
The boring shadowing day is not the physician’s fault. It is a systems problem—and you can fix it with structure.
Most premeds treat office shadowing like watching Netflix with a white coat. They sit, observe quietly, go home, and then wonder why the day felt useless and why they struggle to write meaningful application essays about “clinical experience.”
That approach wastes your time, the physician’s time, and a real opportunity for clinical growth.
You can turn a slow, awkward office shadowing day into focused, high-yield clinical learning—without breaking etiquette, annoying staff, or violating patient comfort. You just need a clear framework, the right tools, and some specific scripts.
This is that framework.
Step 1: Redefine What “Counts” as Learning
Office shadowing feels boring when you expect drama: codes, resuscitations, rare diseases. You will not get that in a typical clinic.
In outpatient medicine, the learning is subtle:
- How the physician moves from door to door without burning out
- How they build trust in the first 60 seconds
- How they translate complex pathophysiology into 7th-grade language
- How they manage patients who disagree, resist, or demand unnecessary tests
- How they make small decisions that prevent hospitalizations six months later
If you walk in expecting “cool cases,” you will miss 90% of the real education.
Reframe your learning goals
Before your next shadowing day, define three categories of learning:
-
- How does the physician introduce themselves?
- How do they ask sensitive questions (sexual history, finances, mental health)?
- How do they end a visit when the patient keeps talking?
Clinical reasoning
- How does the chief complaint turn into a working diagnosis?
- What questions narrow the differential?
- What labs or imaging are ordered—and more importantly, what is not ordered?
-
- How does the team coordinate (MA, front desk, nurse, physician)?
- What slows the day down?
- Where do errors almost happen and then get caught?
You are not just watching “what happens.” You are dissecting how and why it happens.
Write one specific, observable goal in each category:
- Communication: “Observe exactly how Dr. Kim responds to a patient who disagrees with the plan.”
- Clinical reasoning: “Track how the first three questions in each visit differ based on presenting complaint.”
- Systems: “Map the steps from patient check-in to check-out for one visit.”
Now you have a lens. Boredom drops dramatically when your brain is hunting for specific patterns.
Step 2: Build a Simple Shadowing Toolkit
If you walk in with nothing but your student ID and a water bottle, you are unprepared. A shadowing day is a professional learning event—treat it like one.
Bring a minimal but intentional toolkit:
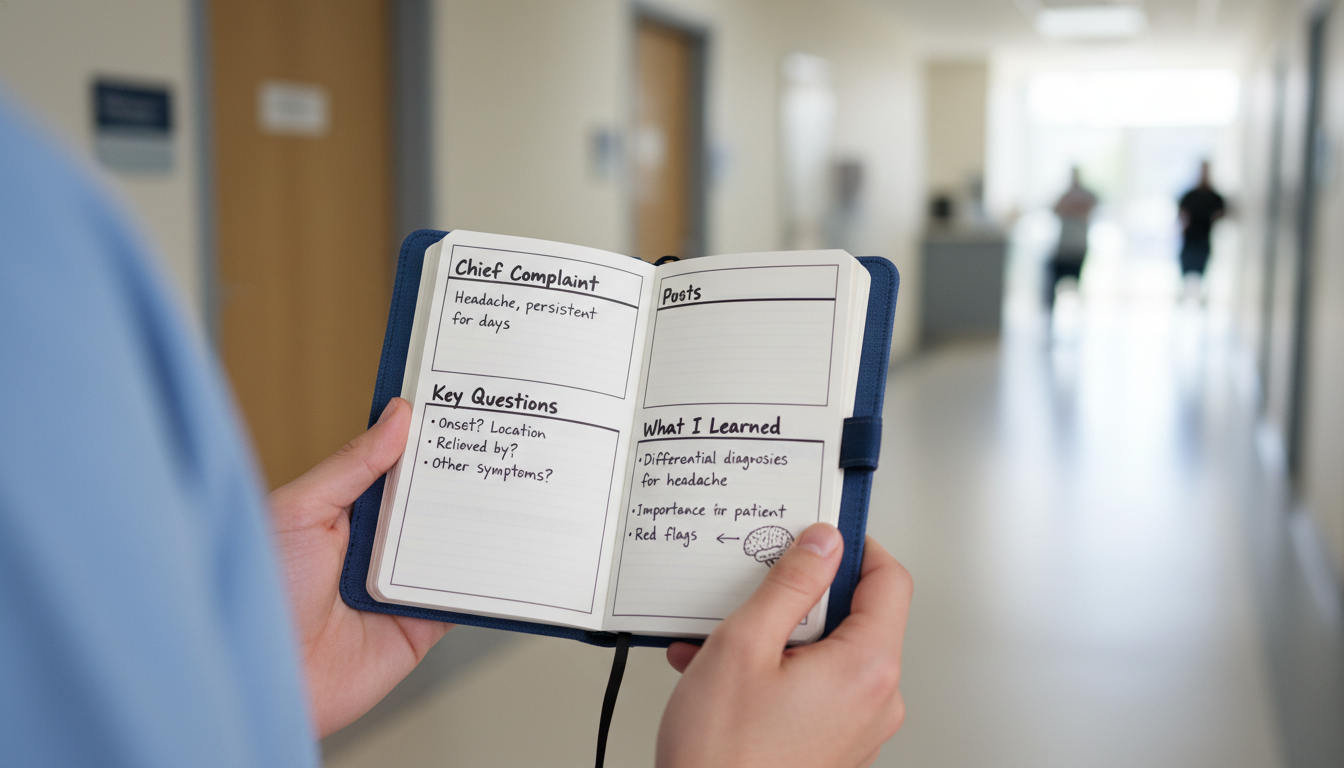
Pocket notebook (or small flip notebook)
- One page per patient (no identifiers—more on that below)
- Sections for: Chief complaint, 2–3 key questions asked, 1 thing you learned
Two pens
- One fine-tipped for discreet writing in hallways
- One backup (pens mysteriously vanish in clinics)
Pre-written question list
- 10–15 questions sorted by category (communication, clinical reasoning, career)
- You will never ask them all. The point is to avoid “blank mind” syndrome when the physician says, “Any questions?”
Time-blocked personal plan
- Break your day into 90-minute learning blocks
