
You are here
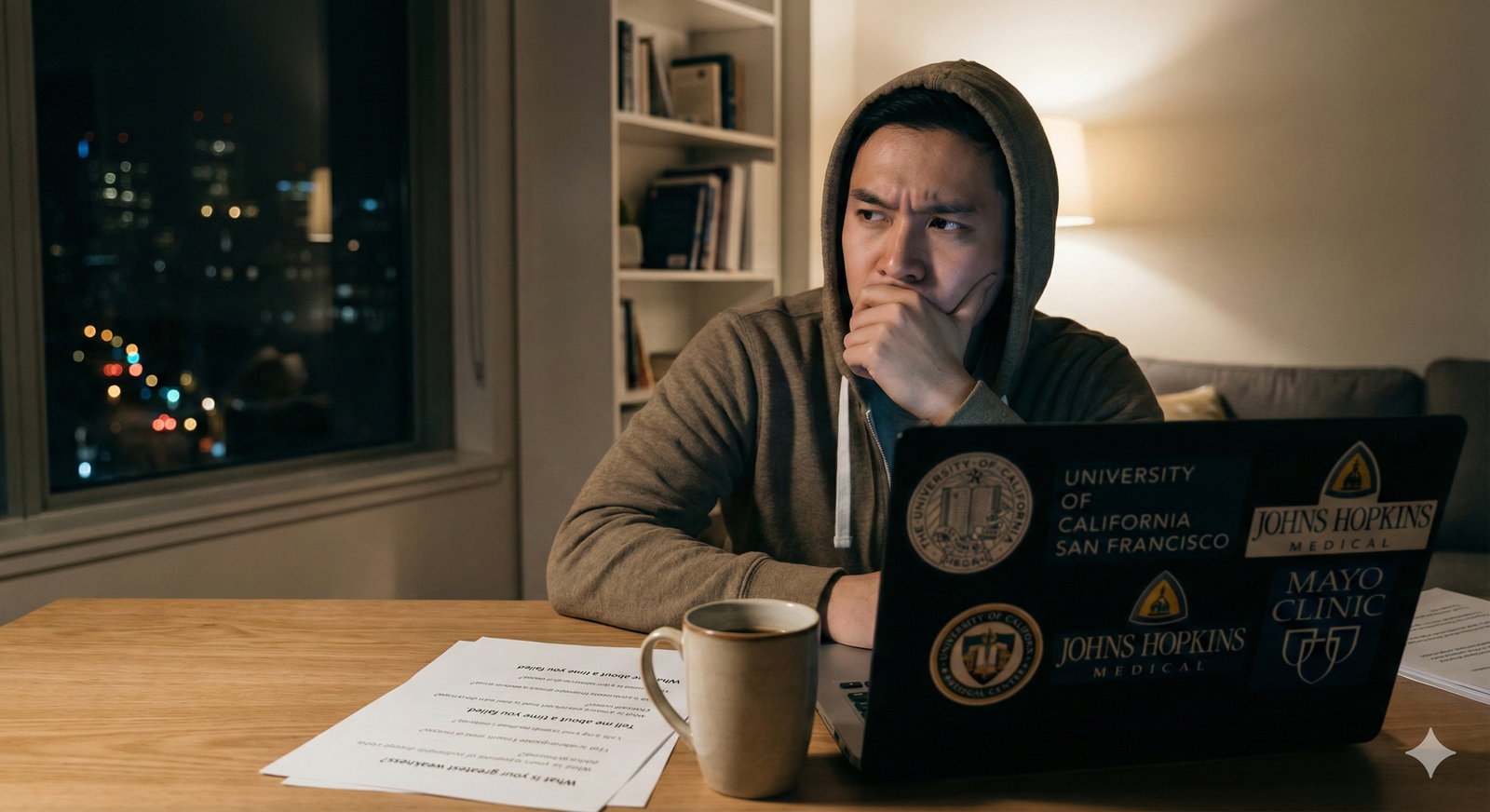
It is 9:00 p.m. on a Tuesday. Your first residency interview is in 48 hours.
