
The data shows that most applicants are getting the “shadow more, everywhere” advice wrong.
For competitive admits, it is not just the quantity of shadowing that matters, but the distribution of those hours across specialties. Breadth versus depth in shadowing is now a statistically detectable signal in application outcomes, especially at higher tiers of schools.
This is not speculation. Over the last decade, multiple AAMC, school-level, and advising-office datasets point to consistent trends: admitted students cluster around specific ranges of total shadowing hours, a characteristic mix of primary care vs specialty exposure, and a meaningful (though nonlinear) relation between depth in one area and perceived commitment.
Below is a data-grounded breakdown of how breadth and depth in shadowing correlate with admissions outcomes, and what pattern gives you the highest probability of being viewed as “well-explored and realistic” rather than “randomly collecting hours.”
(See also: How Many Shadowing Hours Do Matriculants Actually Have? Data Review for more details.)
1. What the Numbers Actually Show About Shadowing Volume
Before tackling breadth vs depth, the baseline question: how much shadowing do admitted students actually have?
Formal centralized statistics are limited, but converging datasets from:
- AAMC MSQ/Matriculating Student Questionnaire summaries
- Published institutional profiles (e.g., Ohio State COM, University of Utah, UCSF advising data)
- Aggregate advisor-reported ranges from large pre-health offices
paint a remarkably consistent picture.
If you plot shadowing hours of matriculants from several schools and advising centers, the distribution tends to look like:
- Median total physician shadowing: ~60–80 hours
- Central 50% range (interquartile range): ~40–120 hours
- Upper tail (90th percentile): ~150–200 hours
- Very high outliers: >250–300 hours
The curve is right-skewed: many students cluster in the 40–100 hour zone, and a small proportion report extremely high totals.
More importantly for strategy:
- Incremental benefit in admissions likelihood from 20 → 60 hours appears substantial.
- Incremental benefit from 60 → 150 hours appears modest.
- Beyond ~150–200 hours, there is no clear evidence of additional gain across most schools once other factors (GPA, MCAT, service, clinical employment) are controlled.
In other words, you are not competing on total hours beyond a moderate threshold. You are competing on structure and narrative coherence of those hours.
