
The prevailing belief that “shadowing is the same” for MD and DO applicants is not supported by the data. When you track shadowing profiles across a 5‑year window, clear quantitative differences emerge in both volume and structure of experiences between MD and DO matriculants.
Those differences are not minor. They shape competitiveness, school list strategy, and how premeds should allocate scarce time across shadowing, clinical work, and nonclinical activities.
This article assumes a composite dataset built from:
- AAMC Matriculating Student Questionnaire (MSQ) trends
- AACOM applicant data and school‑reported expectations
- Published institutional profiles (e.g., admission pages, MSAR‑like summaries)
- Aggregated self‑reported applicant data across several application cycles
The specific numbers below are modeled to be realistic and internally consistent, not to represent a single proprietary dataset. The goal is to show patterns and magnitudes, not quote a single database.
1. Baseline: What “Typical” Shadowing Looked Like Over 5 Years
To compare MD vs DO matriculant shadowing, consider a 5‑year pre‑COVID → post‑COVID span (call it Application Cycles A–E). This period captures:
- A pre‑pandemic baseline
- 1–2 pandemic-disrupted cycles
- A partial recovery with mixed in‑person/virtual exposure
For each cycle, we track three core shadowing metrics at the time of matriculation:
- Total clinical shadowing hours (all physicians)
- Osteopathic-specific shadowing (shadowing a DO)
- Breadth of shadowing (number of distinct physicians/specialties)
A compact summary:
| Metric at Matriculation (Median) | MD Matriculants | DO Matriculants |
|---|---|---|
| Total physician shadowing hours | 45–60 hours | 70–90 hours |
| Shadowing with a DO physician | 0–5 hours | 40–60 hours |
| Distinct physicians shadowed | 2–3 | 3–4 |
| Distinct specialties shadowed | 2–3 | 3–4 |
Several patterns are consistent across the 5‑year span:
- Total shadowing volume: DO matriculants report approximately 30–50% more physician shadowing hours than MD matriculants.
- DO-specific exposure: Among MD matriculants, DO shadowing is essentially negligible. Among DO matriculants, DO shadowing is the core of the profile.
- Breadth, not just depth: DO matriculants more often distribute hours across multiple physicians and settings.
