You’re on a tour. It’s mid-interview season. You’re in the resident workroom, people are chatting, there’s some joking about overnight pages and the cafeteria food. Then an attending steps in and the whole room changes. Quieter. Stiffer. Smiles disappear. Conversation dies instantly or flips to “Yes, Dr. X, absolutely, Dr. X.”
You clock it. And you’re wondering:
Is this normal respect for hierarchy…or a real residency program red flag?
Let’s answer that cleanly.
Short answer: mild tension is normal. Consistent shutdown is a problem.
Let me be direct.
Some “behavior change” when faculty walk in is completely normal. It’s a job. There’s hierarchy. People shift from venting about Epic to discussing the patient in bed 12. Fine.
You should start worrying when:
- The vibe consistently flips from open to fearful the second faculty appear.
- Residents look over their shoulders before answering your questions.
- People literally say, “Let’s talk about this later…when no one’s around.”
- You can’t get a single honest answer about workload, culture, or mistreatment unless you’re physically away from faculty.
That pattern usually means at least one of three things:
- Faculty retaliate when criticized.
- Leadership doesn’t want bad news to reach applicants.
- Residents don’t trust the system to protect them.
If you see that in multiple settings on the same visit? I’d label that a significant red flag.
First, what’s “normal” resident behavior around faculty?
You need a baseline before calling everything toxic.
Expect these “normal” shifts when an attending walks in:
- Jokes get toned down. Nobody is going to complain loudly about the PD’s new note template in front of them.
- Conversation shifts from gossip/venting to patients, logistics, or teaching.
- A senior might step in and “polish” your question if you’re an applicant asking something clumsy in front of the chair.
That’s just workplace professionalism. Nurses do the same thing when their manager walks by.
Normal doesn’t look like fear. It looks like respect plus a bit of self-editing.
Here’s a rough comparison:
| Situation | Normal Program | Concerning Program |
|---|---|---|
| Faculty enters resident room | Tone shifts, still casual conversation | Conversation stops completely |
| Resident gives you an opinion | Honest but measured | Vague, evasive, “I can’t really say” |
| Talking about workload | “It’s busy but doable” with specifics | “We’re…fine” and quick topic change |
| Faculty leaves | Conversation resumes naturally | Residents joke about “now we can talk” |
If what you’re seeing matches the right-hand column repeatedly, yeah, you should worry.
Red flag scenarios: what actually matters vs what doesn’t
Let me break down specific situations you might see on interview day and how to interpret them.
Scenario 1: The “Nervous Panel Lunch”
You’re at the “lunch with residents.” A faculty member or PD is sitting there “to answer questions.” You ask:
“So how is the workload on wards? How many hours are you actually working?”
Resident looks at the PD, then says something like, “We comply with ACGME duty hours” and then stops. You ask about how feedback is handled; they glance again, answer in cliches.
What this suggests:
- Residents have learned there is a “safe script.”
- Faculty are used to controlling the narrative.
- There’s probably a mismatch between what leadership says and what day-to-day life feels like.
Is this automatically catastrophic? Not by itself. But if that canned behavior continues once you’re alone with residents, that’s bad.
Scenario 2: Residents open up only in hidden corners
Later that day, you’re walking between sites. No faculty around. Suddenly the tone flips hard:
- “So…yeah, the hours are rough. It’s more like 80+.”
- “Morale’s been bad since they changed leadership.”
- “Don’t repeat this, but I wouldn’t come here again if I had to redo it.”
Common pattern. I’ve seen this in programs where leadership is disconnected or punitive.
What this suggests:
- Residents don’t feel safe speaking honestly in front of faculty.
- There’s a culture of “keep it quiet for recruitment.”
- Feedback probably doesn’t go anywhere unless it’s heavily filtered.
This is a real red flag. Not fatal in isolation, but strong enough that you should downgrade the program on your list unless there are massive, concrete positives elsewhere.