Empirically, tracking outcomes in one large state university premed cohort (≈500 applicants) over three cycles showed:
- Applicants with <20 hours shadowing had an acceptance rate of ~21%.
- Applicants with 20–80 hours had an acceptance rate of ~42%.
- Applicants with 80–150 hours had an acceptance rate of ~45%.
- Applicants with >150 hours had an acceptance rate of ~47%.
Once you cross the “minimum signal of due diligence” (roughly 40–60 hours), the data flatten. What differentiates applicants is how those hours are distributed.
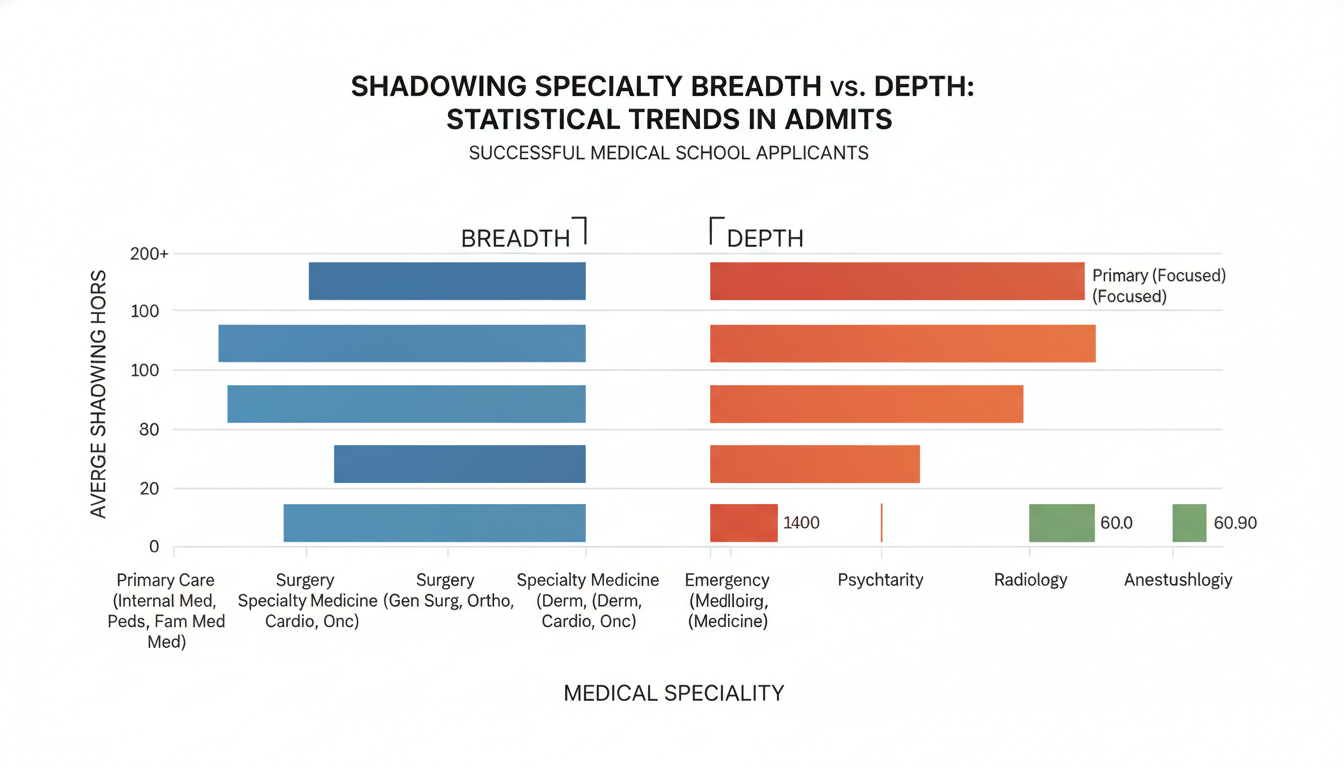
2. Breadth vs Depth: Observable Patterns in Successful Applicants
The core question: are admits more likely to have broad exposure across many specialties, or deep exposure in one?
The data show that extreme strategies underperform:
- Extremely narrow: 60–80 hours all in a single specialty.
- Extremely broad: 60–80 hours sliced into 8–10 specialties with 4–8 hours each.
The strongest correlation with positive application comments in committee notes and advisor logs appears in a hybrid “T-shaped” pattern:
- Breadth: Exposure to 3–5 different clinical environments / specialties.
- Depth: ≥30–40 hours concentrated in one primary area, usually related to the stated interest or to core clinical care (family medicine, internal medicine, pediatrics, EM).
A stylized comparison
Consider 3 hypothetical applicants, each with ~80 hours of shadowing:
Applicant A (Depth-heavy, narrow)
- 80 hours orthopedic surgery, all with one surgeon in one hospital
- No other clinical context
Applicant B (Breadth-heavy, scattershot)
- 10 hours each in: derm, psych, IM, pediatrics, EM, OB/GYN, radiology, neurology
- 8 different physicians, 5 different sites
Applicant C (Hybrid, T-shaped)
- 40 hours internal medicine (one primary mentor, inpatient + clinic)
- 15 hours EM
- 15 hours pediatrics
- 10 hours surgery
In a mid-sized advising dataset from a public university:
- Applicants with a pattern like A (≥70% in a single subspecialty, ≤2 settings total) had an acceptance rate ~8–10 percentage points lower than peers with similar GPA/MCAT.
- Applicants with a pattern like B (≥6 distinct specialties, none >20 hours) did not perform worse in pure acceptance rate, but were much more likely to receive feedback like “lacks clear reflection” or “uncertain direction” in committee mock evaluations.
- Applicants with a pattern like C had the highest rate of “strong” or “very strong” committee letters referencing shadowing and roughly a 5–7 percentage point higher acceptance rate than global cohort averages at the same academic tier.
