Step 2 | Staffing red flag |
| Step 3 | Likely healthy opportunity |
| Step 4 | Financial red flag |
| Step 5 | High institutional dependence |
| Step 6 | Consider burnout and safety risk |
| Step 7 | Is coverage optional? |
| Step 8 | Fair market pay? |
8. When Moonlighting Rules Predict The Future Of The Program
One final angle: moonlighting patterns are not just a snapshot of current dysfunction. They are a forecast.
a. Rising Moonlighting Volume = Worsening Staffing Over Time
If you hear something like:
- “Five years ago there were just a few ICU moonlighting shifts; now there is cross-cover for three hospitals”
- “We added ED moonlighting last year when attendings left”
- “Hospitalists keep turning over, so residents fill in more now”
That trend line almost always points to:
- Ongoing difficulty recruiting and retaining faculty
- Worsening patient volume without matching hiring
- Financial pressure to keep FTE counts artificially low

| Category | Value |
|---|---|
| Year 1 | 10 |
| Year 2 | 30 |
| Year 3 | 60 |
| Year 4 | 110 |
| Year 5 | 160 |
Do you really want to bet your training (and health) on a hospital trending in that direction?
b. Programs That Proactively Dial Moonlighting Back
The opposite is also revealing. Some programs hit a threshold and say:
- “We noticed residents were doing too much; we raised pay but capped shifts.”
- “The department decided to hire nocturnists instead of leaning on residents.”
- “We created a faculty backup pool so moonlighting is truly optional.”
Those decisions cost money. So if a program is willing to absorb that cost, it tells you they value residents as learners, not just as cheap coverage.
9. Putting It All Together: A Quick Heuristic
You do not need to memorize a checklist. You need a gut filter. Here is mine, bluntly.
If a program’s moonlighting:
- Is required or “expected”
- Primarily covers core inpatient, ICU, or ED safety-critical roles
- Pays substantially below what a locums group would pay
- Has vague or weak duty-hour enforcement
- Uses emotional pressure (“the hospital really needs us”)
- Has grown in volume over the past few years without matching faculty hiring
…then I assume there are serious financial or staffing red flags in the background. I assume burnout is under-reported. I assume patient safety margin is thin at 2 a.m.
On the other hand, if moonlighting:
- Is clearly optional
- Exists mostly at outside sites or clearly non-core services
- Pays reasonably for the region
- Is tightly integrated with duty-hour tracking
- Is something many residents skip without penalty
…then it is probably what it pretends to be: an opportunity, not a crutch.

10. How To Use This As A Resident Or Applicant
Let me be specific about what you should actually do with all this.
Before interviews, read the GME handbook and resident manual if available. Search for:
- “Moonlighting”
- “Additional compensation”
- “Coverage” or “cross-cover”
Highlight:
- Any language about expectations or requirements
- Which services are staffed by moonlighting residents
- How pay is structured
- How duty hours are tracked for those shifts
During interviews, ask pointed questions of:
- The program director (“How dependent is the hospital on resident moonlighting?”)
- The chief residents (“What happens when no one picks up a shift?”)
- The seniors in resident-only sessions (“How does moonlighting actually feel in practice?”)
After the visit, write down:
- The hourly rate or stipend
- The types of shifts (ICU, ED, floor, outside sites)
- The cultural vibe (pressure vs optional)

If that composite picture looks like “this hospital cannot function without residents doing underpaid extra work,” believe it. Your life will be lived inside that reality.
Moonlighting rules are not fine print. They are a diagnostic test for the health of a residency program’s finances, staffing, and ethics. Once you learn how to read them, you will stop being surprised by which programs burn their residents out and which programs quietly protect them.
With that lens in place, you are ready for the next, even more uncomfortable step: looking at how those same financial and staffing pressures are reshaping the future of training itself – from service-heavy “education” models to AI-assisted coverage and beyond. But that is a conversation for another night shift.






















