Navigating the Supplemental Offer and Acceptance Program (SOAP) can feel stressful for any applicant, and even more so for a DO graduate aiming for a competitive field like Interventional Radiology (IR). Preparing strategically—well before Match Week—can turn SOAP from a last‑minute scramble into a controlled, opportunity‑maximizing process.
This guide focuses specifically on SOAP preparation for a DO graduate interested in Interventional Radiology, including IR‑integrated programs, independent IR, and alternative pathways that keep your IR goals alive even if you don’t land IR right away.
Understanding SOAP: What It Is, How It Works, and Why It Matters
Before you can prepare effectively, you need a clear answer to “What is SOAP?” and how it fits into the residency match landscape.
What Is SOAP?
The Supplemental Offer and Acceptance Program (SOAP) is an organized, NRMP‑run process that allows eligible unmatched or partially matched applicants to apply to and receive offers from residency programs that did not fill all their positions after the Main Match.
Key points:
- SOAP happens during Match Week (Monday–Thursday).
- You can only apply to unfilled programs listed by NRMP in the SOAP system.
- Application is through ERAS; offers are made through the NRMP system in several rounds.
- Once you accept a SOAP offer, you are legally bound to that program and removed from further SOAP participation.
For a DO graduate, SOAP can open doors at ACGME‑accredited programs, including prelim or transitional year positions that can later support an Interventional Radiology pathway.
DO Graduate Residency Context: Why SOAP Strategy Is Critical
As a DO graduate, you already navigate several layers of complexity:
- Some programs remain more US‑MD‑favored (particularly in historically competitive fields like integrated Interventional Radiology).
- You may have COMLEX‑only scores or a combination of COMLEX and USMLE.
- You might experience more variability in how program directors interpret osteopathic training.
If you go unmatched or partially matched, SOAP becomes one of the most important opportunities to:
- Secure accredited training in a related pipeline specialty (e.g., Diagnostic Radiology, Internal Medicine, Surgery).
- Lock down a preliminary or transitional year essential for later IR opportunities.
- Avoid a gap year without clinical work, which can complicate future applications.
Understanding where SOAP could realistically lead you, given your credentials and IR goals, is the foundation of strong SOAP preparation.
Pre–SOAP Self‑Assessment: Know Your Profile and IR Options
Effective SOAP preparation for an osteopathic residency match in IR starts with an honest appraisal of your competitiveness and flexibility.
Step 1: Analyze Your Application Metrics
Create a concise snapshot of your profile:
- Board exams
- COMLEX Level 1/2/3
- USMLE Step 1/2 (if taken)
- Clinical performance
- Clerkship grades, especially in radiology, surgery, internal medicine, and ICU.
- Any sub‑internships (sub‑Is) or audition rotations.
- IR‑specific exposure
- Electives or rotations in Interventional Radiology.
- IR‑related research, QI projects, presentations.
- Letters of recommendation
- Any from Interventional Radiologists or Diagnostic Radiologists?
- Strength and specificity of comments.
- Red flags
- Exam failures.
- LOA (leave of absence).
- professionalism issues.
Be clear-eyed: IR‑integrated programs are among the most competitive in the country. However, being less competitive for integrated IR does not mean you cannot ultimately become an Interventional Radiologist.
Step 2: Identify Realistic IR‑Related Pathways
Before SOAP begins, define what “success” looks like if direct IR isn’t available in the IR match:
Integrated Interventional Radiology Residency (IR/DR)
- Direct pathway from PGY‑1.
- Offers a combined Interventional and Diagnostic Radiology curriculum.
- Highly competitive, and very few SOAP positions are typically available—if any.
Independent IR Residency (after Diagnostic Radiology)
- Requires completion of a Diagnostic Radiology residency.
- You match into DR first; then match into an IR‑independent position later.
- For SOAP: targeting DR, especially programs that are DO‑friendly, keeps IR possibilities alive.
Diagnostic Radiology → Future IR Fellowship/Pathway
- Even if the program does not advertise IR‑independent positions, strong DR training can set you up to be competitive for IR opportunities later.
Alternative Pathways (if DR/IR are unavailable)
- Internal Medicine → Interventional subspecialties (e.g., Interventional Cardiology, Vascular Medicine).
- Surgery → Vascular Surgery or procedures that share skill sets with IR.
- Anesthesia or Critical Care → Exposure to invasive procedures and imaging.
During SOAP, your primary objective may shift from “IR‑integrated or bust” to “securing a residency that preserves an IR‑adjacent future.”