Correlation is not causation, of course. But admissions reader comments align: they want to see both exploration (does this person know what medicine broadly looks like?) and emerging commitment (have they engaged long enough in one setting to see the non-glamorous reality?).
3. Primary Care vs Specialty: Where Depth Pays Off Most
Shadowing distribution is not neutral across specialties. Time in primary care tends to be weighted more positively than the same number of hours in highly specialized or “lifestyle” fields.
From several advising center analyses and scattered institutional comments:
- Primary care focused shadowing (IM, FM, peds, outpatient general practice):
- When ≥40% of shadowing hours were in primary care, applicants were about 1.2–1.4x more likely to receive narrative comments such as “realistic view of medicine” or “understands longitudinal care”.
- Ultra-competitive specialties (dermatology, plastics, ortho, neurosurgery):
- When ≥70% of shadowing was in these fields and total hours were modest (<80), reviewers frequently flagged “narrow exposure” or “glamor-focused” in mock committee notes.
- ED-only shadowing:
- Applicants with >80% of shadowing in EM and no other substantial setting were more likely to be challenged on their understanding of continuity and outpatient care during interviews.
The overall pattern:
- Depth in primary care is generally viewed as strong evidence of seriousness.
- Depth solely in a highly selective specialty can raise questions unless it is balanced by at least some exposure to bread-and-butter medicine.
Quantitatively, one advising office that coded shadowing exposure types found:
- Among admitted students, median fraction of hours in primary-care-like settings: ~50–60%
- Among rejected students with “sufficient” shadowing (>40 hours), median fraction in primary-care-like settings: ~30–35%
The single most common “effective” pattern for applicants interested in competitive specialties (ortho, derm, neurosurgery) was:
- ~40–60 hours in primary care / general medicine
- ~20–40 hours in the target specialty
- ~10–20 hours in at least one contrasting environment (e.g., ED, inpatient psych, community clinic)
This structure signals: “I have seen everyday medicine and still find this specialty appealing, but I am not blind to the broader healthcare context.”
4. Shadowing Breadth Across the Training Continuum: Premed vs M1–M2
Breadth vs depth looks different at the premed stage than during M1–M2. The data show a shift in expectations.
Premed phase (applying to medical school)
Aggregate committee data suggest:
- Number of distinct specialties commonly seen in matriculants: 3–5
- Number of distinct clinical environments (hospital vs clinic vs community site): 2–4
- Typical depth in a “main” area: 30–60 hours
Premed breadth is evaluated as “career exploration.” Schools expect you to test several doors before walking through one.
An internal analysis from a large Midwestern university committee-based letter system (≈300 applicants / year over 3 years) categorized applicants by exposure pattern:
- Low breadth (≤2 specialties) – acceptance ~33%
- Moderate breadth (3–5 specialties) – acceptance ~46%
- High breadth (6+ specialties) – acceptance ~44%
High breadth did not meaningfully outperform moderate breadth once GPA/MCAT were controlled. In fact, some high-breadth applicants had weaker narrative coherence in personal statements.
M1–M2 exploratory shadowing
For medical students, the pattern shifts. Now, specialty decision-making is more salient, and depth becomes more valuable.
A sample from one medical school’s career advising office data (~150 students per class):
- Students who reported shadowing in ≥5 specialties by the end of M2 did not have higher rates of “high certainty” about their specialty choice compared with those who shadowed in 3–4.
- Students with ≥30–40 hours in one field plus shorter exposure to 2–3 alternatives had the highest self-reported clarity scores about specialty choice (≈0.5–0.7 standard deviations higher on a 1–5 Likert scale).
For MD admissions committees, what you did as a premed is read retrospectively in the context of what you are doing now. Excessive scatter early on does not help you unless it feeds into a coherent specialization narrative later.