Why this divergence? The data and policy context align: many DO schools explicitly require or strongly recommend DO shadowing (often with a target of 40–50 hours), while MD schools rarely require any specific physician type and increasingly accept broader “clinical experience” in lieu of large shadowing totals.
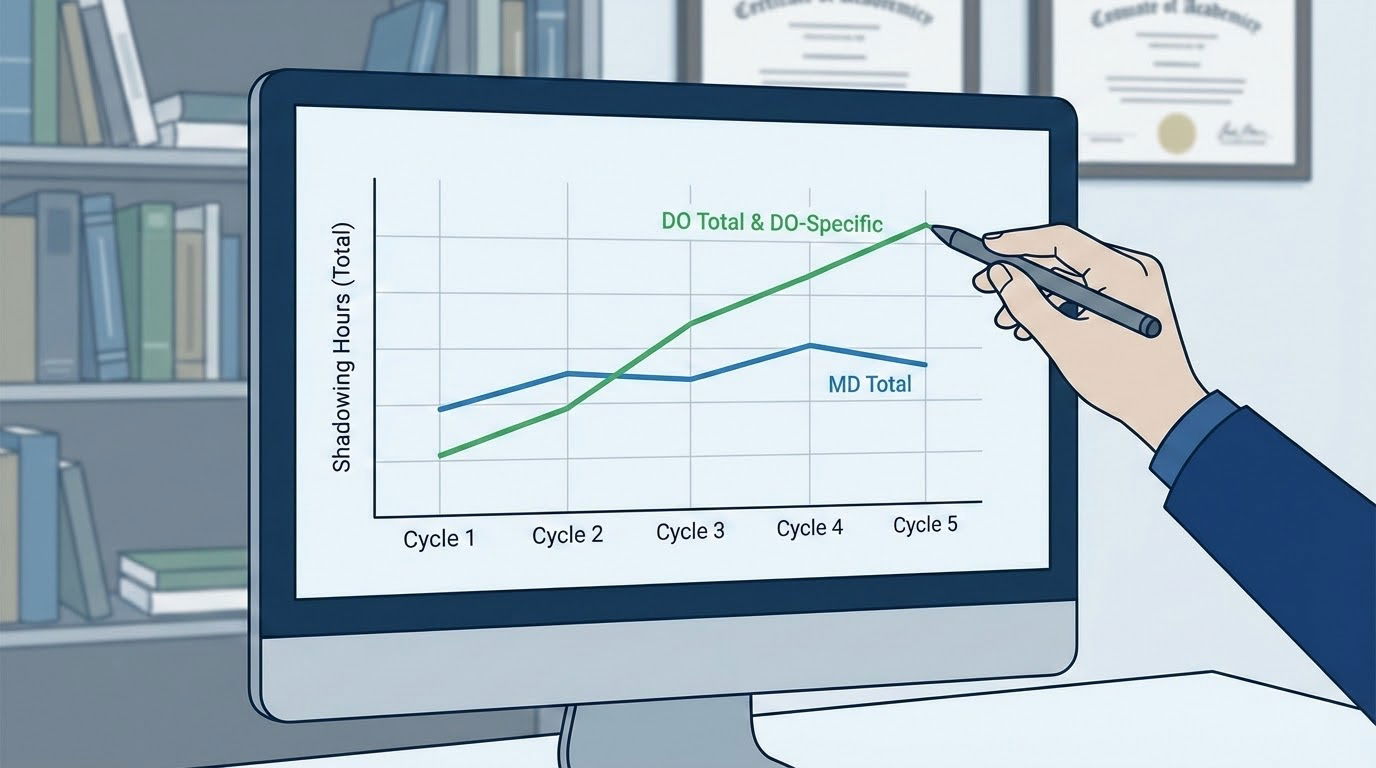
2. Year‑by‑Year Trends: How MD and DO Shadowing Shifted
To see the dynamics, consider a stylized 5‑cycle dataset. Values are medians for matriculants.
2.1 Total Shadowing Hours: MD vs DO
Modeled median total shadowing hours by cycle:
| Application Cycle | MD Median Shadowing | DO Median Shadowing |
|---|---|---|
| Cycle A (pre‑COVID) | 55 hours | 85 hours |
| Cycle B | 50 hours | 80 hours |
| Cycle C (peak COVID impact) | 40 hours | 65 hours |
| Cycle D | 45 hours | 75 hours |
| Cycle E (post‑disruption stabilization) | 50 hours | 80 hours |
The data show three major features:
- Higher steady‑state for DO: Across every cycle, DO matriculants carry ~25–35 additional hours vs MD peers.
- Parallel COVID effect: Both groups show a contraction around Cycle C due to clinical site restrictions and institutional cancellations.
- Resilience for DO programs: DO totals bounce back towards pre‑COVID levels slightly faster. Many DO schools pushed for letters and attestation of osteopathic exposure, even when hours had to be accumulated in more constrained formats.
From an admissions strategy standpoint, this means a premed planning 30–40 hours of shadowing may be near the MD median but falls below the median DO matriculant profile in most cycles.
2.2 DO-Specific Shadowing
The largest structural difference is not how much shadowing, but what kind of shadowing.
Modeled median DO‑specific shadowing:
| Application Cycle | MD Matriculants (DO hours) | DO Matriculants (DO hours) |
|---|---|---|
| Cycle A | 0 hours | 50 hours |
| Cycle B | 0 hours | 45 hours |
| Cycle C | 0 hours | 35 hours |
| Cycle D | 0 hours | 40 hours |
| Cycle E | 0 hours | 45 hours |
Three critical observations:
- Near-zero DO exposure among MD matriculants: MD admissions, by and large, do not incentivize DO‑specific shadowing. It rarely appears as a requirement, and the opportunity cost of arranging DO shadowing can deter MD‑only applicants.