- Assign each block a primary focus:
- Block 1: “How Dr. Lopez builds rapport in minute 1”
- Block 2: “How diabetes follow-ups differ from new patient visits”
- Block 3: “How the MA and physician share information”
This structure keeps you engaged even when the cases are repetitive.
Step 3: Set the Day Up Correctly in the First 5 Minutes
Most boredom is locked in before the first patient is seen.
If the physician thinks you are “just here to observe,” they will default to silence. If they understand you are serious about learning within appropriate boundaries, many will engage more intentionally.
Use a clear, respectful opening script
As soon as you meet the physician, say something like:
“Thank you for letting me shadow today. To make sure I am not in the way and that I actually learn something useful, I planned a few focused goals.
During patient visits I will stay quiet unless you invite me to speak, and I will respect any visit you would prefer me to skip.
Between patients, would it be alright if I ask brief questions about your reasoning or communication, as long as I keep it to 2–3 minutes?”
This does several things:
- Signals professionalism and planning
- Respects time and patient boundaries
- Makes it easier for them to think of you as a learner, not a shadow
You can also hand them a one-page “learning goals” sheet you prepared:
- 3 bullet points: what you are hoping to learn
- 2–3 lines: relevant background (year in school, courses taken)
- 1 line: any particular interests (primary care, neurology, surgery, etc.)
It may feel over-prepared. Clinics run on structure—this aligns you with that.
Step 4: Use a Visit-by-Visit Observation Framework
If you just “watch the visit,” your brain will wander. Use a consistent observation framework for each encounter.
For every patient you see, mentally run through this 5-part checklist:
Doorway Moment (10–20 seconds)
- What does the physician do before entering? (Review chart? Deep breath? Knock?)
- How do they greet the patient? (Handshake? Use the patient’s name? Sit or stand?)
- What is the first question?
Information Gathering
- What type of questions are used:
- Open-ended: “Tell me what brings you in.”
- Focused: “When did the pain start?”
- Clarifying: “When you say dizzy, do you mean lightheaded or spinning?”
- What is not asked? Why might that be?
- What type of questions are used:
Transition to Assessment/Plan
- Exact phrases used when shifting from listening to explaining:
- “Let me summarize what I’m hearing…”
- “Based on your symptoms, here is what I am thinking…”
- How the doctor frames uncertainty:
- “I am not certain yet, so I want to rule out…”
- Exact phrases used when shifting from listening to explaining:
Patient Education and Shared Decision-Making
- What analogies or visuals are used?
- How does the physician check for understanding?
- How do they respond to disagreement? (“I do not want that medication,” “I read online that…”)
Closure
- How does the visit end?
- Does the physician:
- Ask: “Any other questions today?”
- Review next steps clearly?
- Use teach-back (“Can you repeat how you will take this medication?”)
Write down only patterns and phrases, no patient identifiers:
- Example entry in notebook:
- CC: “back pain 3 weeks”
- Key Qs: “What makes it better/worse?”, “Red flags?” (weakness, incontinence)
- Phrase: “I cannot fix all pain today, but we can improve your function.”