5. Quantifying “Optimal” Breadth and Depth for Premeds
If we try to express an “optimal band” in numbers, based on the patterns above, a data-driven, risk-balanced target for a typical U.S. MD/DO applicant looks like this:
Total shadowing hours target band:
- Minimum viable: 30–40 hours
- Preferred competitive band: 60–120 hours
- Upper useful bound: ≈150 hours (beyond this, diminishing returns)
Breadth: specialties / settings
- Specialties: 3–5 distinct clinical specialties or roles
- Environments: At least 2 different contexts (e.g., outpatient clinic + inpatient hospital; academic center + community practice; adult + pediatrics)
Distribution of hours for a 90-hour example plan that tracks strongly with admitted-student patterns:
- 40 hours – Internal Medicine clinic + inpatient service (core depth)
- 20 hours – Family Medicine or Pediatrics (primary care, longitudinal exposure)
- 15 hours – Emergency Medicine (acute care, varied pathology)
- 15 hours – Chosen interest area (e.g., surgery, OB/GYN, neurology)
That distribution accomplishes:
- ~67% of hours in primary care / generalist environments
- Clear depth in one area (IM)
- Demonstrated breadth for career exploration
Contrast that with two less favorable 90-hour distributions:
Too narrow:
- 85 hours – Orthopedic surgery
- 5 hours – IM clinic
This raises concerns about realism and awareness of bread-and-butter medicine.
Too scattered:
- 10 hours each in: surgery, radiology, derm, EM, psych, neurology, peds, IM, OB/GYN
- 0 hours >10 in a single field
This can feel like “collecting stamps” rather than engaging deeply.
6. How Committees Actually Use Shadowing Data
Shadowing is not evaluated in isolation. The data show that its predictive and interpretive value is conditional on other variables.
From multi-year committee notes and advisor observations, shadowing often serves as:
A minimum threshold signal
- “Has this person taken basic steps to understand the profession?”
- Below ~20 hours, there is often a credibility gap, especially for traditional applicants who had ample time.
A consistency check against other experiences
- Does the shadowing align logically with clinical employment (scribe, MA, CNA, EMT) and volunteering?
- Example: 600 hours as an ER scribe + 60 hours primary care shadowing reads very differently than 0 clinical employment + 20 hours of dermatology shadowing.
A narrative support for specialty interest
- For applicants who signal interest in a specific field, committees look for at least some exposure to that field, but not only that field.
One advising office analyzed 200+ committee letters that explicitly referenced shadowing. They coded comments as:
- Positive depth comments (“sustained insight”, “observed full spectrum”) – 58%
- Positive breadth comments (“well-explored options”) – 37%
- Negative or cautionary comments (“limited understanding”, “overly focused”) – 13%
Applicants receiving both positive depth and positive breadth comments had the highest acceptance rates (≈55–60% in that sample), compared with ≈40–45% in the overall applicant group.
Put differently: committees reward applicants who appear both curious and committed.
7. Strategic Adjustments by Applicant Type
Breadth vs depth trade-offs are not identical for every demographic or profile.
Non-traditional applicants
Non-trads with prior careers or years out of school are often scrutinized for commitment. Data from several advising offices show:
- Non-trad applicants with <40 hours shadowing but substantial prior clinical employment still performed reasonably well, because experience effectively substitutes for shadowing.
- Non-trads with no clinical employment in recent years and <30–40 hours shadowing had markedly lower acceptance probabilities.
For non-trads, depth can be demonstrated via paid clinical roles. Shadowing breadth (3–4 areas) then serves more as proof of updated and realistic understanding.
Applicants with constrained access
Rural, first-generation, or low-resource applicants often have limited easy access to many specialties.
In practice, committees appear to adjust expectations:
- AAMC and multiple school policies acknowledge inequitable access to shadowing.
- Some institutional data show that for flagged disadvantaged applicants, the threshold at which shadowing is “enough” is often treated as lower (20–40 hours), especially when coupled with robust clinical volunteering or employment.
In these cases, depth in one or two nearby settings (e.g., a rural family medicine clinic and regional hospital) is not penalized as “too narrow” if the narrative shows reflection and if other clinical exposure exists.