You have:
- A mostly updated ERAS application
- A vague memory of “STAR format” from some workshop a year ago
- A calendar full of interviews you somehow booked
- And no real, structured prep for behavioral questions
This is the cram plan. You have 48 hours. I am going to walk you through what to do hour by hour, not vague “practice some answers” nonsense.
You will not become a perfect, polished TED Talk speaker in two days. You can, however, become:
- Organized in your stories
- Clear in your structure
- Ready for 90% of the behavioral questions you will actually be asked
Let’s break the 48 hours.

| Period | Event |
|---|---|
| Day 1 - Hour 0-2 | Inventory experiences |
| Day 1 - Hour 2-4 | Build core stories STAR |
| Day 1 - Hour 4-6 | Map stories to questions |
| Day 1 - Hour 6-10 | First practice round + refine |
| Day 2 - Hour 24-28 | Targeted practice by theme |
| Day 2 - Hour 28-32 | Mock interview + feedback |
| Day 2 - Hour 32-40 | Polishing + red-flag review |
| Day 2 - Hour 40-46 | Light run-through, logistics |
| Day 2 - Hour 46-48 | Rest, mental reset |
Hour 0–2: Build your raw material bank
At this point you should stop googling “top 50 residency behavioral questions” and actually gather your own content. Interviewers do not care if you read a list. They care if you have real stories.
Step 1 (0:00–0:30) – Pull your documents and data
You need everything in one place:
- Your ERAS application (PDF)
- Your CV
- Personal statement
- Rotation evaluations (at least the narrative parts)
- Any awards, leadership roles, significant projects
Print them or keep them open on your laptop in separate tabs. You will mine these for stories.
Step 2 (0:30–1:30) – Rapid experience inventory
You are building your “story bank.” Goal: 15–20 specific situations.
Create a simple 3-column table for yourself (paper or Word):
| Category | Experience Title | Quick Notes |
|---|---|---|
| Leadership | Led new sign-out process | IM Sub-I |
| Conflict | Disagreement with senior | Surgery rotation |
| Failure | Missed lab follow-up | M3 Inpatient |
| Teamwork | Covered understaffed floor | Night float |
| Stress/Overload | 28-hour call with crisis | ICU |
Now, speed write bullet entries under these categories. No polishing. Just get them down.
Hit at least:
- 3–4 leadership / initiative examples
- 3–4 conflict / difficult interaction examples (peers, nurses, attendings, patients)
- 3 failures or mistakes
- 3 teamwork / collaboration
- 2–3 stress / time management / resilience
- 2 patient communication / empathy / breaking bad news
If you are stuck, scan your rotation eval comments and your personal statement. Anywhere an attending wrote, “Handled X well” or “Showed growth in Y” is a story.
Step 3 (1:30–2:00) – Pick your core 8–10
You do not have time to polish 20 stories in 48 hours. Choose ~8–10 high-yield ones that are:
- Clear events with a beginning, middle, end
- Show different settings (inpatient, outpatient, overnight, ICU, pre-clinical project, etc.)
- Highlight different roles (leader, follower, communicator, learner, advocate)
These become your “core stories” that you will reuse and reshape.
Write a one-line label for each:
- “Difficult attending – mismatch expectations – improved with check-ins”
- “Code blue as M4 – low role but clear communication”
- “QI project on discharge summaries – resistance then adoption”
You are done with raw material. Now you shape it.
Hour 2–6: Turn experiences into STAR stories
At this point you should stop adding more stories. Depth beats quantity.
Use the STAR structure:
- Situation – brief context
- Task – your role and goal
- Action – what you did, how you thought
- Result – outcome + reflection / learning
Step 4 (2:00–4:00) – Script rough STAR outlines
For each of your 8–10 core stories, build a skeleton, not a novel. Aim for 90–120 seconds per story when spoken.