This structure lets you extract value from even the fifth “back pain” visit of the day.
Step 5: Turn Slow Times into Micro-Learning Sessions
There will be downtime:
- Late patients
- No-show appointments
- Charting backlogs
- Insurance calls
The default is scrolling your phone or staring at the wall. Replace that with pre-planned micro-learning.
Have a “downtime menu”
Prepare a short list of things you can do in 5–15 minutes:
Ask targeted questions
- “Could you walk me through your thought process on that chest pain patient, from when you saw the chief complaint in the chart to your final plan?”
- “What is one common misunderstanding premeds have about primary care?”
- “You mentioned avoiding unnecessary imaging. How do you decide when to say no to a patient’s request?”
Deconstruct a specific skill
- “I noticed you calmed down a very anxious patient quickly. What were you paying attention to, and what phrases do you rely on?”
- “How did you learn to give bad news without overwhelming patients?”
Shadow another part of the system (only with permission)
- Ask: “If there is a brief period where you are charting, would it be appropriate for me to observe how the MA or nurse works, as long as they are comfortable and I stay out of the way?”
- You may see:
- Blood draw workflow
- Vaccine administration
- Prior authorization phone calls
- Scheduling challenges
Structure your notes
- Turn messy notes into brief “learning summaries”
- Example template:
- “Today I learned three ways physicians handle unrealistic requests:
- Validate concern
- Explain risk vs benefit in concrete numbers
- Offer a safe alternative plan.”
- “Today I learned three ways physicians handle unrealistic requests:
Use small windows of time intentionally; they often hold the richest teaching moments.

Step 6: Stay Within Ethical and Professional Boundaries
High-yield learning never justifies boundary problems. You must protect patient privacy, autonomy, and clinic flow.
Patient consent and comfort
Always:
- Allow the physician to introduce you:
- “This is [Your Name], a pre-medical student observing today. Is it alright if they stay in the room during the visit?”
- If the patient hesitates, step out immediately and without visible frustration.
- Use a neutral phrase: “Of course, thank you,” and leave.
Do not:
- Introduce yourself as “doctor,” “student doctor,” or “medical student” if you are not
- Touch patients or perform any exam maneuvers unless explicitly invited by the physician and consented by the patient (and the institution allows it)
Note-taking and HIPAA
Your notebook:
- Must never include:
- Names
- Dates of birth
- MRNs
- Unique identifying details (rare disease + specific town + age, etc.)
- Should use generic labels:
- “Middle-aged man, uncontrolled diabetes”
- “Young adult with new depression symptoms”
If you ever think, “Could someone identify this patient from this note?” then change or delete it.
Step 7: End the Day with a 10-Minute Debrief
Many students just say “Thank you” and leave. You are leaving learning (and letters of recommendation) on the table.
Ask for a quick exit debrief
Near the end of the day, say:
“Would you have 5–10 minutes before I leave for any feedback or final thoughts? I would appreciate any advice on how I can learn more effectively from shadowing or prepare for medical training.”
Use those minutes to:
Summarize your learning
- “Three things I learned today were:
- How you set expectations early when there are multiple issues to cover
- How you balance reassurance with not missing serious disease
- How much time you spend documenting and coordinating care outside the room”
- “Three things I learned today were:
Ask one reflective question
- “What do you know now about outpatient medicine that you wish you had known before medical school?”
- “What kind of student stands out to you as particularly ready for clinical training?”
Clarify future opportunities
- “Would it be alright if I email you in a few months with any follow-up questions or updates on my path?”
- “If your schedule permits, I would be very grateful to shadow again in the future, especially during [type of clinic].”
This short debrief:
- Reinforces that you took the day seriously
- Gives you better insight than 8 hours of silent observation
- Lays the groundwork for a stronger relationship
Step 8: Convert the Day into Application-Ready Material
A shadowing day is not just about that day. It should feed:
- Your personal statement
- Your activity descriptions
- Your future interview answers
- Your internal clarity about medicine
That night: 20-minute consolidation protocol
Within 24 hours, do this:
Write a one-page “Clinical Learning Summary”
- Headings:
- “Most meaningful patient interaction”
- “Most important communication skill I observed”
- “One misconception about outpatient medicine that changed today”
- “How this reinforced or challenged my interest in medicine”
- Headings:
Extract 2–3 specific anecdotes
- Example:
- “I watched Dr. S. gently redirect a patient who wanted unnecessary antibiotics. She…”
- Remove all identifiers
- Focus on:
- The tension or challenge
- What the physician did
- What you learned
- Example:
Translate learning into future behavior
- “Because I saw [X], I now plan to [Y] in my own development.”