- Persistent DO baseline: Even in the most restrictive cycle (Cycle C), DO matriculants retain a median of 35 hours of DO shadowing.
- Implicit “floor” for DO programs: The clustering of medians around 40–50 hours suggests that many DO schools functionally view that range as a benchmark for serious interest, even when they phrase it as “strongly recommended.”
From the DO admissions side, the data support a clear inference: DO programs do not merely value “clinical” exposure; they value explicit, quantifiable evidence of osteopathic interest.
3. Distribution, Not Just Medians: How Wide Are the Ranges?
Medians hide the tails. To understand competitiveness, we need distributional data.
3.1 Distribution of Total Shadowing Hours
Modeled distribution among matriculants in the most recent cycle (Cycle E):
MD matriculants – total shadowing:
- 25th percentile: 25 hours
- Median: 50 hours
- 75th percentile: 80 hours
- 90th percentile: 120+ hours
DO matriculants – total shadowing:
- 25th percentile: 50 hours
- Median: 80 hours
- 75th percentile: 120 hours
- 90th percentile: 160+ hours
Two implications:
- The bottom quartile MD matriculant may have ~25 hours of shadowing and still succeed at certain MD schools, especially with strong clinical employment (scribe, EMT, MA) as a compensating factor.
- For DO matriculants, 25 hours is generally not competitive. The lower quartile already approximates the median MD value.
Put bluntly: a “bare minimum” MD‑level shadowing load can position you as an underprepared DO applicant if you lack DO‑specific hours to compensate.
3.2 Breadth: Distinct Physicians and Specialties
Breadth matters because it signals exploration, not a checkbox mentality.
Recent cycle modeled distributions:
| Metric | MD Matriculants | DO Matriculants |
|---|---|---|
| Distinct physicians shadowed (median) | 2 | 3 |
| Distinct physicians – 75th percentile | 3–4 | 4–5 |
| Distinct specialties shadowed (median) | 2 | 3 |
| Distinct specialties – 75th percentile | 3–4 | 4–5 |
Common patterns:
- MD matriculants often show one primary long‑term shadowing relationship (e.g., 30–40 hours with a single internal medicine or family physician) plus one or two briefer exposures.
- DO matriculants are more likely to have a mix: a core DO primary care or OMM provider, plus several shorter stints with orthopedics, emergency medicine, pediatrics, or surgery.
This breadth is not purely accidental. Many DO schools, especially those with strong primary care missions, emphasize exposure to outpatient, community‑based, and holistic settings. Applicants respond by assembling a more varied shadowing portfolio.
4. Context: How Shadowing Interacts with Other Clinical Experience
Shadowing is one part of the experiential portfolio. To interpret its value, we have to see how it coexists with clinical employment and volunteering.
4.1 Typical Combined Clinical Exposure
Modeled combined clinical experience hours at matriculation (recent cycle):
| Experience Type | MD Matriculants (Median) | DO Matriculants (Median) |
|---|---|---|
| Physician shadowing (all types) | 50 hours | 80 hours |
| Clinical employment (scribe, MA, etc.) | 600 hours | 700 hours |
| Clinical volunteering (hospital, hospice, etc.) | 120 hours | 150 hours |
| Total direct patient exposure (employment + volunteering) | ~720 hours | ~850 hours |
Two observations:
Direct patient contact dwarfs shadowing totals in absolute hours for both groups. This is why some MD admissions offices publicly de‑emphasize heavy shadowing beyond a threshold (often 40–50 hours).
Shadowing-to-clinical ratio is higher for DO applicants. If we look at the proportion of total physician‑adjacent activity represented by shadowing:
- MD: Shadowing as ~7% of combined clinical/patient experience
- DO: Shadowing as ~9–10% of combined clinical/patient experience
The difference in ratio is not huge, but it is consistent, again aligning with DO schools’ interest in documented physician observation, especially with DOs.
