The worst way to find out a program has red flags is after you match there.
The core move: stop asking “Are there red flags?” entirely
You should almost never ask, “So… any red flags I should know about?”
That question does three things you do not want:
- Puts residents on the spot to bad-mouth their employer.
- Sounds naïve. Like you did not do basic homework.
- Forces awkward silence or canned PR answers.
Instead, your job is to:
- Ask neutral, specific questions that expose problems indirectly.
- Change how you ask (setting, phrasing, tone) so residents feel safe.
- Watch what people do not say as much as what they do.
Here is the framework I’d use if I were going through interviews again.
Step 1: Set up the right conditions before you ask anything
You cannot get honest answers if:
- The PD is in the room.
- A chief resident is hovering.
- Everyone is in a big formal Q&A where one brown-noser keeps praising everything.
You want:
- Small groups.
- No attendings.
- Ideally late in the day when people are tired and less filtered.
On interview day, prioritize:
- Resident-only lunch/dinner.
- The social the night before (this is where the real talk happens).
- Pulling one resident aside for a hallway / walk-between-sessions chat.
If there’s a pre- or post-interview social on Zoom, stay to the end. The tone always changes in the final 15–20 minutes when admin people log off and only residents remain.
Step 2: Use “code” questions that surface red flags
You are not asking, “Is this a toxic program?” You are asking questions that make toxicity obvious if it exists.
Here are the strongest categories and exact phrases you can borrow.

| Category | Value |
|---|---|
| Workload | 85 |
| Culture | 75 |
| Education | 65 |
| Support | 60 |
| Safety | 50 |
1. Workload and coverage (the fastest way to detect misery)
Ask:
- “What does a bad call night look like here, and how often does that happen?”
- “On your busiest rotations, what does a typical week of hours look like?”
- “When someone is out sick, how is coverage handled?”
Red flag clues:
- They laugh, look at each other, then say “It depends” and change the subject.
- “Honestly, you just do what you have to do. We make it work.”
- “Sick call? We don’t really have a formal system… we just pick up the slack.”
Green-ish signals:
- Specific numbers. “On ICU we’re ~70–80 hours, most others around 55–60.”
- “We have a jeopardy system; it gets used and people don’t get punished for being sick.”
2. Culture and how people talk to each other
Ask:
- “How would you describe how attendings give feedback here?”
- “If a resident makes a mistake, what usually happens next?”
- “Can you think of a resident who struggled—what kind of support did they get?”
Red flag clues:
- “It’s a very self-directed environment.” (Often code for zero support.)
- “If you’re strong you’ll be fine.” (They only want workhorses.)
- Stories where errors led to humiliation, yelling, or threats.
Healthier answers:
- “We have formal feedback, but a lot of us just grab attendings after rounds to ask how we’re doing.”
- Concrete example of a struggling resident who was remediated and graduated, not quietly pushed out.
3. Education vs. cheap labor
Ask:
- “How often does teaching get canceled because of clinical demands?”
- “Who usually runs teaching—attendings, fellows, residents?”
- “Do you feel like you’re primarily here to learn or to move volume?”
Red flag clues:
- “Morning report is on the schedule… it happens when census is manageable.” (Translation: rarely.)
- “We’re a very busy hospital; most of the learning is on the fly.”
- No protected time. No one mentions a culture of “we stop to teach.”
Better answers:
- “We actually leave the floor for noon conference, pages go to a jeopardy resident or the attending.”
- “Sometimes it gets cut short on rough days, but it happens the majority of the time.”
4. Resident retention and program stability
Ask:
- “Have many residents left the program or switched out in the last few years?”
- “Have there been any big leadership changes recently? How did that impact you all?”
- “Do most people stay for fellowship here or leave happy?”
Red flag clues:
- Visible discomfort. “Yeah, there were… a couple situations… but it’s fine now.”
- High resident turnover. Multiple people leaving, PGY-2s not matching into PGY-3 spots.
- Frequent leadership churn with vague explanations.
Good signs:
- They can name one or two departures with clear, non-toxic reasons (family move, partner, specialty switch).
- Leadership changes described with specifics and residents feeling heard about it.