Format per story:
- Situation (2–3 sentences)
- Task (1–2 sentences)
- 3–5 bullet points for Actions (what you actually did)
- Result / Reflection (2–3 sentences)
Example:
Story: Missed lab follow-up (failure / accountability)
- Situation: M3 on inpatient medicine, managing a panel with resident. Busy post-call morning with multiple discharges.
- Task: I was responsible for checking morning labs and alerting team to critical results.
- Actions:
- Prioritized discharge paperwork, falsely assumed normal labs.
- Realized in afternoon that a patient had a potassium of 6.1 that I had not flagged.
- Immediately notified resident and attending, apologized directly.
- Stayed late to follow the patient’s course, read about hyperkalemia management.
- Created a personal checklist system for lab review on subsequent days.
- Result: Patient was treated promptly once flagged and had no adverse outcome. Attending used it as a teaching point. I adopted that checklist system and used it consistently; evaluations later commented on my reliability with follow-up.
Do this for all core stories. Keep it tight. If you are writing paragraphs, you are overdoing it. You only need enough to trigger your memory and structure when speaking.
Step 5 (4:00–6:00) – Map stories to common question types
Now connect your stories to the questions that will actually be asked.
Create a quick mapping:
| Question Theme | Story # / Title |
|---|---|
| Conflict | #2 Difficult attending; #5 Nurse disagreement |
| Leadership | #1 New sign-out process; #4 Student-run clinic |
| Failure | #3 Missed lab follow-up |
| Stress/Burnout | #6 28-hour call ICU |
| Teamwork | #7 Understaffed floor coverage |
| Ethical Dilemma | #8 Patient refusing care |
You want:
- At least 2 stories that can serve as conflict
- 2 that show leadership / initiative
- 1–2 clear failure / mistake stories
- 1 that shows dealing with stress or overload
- 1 that shows handling a difficult patient / family
- 1 that shows ethical judgment / professionalism
This mapping lets you adapt quickly when the wording changes. “Tell me about a time you had a disagreement with a superior” and “Tell me about a difficult interaction with an attending” can both use the same story with minor framing.
Hour 6–10: First practice loop (out loud, not in your head)
By this point, you should stop writing and start talking. Silent prep creates fake confidence.
Step 6 (6:00–8:00) – Solo out-loud run-through
Use a timer and record yourself (phone voice memos is fine). For each story:
- Pick a common prompt (e.g., “Tell me about a time you failed.”)
- Answer with the story using STAR, aiming for 90–120 seconds
- Stop. Listen once. Identify:
- Rambling points
- Missing “Result / reflection”
- Overuse of jargon or acronyms
Mark in your notes:
- Cut phrases that add nothing (“it was just really crazy,” “I was like…”)
- Add one explicit learning sentence per story (“This changed how I…”)
You are not trying to memorize sentences. You are stabilizing structure.
Step 7 (8:00–10:00) – Introduce behavioral themes
Now practice answers to the actual common behavioral question classes using your mapped stories.
Core residency behavioral categories:
- Teamwork / collaboration
- Conflict (with peers, nurses, attendings, patients)
- Leadership / initiative
- Failure / mistake / weakness
- Stress / time management / workload
- Diversity / inclusion / working with different backgrounds
- Ethical / professionalism issues
- Handling feedback and growth
For each category, do:
- 2 different questions from an online list
- Answer using one of your mapped stories
- Keep answers to 1.5–2 minutes
You should feel patterns emerging. This is good. Behavioral interviews are pattern-based.
Day 2 – Hour 24–32: Targeted refinement and mock
Sleep. Then come back.
You now have about 24 hours until the interview. Day 2 is about refinement, realism, and preventing unforced errors.
Hour 24–28: Fix the weak categories
At this point you should know your thin spots. Most people are weak in one of these:
- A genuine failure story that does not sound fake or trivial
- A conflict story where they are not the hero and not the victim
- An ethical/professionalism situation with nuance
- A real, non-pageant answer to “What is your biggest weakness?”