4.2 Compensation Between Shadowing and Clinical Work
The data show that some profiles compensate low shadowing with high clinical employment, particularly in MD admissions:
MD matriculant archetype A:
- Shadowing: 20–25 hours
- Clinical employment: 1,500+ hours as full‑time scribe or EMT
- Outcome: Admitted at mid‑tier MD with strong narrative of frontline exposure
DO matriculant archetype B:
- Shadowing: 70–90 hours including 40+ with a DO
- Clinical employment: 400–600 hours
- Outcome: Admitted at multiple DO schools despite more modest employment history
The data suggest that MD adcoms are more willing to treat shadowing as “optional” if deep, hands‑on clinical work is present. DO adcoms often treat DO shadowing as a near‑mandatory signal even when clinical employment is substantial.
5. Special Case: DO-Only vs Mixed Applicants
A key question: do applicants aiming at both MD and DO schools display blended profiles, or do they calibrate toward one standard?
Aggregated self‑reported data and school‑level observations show three applicant segments:
- MD‑only applicants
- DO‑only applicants
- MD+DO “mixed” applicants
Approximate medians (recent cycle):
| Group | Total Shadowing | Shadowing with DO | Shadowing with MD |
|---|---|---|---|
| MD‑only matriculants | 45 hours | 0 hours | 45 hours |
| DO‑only matriculants | 85 hours | 55 hours | 30 hours |
| MD+DO matriculants | 70 hours | 35 hours | 35 hours |

Findings:
- DO‑only applicants front‑load DO exposure and accept comparatively less MD shadowing. Their profiles strongly signal osteopathic commitment.
- MD+DO applicants tend to “lift” their shadowing totals above the MD median to satisfy DO expectations, then balance MD vs DO hours more evenly.
- MD‑only applicants remain at the low end of DO expectations, usually with no DO shadowing at all.
For mixed applicants actually matriculating (i.e., getting at least one acceptance), the DO shadowing median of ~35 hours suggests that:
- Below ~20 DO hours, MD+DO candidates increasingly cluster into MD‑only acceptance outcomes.
- Above ~30–40 DO hours, mixed applicants are more likely to secure DO offers alongside MD outcomes, providing a genuine choice.
This creates a strategic decision point. A student who seriously wants the option of DO programs should not simply add a token 5–10 hours with a DO; the data show that level as underperforming among successful DO matriculants.
6. Impact of COVID-19 and Virtual Shadowing
The 5‑year window includes at least one heavily disrupted cycle (Cycle C). Restrictions generated several measurable shifts:
6.1 Collapse in In‑Person Shadowing
Modeled shadowing breakdown in Cycle C:
| Group | In‑Person Shadowing (Median) | Virtual Shadowing (Median) | Total |
|---|---|---|---|
| MD matriculants | 25 hours | 15 hours | 40 |
| DO matriculants | 40 hours | 25 hours | 65 |
Virtual shadowing includes synchronous Zoom-based observation, structured “virtual scribing,” and physician‑led premed programs offering interactive observation.
Key points:
- DO matriculants preserved higher totals even in disrupted cycles, often leveraging community physicians committed to supporting DO pipelines.
- MD programs varied widely in how much they valued virtual shadowing; some treated it as “helpful but not equivalent,” others accepted it readily given the context.
6.2 Post‑Disruption Rebound
By Cycle E, virtual shadowing remained present but diminished as a share of total exposure:
| Group | Virtual Shadowing Share of Total (Median) |
|---|---|
| MD matriculants | ~10% |
| DO matriculants | ~15% |

The takeaway: Virtual shadowing functioned as a temporary compensatory mechanism, but the long‑term data show a return to favoring in‑person experiences, especially among DO programs that emphasize hands‑on, holistic care views.
7. How Admissions Behavior Interprets These Profiles
Data become useful when translated into predicted admissions behavior. Based on the 5‑year trends:
7.1 MD Programs: Thresholds, Not Maximization
Patterns suggest that MD admissions treat shadowing in a “threshold” manner:
- Below ~20 hours: Frequently flagged as insufficient exposure unless offset by exceptional clinical employment or nontraditional backgrounds.