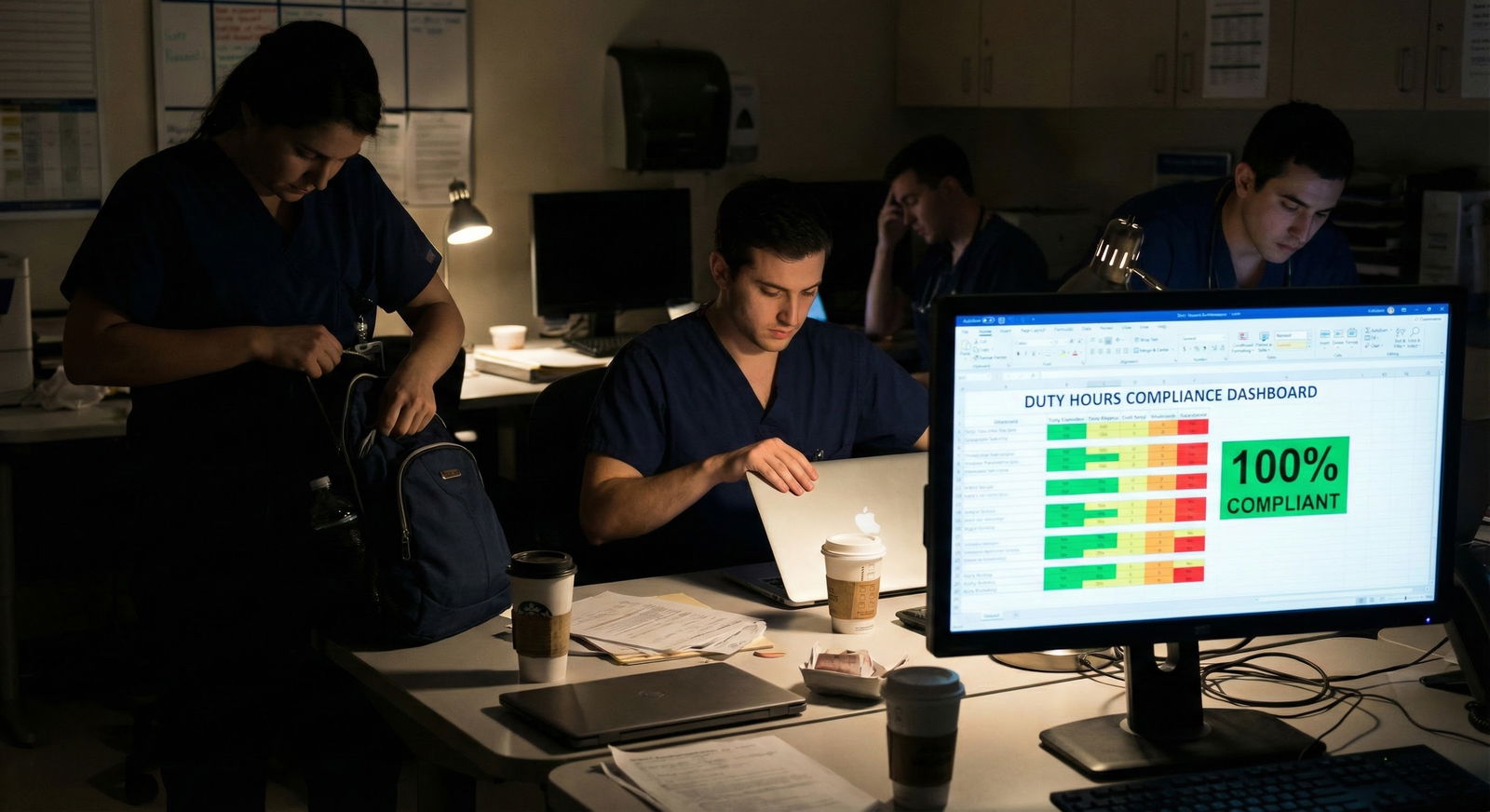
Scenario 3: Attending walks in, everyone goes silent
You’re in the resident workroom talking about call schedules. There’s normal, mildly sarcastic banter. An attending steps in. Silence. People physically turn back to their screens. Whoever was talking cuts mid-sentence.