Step 8 (24:00–26:00) – Deep work on 3 “must-not-screw-up” answers
Focus on:
Failure – Make sure:
- It is something that actually mattered (not “I studied too hard”).
- You own responsibility without throwing others under the bus.
- You have a clear behavior-level change that followed.
Conflict – Ensure:
- You show understanding of the other person’s perspective.
- You do not sound combative or passive-aggressive.
- You end with a concrete resolution and what you learned about communication.
Weakness – Criteria:
- Real, but not catastrophic (e.g., “struggle with delegating,” “tend to overprepare notes”).
- Anchored in behavior, not identity (“I procrastinate” is lazy; “I used to delay documentation…” is better).
- Includes what you do now to manage it.
Write tighter outlines for just these three. Practice them out loud 2–3 times each.
Step 9 (26:00–28:00) – Program-specific angle
Now, you adapt to the specialty / program type. Behavioral answers should already show alignment.
Ask:
- For internal medicine: Do your stories show curiosity, follow-up, ownership of patients, systems thinking?
- For surgery: Do they show calm under stress, team orientation in the OR, comfort with hierarchy, resilience?
- For pediatrics: Communication with anxious parents, patience, advocacy?
Tweak a few words in your stories so they naturally emphasize traits your specialty values. Not fake, just framed.
Hour 28–32: Do a real(er) mock interview
At this point you should do at least one full run. No pauses, no rewinds.
Step 10 (28:00–30:00) – Find a human or simulate one
Best options, ranked:
- Resident or fellow in your target specialty
- Classmate who is also interviewing (swap 30-minute sessions)
- Family member / friend with some hiring/interview experience
- Worst-case: yourself on Zoom, recording with camera on
Give them a list of 10–12 behavioral questions:
- “Tell me about a time you had a conflict on the team.”
- “Describe a situation where you made a mistake in patient care.”
- “Tell me about a time you went above and beyond for a patient.”
- “Describe a stressful situation and how you handled it.”
- “Tell me about a time you received critical feedback.”
- “Give an example of a time you had to lead without a title.”
- “Tell me about a time you worked with someone very different from you.”
Step 11 (30:00–32:00) – Run the mock and extract 3 fixes
Do a 25–30 minute mock. Then ask for specific feedback:
- Were any answers confusing or too long?
- Did I sound defensive in any story?
- Did I actually answer the question asked?
Pick only three concrete things to fix. Example:
- Shorten intros by 10 seconds
- Add explicit reflection line to conflict stories
- Stop saying “like” every 4 words
Then do one short repeat round (15–20 minutes) to try those corrections.
Hour 32–40: Polish, red-flag check, and curveball prep
Now you are moving from “good enough” to “tighter and safer.”
Step 12 (32:00–36:00) – Red-flag audit
You want to avoid accidentally sending the wrong signal. Go through your stories and ask brutally:
- Do any stories make me sound reckless, cavalier, or unsafe?
- Am I blaming someone else too much? (nurse, resident, attending, system)
- Is there any story where an interviewer could reasonably think: “This person will be a problem”?
If yes, either:
- Change which story you use for that theme
- Or reframe it to show more humility, insight, and shared responsibility
Especially watch:
- Stories about conflict with nurses (easy to sound condescending)
- Stories about calling out attendings (easy to sound naive / arrogant)
- Stories where patient harm occurred (must show seriousness and learning)
If something feels even slightly off, discard the story. You have other options.
Step 13 (36:00–38:00) – Prepare for classic curveballs
You do not need to spend hours here, but give 30–60 minutes to:
- “Tell me about yourself.” → 60–90 seconds: background, medical school focus, and why this specialty.
- “Why this specialty?” → 60–90 seconds anchored in experiences, not clichés.
- “Why our program?” → 60–90 seconds using specifics from their website / resident bios / tracks.
- “Anything else we should know about you?” → 30–60 seconds tying together themes from your stories.
These are not pure behavioral questions, but they set the frame. Sloppy answers here make the rest of your good prep look weaker.