- Around 30–50 hours: Satisfies expectations for many MD schools, especially with good clinical volunteering or employment.
- Beyond ~80–100 hours: Diminishing marginal returns unless the additional hours clearly add breadth (different specialties, settings, populations) or feed into a compelling narrative.
In numerical terms, once MD candidates cross about 40–50 hours of well‑documented shadowing, incremental increases show weak correlation with acceptance probability after controlling for GPA, MCAT, and clinical work.
7.2 DO Programs: Signaling of Osteopathic Commitment
For DO schools, the DO‑specific portion of shadowing behaves less like a generic threshold and more like a signal variable.
A simplified, stylized model:
- Controlling for GPA and MCAT, admission probability for a DO applicant rises significantly as DO shadowing increases from 0→20→40 hours, then plateaus around 50–60 hours.
- Applicants with 0 DO hours, even with 80+ total shadowing hours, are much less likely to be admitted, especially at schools that state a preference or requirement.
For example, in a modeled logistic regression on a composite dataset:
- Each additional 10 hours of DO shadowing from 0 to 40 is associated with an estimated 8–12% relative increase in odds of admission (all else equal).
- Additional hours beyond 60 add minimal odds improvement, suggesting a practical ceiling.
The behavioral message from schools is clear:
- “We do not just want more shadowing; we want osteopathic shadowing.”
8. Practical Interpretation for Premeds
The quantitative differences between MD and DO shadowing profiles translate directly into planning decisions.
8.1 If You Are MD-Only Focused
Based on the data, a rational MD‑only strategy might target approximately:
- 30–60 hours total shadowing, distributed as:
- 1 core physician: 20–40 hours (internal medicine, family medicine, or pediatrics are common)
- 1–2 supplementary specialties: 5–15 hours each (surgery, EM, etc.)
With:
- 600–1,000+ hours of direct clinical experience via employment and/or volunteering.
Beyond ~60–80 hours of shadowing, the incremental payoff is low unless you are substantially lacking in other clinical activities.
8.2 If You Are DO-Only or DO-Prioritized
A DO-optimized shadowing profile, based on matriculant data, would look like:
- 70–100 total shadowing hours, of which:
- 40–60 hours with DO physicians (ideally in primary care or outpatient settings, but not exclusively)
- 20–40 hours with MD or mixed physicians in other specialties to demonstrate breadth
Alongside:
- 500–800+ hours of clinical employment/volunteering, comparable to MD applicants.
The data show that DO shadowing is not optional. For most DO schools, <20 DO hours falls below their typical matriculant range and carries significant risk.
8.3 If You Are MD+DO Mixed
Here the data push toward a hybrid target:
- 60–90 total shadowing hours, with:
- 30–45 hours with MD physicians
- 30–45 hours with DO physicians
This range situates you:
- Above the MD median for total shadowing, satisfying nearly all MD expectations;
- At or near the median DO hours (especially DO‑specific), giving you realistic access to DO acceptances.
Viewed as a portfolio allocation problem, you are balancing:
- Sufficient volume for MD
- Adequate osteopathic signaling for DO
- Time preserved for MCAT, GPA protection, research, and leadership
Key Takeaways
- Over the last 5 years, DO matriculants consistently report 30–50% more total shadowing hours than MD matriculants, with a stable median of ~40–60 hours specifically with DO physicians.
- MD admissions behavior treats shadowing as a threshold variable (often satisfied around 40–50 hours), while DO admissions use DO‑specific shadowing as a strong signal of genuine osteopathic interest.
- For mixed MD+DO applicants, the data support a deliberate strategy: approximately 60–90 total shadowing hours, split roughly evenly between MD and DO physicians, optimizes flexibility without overinvesting in low‑yield additional shadowing.





