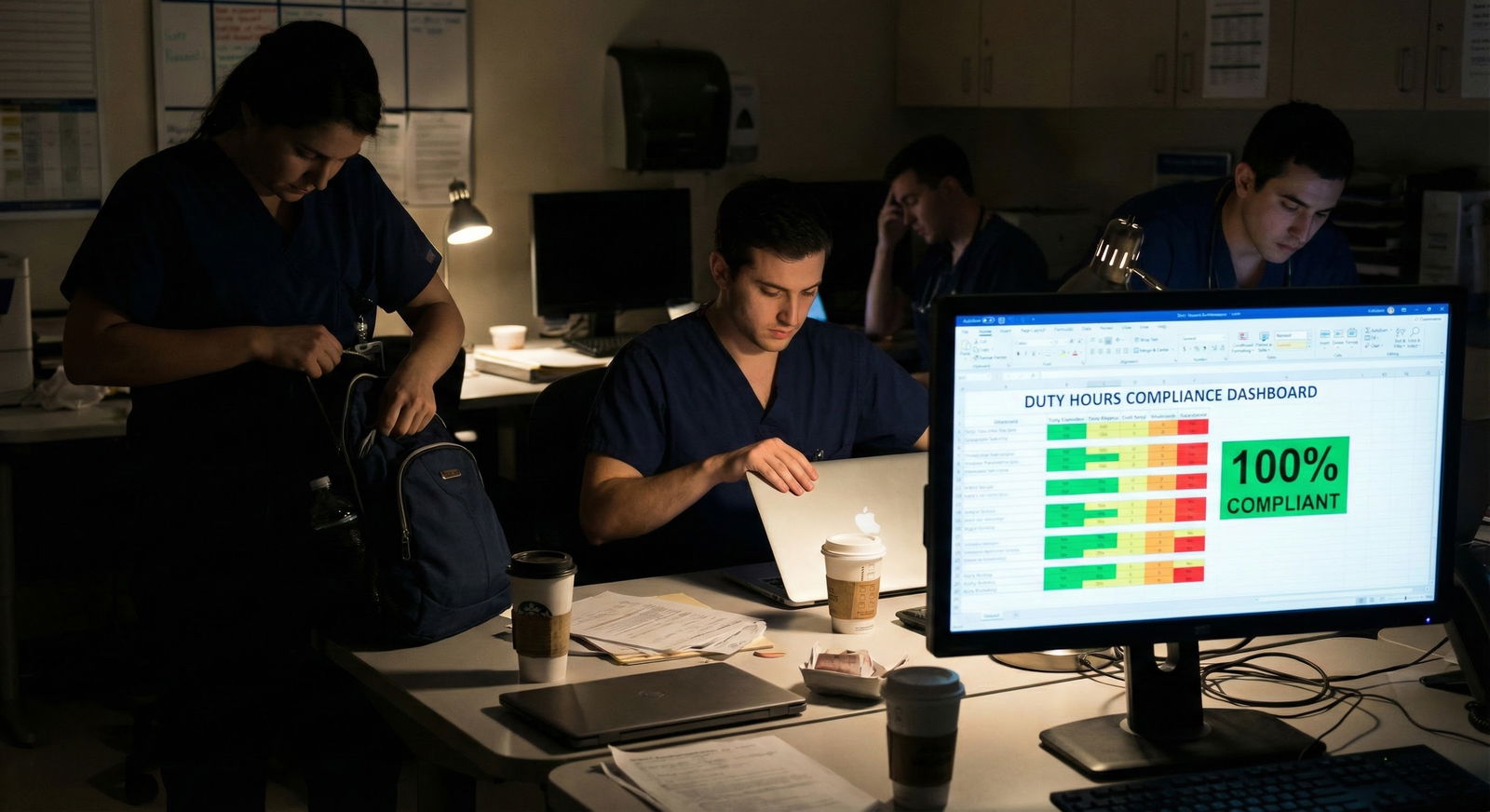
5. Safety, duty hours, and pushing limits
Ask:
- “Do you usually get out close to post-call time, or does work often spill over?”
- “How does the program respond if duty hours are getting violated?”
- “Have you ever felt pressured to come in sick or stay longer than is safe?”
Red flag clues:
- “We definitely document 80 hours.” (That word choice matters.)
- Jokes about “creative charting” of hours.
- “If you’re efficient, it’s fine.” (Blaming the resident, not the system.)
You want to hear:
- Stories of when people reported problems and something concrete changed.
- “Our chiefs track hours pretty aggressively and go to bat for us.”
Step 3: Make residents feel safe answering you honestly
Your questions can be perfect and still fail if you sound like you’re collecting dirt for an expose.
Three tactics:
Normalize the question upfront.
“Every program has things that are great and things that are frustrating. I’m trying to figure out where the pain points are so I can see where I’d fit. For you all, what are the 1–2 things you’d change if you could?”Show you’re not naïve.
“I know every residency is hard. I’m not afraid of work. I just don’t want to end up somewhere unsafe or where residents feel disposable.”Ask for their personal experience, not general gossip.
“What’s been the hardest part of training for you here?”
“What do you vent about most when you’re post-call?”
People are much more willing to be honest if:
- You’ve already shown you understand medicine is tough.
- You’re clearly not going to blast them on social media.
- You ask like a colleague, not an undercover investigator.
Step 4: Use triangulation, not one-off comments
Never anchor your rank list on one salty PGY-1.
Your goal is pattern recognition:
- Do multiple residents independently say the same thing?
- Do interns and seniors describe the culture similarly?
- Do answers match what you see on rounds, in the lounge, in body language?
| Program Size | Minimum Residents To Sample | What You’re Aiming For |
|---|---|---|
| ≤ 20 total | 3–4 | At least 1 intern, 1 senior |
| 21–40 | 4–6 | Mix of PGY levels, 1 chief |
| 41–60 | 6–8 | Different rotations/services |
| > 60 | 8–10 | Broad slice of the program |
If:
- One person is bitter and everyone else seems grounded → log it, but don’t overreact.