- Example:
- “After seeing how much time chronic disease requires, I plan to seek long-term volunteer work with diabetic patients rather than only doing short health fairs.”
These reflections turn “I shadowed 40 hours” into “I can articulate how physicians think, communicate, and manage real-world constraints.”
Step 9: Troubleshooting Common Shadowing Problems
You can do everything right and still run into obstacles. Here is how to handle the most common ones.
Problem 1: The physician barely talks to you
Do this:
- Accept that some attendings are exhausted, behind on notes, or just not inclined to teach
- Use structured self-observation more heavily (your 5-part visit checklist)
- Ask micro-questions that can be answered while walking:
- “What were you mainly trying to rule out with those first few questions?”
- “What made you choose that medication instead of [alternative]?”
At lunch or at the end of the day, ask:
“I know clinic is extremely busy. Are there particular aspects of visits you think I should focus my observations on today to learn the most?”
This respects their time while showing initiative.
Problem 2: The clinic is mostly routine refills and follow-ups
Perfect. That is real medicine.
Adjust your lens:
- Focus on:
- Preventive care
- Longitudinal relationships
- Behavior change conversations
- Track:
- How adherence is discussed
- How small wins are celebrated
- What systems are used to track chronic disease metrics (A1C, BP, etc.)
Challenge yourself:
- “How would I briefly explain to a family member why this 10-minute blood pressure visit matters long term?”
Problem 3: You feel like you are in the way
Mitigate by:
- Asking the MA or nurse quietly: “Where is the best place for me to stand or sit so that I am not in anyone’s way?”
- Positioning yourself:
- Near a wall, not blocking drawers
- Behind and slightly to the side of the physician, not directly facing the patient initially
- During room turnovers:
- Offer to step into the hallway quickly
- Never touch supplies or equipment unless instructed
Reassure yourself: your presence is a normal part of academic and community medicine. You are not a burden if you are respectful and low-friction.
Step 10: A Simple Template for Your Next Shadowing Day
Here is a concise protocol you can literally copy for your next office day.
The Night Before
- Set 3 learning goals (communication, reasoning, systems)
- Prepare:
- Pocket notebook labeled with date and clinic
- 10–15 questions list
- Print or write a one-page learner introduction (goals + background)
Morning: First 10 Minutes
- Introduce yourself and your goals to the physician
- Clarify boundaries:
- When and how you may ask questions
- Any parts of clinic you should avoid (procedures, counseling, etc.)
During Each Visit
- Run the 5-part observation checklist
- Record:
- Chief complaint (generic)
- One key question
- One phrase or behavior that stood out
During Downtime
- Choose from your “downtime menu”:
- One targeted question
- Observation of another team member (if allowed)
- Note consolidation
End of Day
- Ask for a 5–10 minute debrief
- Express gratitude with specific learning points
That Evening (20 minutes)
- Write a one-page Clinical Learning Summary
- Pull out 2–3 de-identified anecdotes
- Reflect: “What did today show me about the reality of being a physician?”
Do this consistently, and even the quietest clinic becomes a powerful classroom.
FAQ
1. How many hours of office shadowing are actually useful before it becomes repetitive?
For most premeds, 20–40 hours of high-quality, structured shadowing in a single setting is enough to deeply understand that environment. Beyond that, diversify: urgent care, inpatient, different specialties, community vs academic clinics. The goal is breadth of systems and depth of reflection, not just packing hours.
2. Should I ever ask the physician if I can speak during the patient visit?
Yes, but only if the relationship is established and the physician invites it. For example, after a few hours, you might ask privately: “If there are appropriate moments where I could ask the patient one or two simple questions, would that be acceptable, or would you prefer I remain completely silent?” Many physicians will either give you specific guardrails or say they prefer silence. Respect their choice fully.
3. Is it worth shadowing in a specialty I do not think I am interested in?
Yes. Early on, your goal is to understand what any outpatient clinical day looks like: pace, documentation load, patient emotional tone, team interactions. Even if you never go into dermatology or endocrinology, understanding how chronic disease is managed in the outpatient world will inform your future specialty decisions and help you speak intelligently in interviews.
4. How can I follow up after shadowing without being annoying?
Within 24–48 hours, send a concise thank-you email:
- 3–4 sentences max
- Mention 1–2 specific things you learned
- Express interest in staying in touch Later, you can send occasional brief updates (every few months) about major milestones: MCAT taken, acceptance to medical school, etc. Keep messages short, specific, and respectful of their time.
Open your calendar right now and block out 30 minutes to build your next shadowing toolkit: write your 3 learning goals, draft your physician introduction script, and set up your pocket notebook template. That simple preparation is the difference between another boring day and real clinical learning.





