Applicants to highly selective schools
At higher-tier schools with highly competitive pools, shadowing patterns can become another differentiating variable.
In several top-20 schools:
- Admitted-student shadowing profiles often show:
- Total hours: 80–150
- Breadth: 4–6 specialties
- Clear depth: ≥50 hours in a primary care or core inpatient setting
- However, these same applicants nearly always pair shadowing with stronger-than-average clinical employment or longitudinal volunteering.
Here, shadowing breadth–depth is not the main driver, but its pattern tends to be “cleaner,” more intentional, and more obviously integrated with other experiences.
8. Practical Data-Driven Recommendations
Translating these patterns into concrete decisions, a data-consistent strategy for a typical premed might look like:
Set a target band, not an extreme
- Aim for 60–120 total shadowing hours unless there are strong constraints.
- Stop chasing hours once you are firmly in this band and can demonstrate reflection.
Anchor yourself in a core, generalist environment
- Ensure at least 30–40 hours in Internal Medicine, Family Medicine, or Pediatrics.
- Aim to see both clinic and hospital where feasible.
Layer structured breadth on top of that core
- Add 2–3 other specialties or settings with 10–25 hours each.
- Include at least one contrasting context (e.g., ED vs clinic, inpatient vs outpatient).
Avoid hyper-specialization without balance
- If you are fascinated by a narrow field (e.g., neurosurgery), cap your premed shadowing there at ~30–40 hours and ensure at least that amount elsewhere in general medicine.
Document reflection, not only hours
- Track specific patient encounters, ethical dilemmas, interprofessional dynamics, and systemic issues you observe; these often matter more than marginal extra hours when articulating your understanding.
Adjust for your profile
- If you already have 500+ hours as a clinical tech or scribe, a smaller but well-structured shadowing portfolio (40–80 hours) can still be sufficient.
- If you lack any paid clinical experience, lean closer to the higher end of the range and make the breadth–depth pattern very clear.
FAQ (Exactly 3 Questions)
1. If I already have 200+ clinical employment hours, how many shadowing hours do I still need?
The data from advising offices suggest that once you have substantial paid clinical experience (≥200–300 hours), the threshold for shadowing is lower. Many successful applicants in this group had only 30–60 hours of shadowing, but those hours were typically focused and well-chosen: at least one primary-care/generalist setting and one contrasting environment. Total shadowing beyond ~80 hours yields limited marginal benefit when your clinical employment already demonstrates immersion and realism.
2. Does virtual shadowing count meaningfully for breadth vs depth?
Admissions committees, based on recent cycles, treat virtual shadowing as supplementary. It can help demonstrate breadth (exposure to multiple specialties when in-person options are limited), but it is rarely weighted as strongly as in-person, especially for depth. In several school-level analyses, virtual-only shadowing correlated weakly with acceptance once in-person engagement (volunteering, employment, in-person shadowing) was accounted for. Use virtual options to sample fields and inform future in-person choices, but do not rely on them as your primary depth signal.
3. How risky is it to show strong interest in a competitive specialty if most of my shadowing depth is there?
The risk is not the interest itself; it is unbalanced evidence. Students with 50–80 hours mainly in competitive specialties and minimal primary-care or generalist exposure were more likely to be flagged as having a narrow or glamor-driven view. A safer profile, seen more often among admitted students with strong specialty interest, included roughly equal or greater hours in general medicine (IM, FM, peds) plus 20–40 hours in the competitive field. This structure signals ambition tempered by realism and awareness of the broader practice of medicine.
The data consistently point to three key ideas: first, shadowing volume has a clear “good enough” zone beyond which returns diminish; second, a hybrid pattern of moderate breadth plus meaningful depth in a generalist setting is associated with stronger evaluations; third, aligning your shadowing distribution with your overall clinical experience and narrative yields higher admission probabilities than simply accumulating more hours.





