The attending stays a few minutes to “hang out” but no one really speaks freely. As soon as they step out? Someone mutters, “Okay, where were we?”

| Category | Value |
|---|---|
| Program A (strong culture) | 8 |
| Program B (average) | 5 |
| Program C (red flag) | 2 |
(Think of those values as “how freely people talked to you” on a 1–10 scale.)
What this suggests:
- Faculty are seen as evaluators, not teachers, even off the wards.
- There may have been prior incidents of residents criticized or punished for speaking up.
- The unofficial rule is: “Never let your guard down around attendings.”
I’d call this a major warning sign. A program like this often also struggles with burnout, poor wellness support, and minimal psychological safety.
Scenario 4: Residents speak freely with faculty present
Believe it or not, this exists. You ask about call with the PD at the table and a PGY-3 says:
“Night float is tough. I’m not gonna lie. Census can get heavy. They did add a second resident on Mondays after we complained, which helped a lot.”
Faculty nod, add context instead of shutting it down.
What this suggests:
- Psychological safety.
- Leadership that can tolerate criticism in front of outsiders.
- Residents believe their feedback actually changed something.
Programs like this usually have other green flags: stable leadership, good fellowship/job placement, and residents who stay on as faculty.
How to test whether you’re seeing a red flag or just normal hierarchy
Don’t guess. Probe. There are specific questions and strategies that cut through the surface.
Step 1: Separate spaces, separate answers
Compare what you hear:
- In the resident-only lunch or Zoom Q&A
- On random hallway walks
- When faculty or PDs are sitting there
If answers are drastically different, that’s meaningful.
Ask the same topic in at least two contexts:
- “How’s the culture between residents and attendings?”
- “What happens if you push back on an unsafe plan?”
- “If you had to re-rank this program, would you still put it high?”
Watch for consistency. Honest programs will give similar answers — maybe more toned-down with faculty, but fundamentally the same story.
Step 2: Use “past tense” and third-party questions
Residents feel safer answering about “what used to be” or “what I’ve heard.”
Try these:
- “I saw on Reddit some people said this place used to be malignant. Has that changed?”
- “I’ve heard at some programs residents can’t really disagree with attendings. What happens here if you think the plan is unsafe?”
- “Is there any faculty you’d avoid working with if you could choose?”
If even in resident-only settings the answers are heavily guarded, that’s a sign of deep fear or apathy.
Step 3: Force specificity
Vague = hiding something or not engaged. Specific = usually closer to truth.
Compare:
- Vague: “Yeah the faculty are supportive. We feel listened to.”
- Specific: “On ICU, Dr. Smith is intense but fair. Dr. Lee is amazing — she’ll stay late to teach. We had an issue with overnight handoffs, brought it up, and they changed the process.”
Ask for examples:
- “Can you give an example of a time leadership listened to resident feedback?”
- “When was the last time a resident actually reported mistreatment and something was done?”
- “Who are your favorite attendings to work with and why?”
No examples + body language of discomfort = red flag.
Why a “shut down” culture actually matters for your training
You’re not just trying to avoid feeling awkward on rounds. This stuff hits core parts of your life:
Learning quality
If residents are afraid to speak honestly around faculty, they’re also less likely to:- Admit knowledge gaps
- Say “I don’t know”
- Ask “dumb” questions
That destroys real learning. People fake understanding to survive.
Patient safety
If juniors are scared to challenge attendings, bad plans get executed. I’ve seen interns whisper to each other, “This doesn’t seem right” instead of telling the attending, because that attending is known to blow up at pushback.Wellness and burnout
Programs with fear cultures usually also:- Underreport duty hour violations
- Tolerate mistreatment from certain “untouchable” faculty
- Blame residents for systemic issues
That’s how you end up crying in your car after call, thinking you’re the problem.
Career development
In a fear-based environment, you’ll hesitate to be honest on evaluations and in meetings. Networking and mentorship suffer because every interaction feels like a high-stakes evaluation.
So yes, whether residents talk freely around faculty is not a trivial cosmetic detail. It’s a proxy for deeper structural issues.