- Everyone dodges the same topic → that’s the red flag.
- People light up about some aspects and wince at others → that’s normal and actually reassuring. Nuance = honesty.
Step 5: Phrases that are “polite red flag detectors”
Here are some script-level lines that work well and don’t feel awkward.
- “What surprised you most after you started here—good or bad?”
- “If your best friend were ranking this program, what would you tell them to think twice about?”
- “What’s one thing applicants usually miss about this place, that they only understand after starting?”
- “How does the program handle it when residents push back or have concerns?”
Watch for:
- Overly polished answers that sound like the website.
- Residents constantly glancing at each other before speaking.
- Jokes that keep recurring: “Hope you like nights,” “Say goodbye to your weekends,” “We live here.”
One resident joking about suffering is just residency. A whole group of them defaulting to burnout humor is something else.
Step 6: Follow-up emails and DMs without being weird
If you need more info after the interview day, you can reach out. Just do it like a normal human.
Subject line ideas:
- “Quick follow-up about [Program Name]?”
- “Thanks again – one more candid question?”
Body example:
Hi [Name],
Thanks again for talking with us on interview day – your comments about [specific rotation or aspect] really stuck with me.
I’m seriously considering ranking [Program] highly and want to make sure I have a realistic sense of training there. If you’re comfortable, I’d love to ask a more candid question or two about what’s been hardest for you and what you’d change if you could. I completely understand if you’d rather not put that in writing.
Thanks again either way,
[Your Name]
Key points:
- Anchor to something they already said.
- Explicitly give them permission to not answer.
- Avoid asking for a yes/no “Is this place toxic?” judgment.
Often they’ll say, “I’d prefer to answer this by phone,” which is your signal they’re going to be honest.
Step 7: Recognize the “too perfect” program
One more thing nobody tells you: a place where no one can name a single problem is almost always hiding something.
Healthy programs have:
- Annoyances residents can name easily.
- Areas they’re actively trying to fix.
- Trade-offs. “Loads of autonomy but the documentation is brutal.” “Great teaching, call is heavy.”
What you do not want:
- “Honestly, everything is great here.” (From everyone.)
- Leadership always in the room when residents talk.
- Residents using vague corporate language: “continuous improvement,” “transformational leadership,” but no concrete examples.
You’re not looking for a perfect program. You’re looking for one where the problems are:
- Visible.
- Acknowledged.
- Being worked on.
If residents can describe that dynamic, awkwardness disappears. You’re just two doctors talking about a workplace.

| Step | Description |
|---|---|
| Step 1 | Interview Day |
| Step 2 | Find resident only time |
| Step 3 | Ask neutral specific questions |
| Step 4 | Watch verbal and nonverbal cues |
| Step 5 | Follow up after visit |
| Step 6 | Log minor issues only |
| Step 7 | Adjust rank list |
| Step 8 | Consistent concerns? |
FAQ: Discreet Questions About Residency Program Red Flags
1. Is it ever okay to directly ask, “Are there any red flags?”
Rarely. It puts residents in a risky spot and usually shuts down honesty. If you insist on being direct, soften it: “Every program has weaknesses. What would you say are this program’s biggest growing edges right now?” That’s about as blunt as you should get.
2. How do I read between the lines if everyone is being diplomatic?
Look for what they won’t talk about. If you ask three workload questions and get zero specifics, assume workload is rough. If people gush about fellowship matches but never mention how residents are treated day to day, that’s a clue. Silence around one domain is itself data.
3. What if I only talk to happy residents—can I trust that?
Partly. If they can name real downsides and still say they’d choose the program again, that’s gold. If they’re only positive, with no specific frustrations, be cautious. Try to find a different PGY level or a resident from another service (ICU vs clinic, for example) to compare.
4. How do I ask about burnout without sounding accusatory?
Ask about sustainability and support. “What helps you avoid burnout here?” or “What do people do when they start feeling overwhelmed—does the program step in at all?” Their answer will tell you both whether burnout is common and whether the system cares.
5. Are socials and dinners really that important for honest answers?
Yes. Residents are dramatically more candid away from conference rooms and PDs. I’ve heard things at a pre-interview bar meetup that would never be said in a noon Q&A. If you’re skipping socials, you’re basically agreeing to see the brochure version of the program.
6. How much weight should I give to one really negative resident?
Treat it as a signal, not proof. Ask yourself:
- Do others hint at similar issues?
- Does this align with the vibe you saw on the units?
If it’s just one outlier, note it but don’t let it dominate your rank list. If three different people, on different days, tell variations of the same story—that’s when you should move the program down.
Open a notes doc right now and build a short list of 8–10 specific questions from this article that feel natural to you—then bring that list to every interview day and actually use it.






