Step 14 (38:00–40:00) – Quick mental reps
Do a rapid-fire drill:
Set a timer for 20 minutes. No recording. Just speed practice:
- Pick random behavioral questions from a list.
- Answer in 60–90 seconds.
- Move on, no rewinding.
This builds agility. Residency interviews are often fast and slightly awkward. You need to be able to pivot.
Hour 40–48: Light review, logistics, and mental reset
Last phase. At this point you should stop heavy drilling. Over-prepping right before makes you robotic and anxious.
Hour 40–44: Light review and visualization
Step 15 – One clean rehearsal of your core bank
Choose:
- 5 high-yield stories (leadership, conflict, failure, teamwork, stress)
- 3 core non-behavioral but related answers (“Tell me about yourself,” “Why this specialty,” “Weakness”)
Say each once out loud, without notes if possible. You are not aiming for perfection, just flow.
Then close the laptop.
Step 16 – Walk through the interview day in your head

Spend 10–15 minutes visualizing:
- Logging into Zoom / walking into the hospital
- Greeting the interviewer confidently
- Getting a behavioral question you recognize and answering smoothly
- Getting one you do not recognize and calmly asking for a second to think
This is not fluff. I have watched anxious students settle significantly after doing this.
Hour 44–46: Logistics and environment
At this point you should handle everything non-academic so you are not scrambling.
- Confirm interview time, platform, and time zone
- Check email for any program-specific instructions
- For virtual:
- Test camera, microphone, lighting
- Choose neutral background
- Charge laptop, have backup device nearby
- Lay out your outfit
- Print or open:
- Your ERAS PDF
- Short bullet list of your core stories by title only
- 3–5 questions you will ask them
Do a quick 2-minute tech test (Zoom or similar) checking framing and sound.

| Category | Value |
|---|---|
| Story review | 90 |
| Mock / speaking practice | 60 |
| Logistics & tech | 45 |
| Rest & sleep | 525 |
(Values in minutes; aim for most of your time to be sleep / rest, not last-second cramming.)
Hour 46–48: Stop. Sleep.
Last two hours before sleep:
- No new questions.
- No rewriting stories.
- Skim your story titles once. Close the file.
Then sleep like your performance depends on it. Because it does.
If nerves spike in bed:
- Mentally run one or two of your strongest stories start to finish, in STAR.
- Remind yourself: the stories are real. You already lived them. You are not fabricating anything, just organizing it.
Quick specialty-specific calibration (30-minute add-on if you have time)
If you are applying to multiple specialties or you want finer tuning, spend ~30 minutes doing this:
| Specialty | Emphasize in Stories |
|---|---|
| IM | Ownership, follow-up, systems |
| Surgery | Calm under pressure, hierarchy |
| Peds | Communication with families |
| EM | Rapid decision-making, triage |
| Psych | Listening, boundaries, insight |
Take 2–3 of your core stories and mentally highlight the angles that match your specialty. For example:
- EM: In your “stressful situation” story, emphasize triage, prioritization, and clear communication in chaos.
- Psych: In your “conflict” story, emphasize listening, validation, exploring others’ perspectives before responding.
Do not invent new stories. Just shift which parts you emphasize.
Final 10-minute pre-interview routine (day of)
You wake up. Interview in ~1–2 hours. Here is the last stretch:
- 5 minutes: Skim your story titles and their main themes.
- 3 minutes: Say out loud, once, “Tell me about yourself” and “Why this program.”
- 2 minutes: Deep breaths, slow exhale, relax shoulders.
Then you go in and have a conversation. Not a performance.
Key Takeaways
- In 48 hours, your priority is not learning more questions. It is organizing 8–10 real stories into clear STAR structures and mapping them to common behavioral themes.
- You should spend less time typing and more time speaking out loud, ideally with at least one short mock interview to expose your weak spots and fix 2–3 concrete issues.
- The last 12 hours are for light review, logistics, and sleep, not frantic rewriting. A rested brain with a solid story bank will outperform a burnt-out crammer every single time.




