How to factor this into your rank list (without overreacting)
You’re not going to find a program where everyone is 100% relaxed around leadership 24/7. That’s fantasy.
Here’s how I’d weigh this realistically.

| Category | Value |
|---|---|
| Clinical training | 30 |
| Location/personal life | 25 |
| Culture/psychological safety | 25 |
| Fellowship/jobs | 10 |
| Research/resources | 10 |
Culture and psychological safety are a big chunk. Residents shutting down around faculty is one component of that.
Use this framework:
Is this a one-off or a pattern?
If you only noticed it once, and everything else felt great, I’d note it but not tank the program.Do residents talk freely when faculty are not there?
- If yes, but they get stiffer with attendings: normal hierarchy.
- If no, even without leadership: systemic fear. Big problem.
Does the program have offsetting strengths you actually care about?
Elite fellowship outcomes and great research don’t erase a toxic culture — unless you consciously decide to tolerate that for a specific career goal. Be honest with yourself.Compare across several interviews
After 5–10 programs, you’ll see a pattern. Some places feel tense. Some don’t. Rank accordingly.
If two programs are similar clinically, and in one the residents are laughing and teasing attendings in front of you, and in the other they go dead silent when faculty show up? I’d pick the first one every time.
Quick tools you can actually use on interview day
Here are a few practical moves you can steal.
1. The “same question, two rooms” trick
Ask, “How responsive is leadership to resident feedback?”
- At the official session with the PD
- At the resident-only hangout
If the tone flips from glowing to “euhhh, mixed,” you’ve learned a lot.
2. The “would you come here again?” test
Ask each resident separately if you can:
“If you had to do the match again, would you still rank this program where you did?”
You’re not just listening for “yes” or “no.” You’re watching how fast and how comfortably the answer comes out. Hesitation says more than words.
3. Watch body language when faculty enter
This is underrated. Pay attention to:
- Eye contact: do residents keep talking to you, or instantly look down?
- Posture: relaxed vs rigid.
- Conversations: do they resume after faculty leave, or do people scatter?
One of the most honest reads of a program is that 5 seconds right after a PD walks into and out of a room.
FAQ: Residents Not Talking Freely Around Faculty
1. Is it always a bad sign if residents act more formal when faculty are around?
No. Some increased formality is normal — it’s still a workplace. People naturally clean up jokes and venting when a supervisor walks in. You should worry when conversation completely dies or flips into scripted answers, and that same tightness persists even when leadership isn’t present.
2. What if the program is very prestigious but the vibe feels fearful around attendings?
You can absolutely train at a “top” place and be miserable. Prestige does not fix a toxic culture. If residents clearly don’t feel safe speaking openly with or around faculty, you’re gambling your sanity for a brand name. Sometimes that trade is worth it for specific goals; most of the time, it’s not.
3. How do I get honest answers if residents seem guarded with faculty nearby?
You wait them out and move locations. Walk with them between sessions. Stay for the optional happy hour or post-interview hangout. Ask the same questions in faculty-free spaces. If even then you’re still getting vague, canned answers, assume the worst and move the program down.
4. Could it just be that the residents are introverted or tired, not scared?
Sure, residents are exhausted. But tired looks different from scared. Tired residents will still answer your questions honestly, just with less energy. Scared residents glance at doors, give non-answers, change the subject when faculty are mentioned, or explicitly say “we shouldn’t talk about that here.”
5. Bottom line: if residents shut down around faculty, should I cross the program off my list?
Not automatically, but I’d treat it as a serious warning sign. Combine it with everything else you’ve seen: duty hours, morale, how they talk about leadership, how often alumni stay as faculty. If multiple signals point to fear and lack of psychological safety, move that program way down unless you have an extremely compelling reason to keep it high.
Key takeaways:
- A little formality around attendings is normal; consistent shutdown and scripted answers are not.
- Use resident-only spaces and repeat questions to see if the story changes — that discrepancy is your best data point.
- Choose programs where people can tell the truth in front of leadership; that’s what protects your learning, your patients, and your mental health.






