Strategic SOAP Preparation for a DO Graduate Aiming for Interventional Radiology
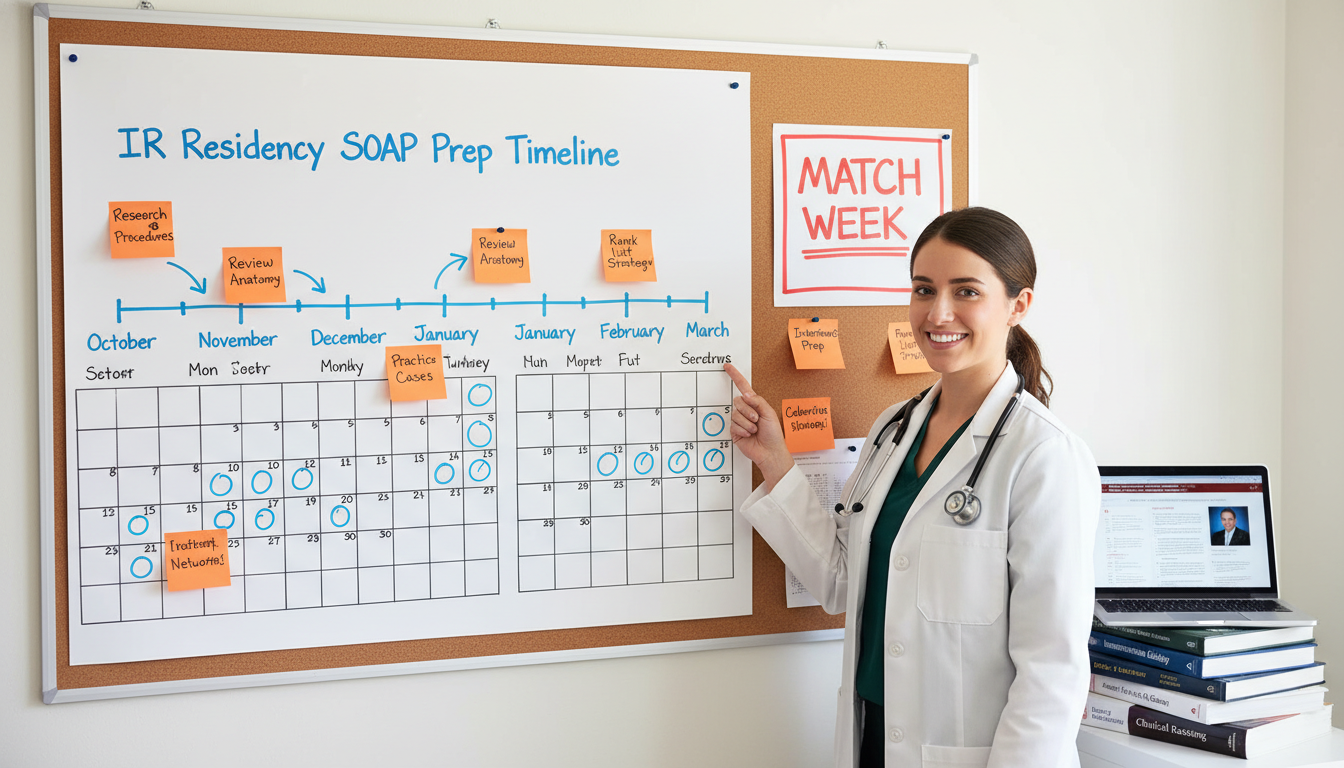
Build a Plan Before Match Week
SOAP success rarely comes from improvisation. You should have a written plan well before rank lists are due, and definitely before Match Week.
1. Understand SOAP Eligibility and Rules
Confirm with NRMP and your Dean’s office:
- That you are SOAP‑eligible (registered for the Main Match, with no contract violations).
- How many programs you will be allowed to apply to (currently up to 45 total during SOAP).
- That you cannot contact programs directly during SOAP unless they contact you first.
- That you must accept or reject offers within very short time windows during each round.
Keep a printed and digital copy of NRMP’s SOAP schedule and rules.
2. Clarify Your Preference Hierarchy
Rank your possible outcomes before emotion clouds your choices:
- Integrated IR programs (if any appear in SOAP).
- Diagnostic Radiology categorical programs.
- DR advanced programs plus a solid prelim/transition year.
- Transitional Year or preliminary year in Medicine or Surgery with IR exposure.
- Categorical positions in Internal Medicine, Surgery, or Anesthesia at institutions with strong IR services.
Write this out and share it with a trusted mentor so someone can remind you of your priorities when decisions come rapidly.
3. Align IR Goals with SOAP Reality
Recognize:
- Most Interventional Radiology residency (integrated or independent) spots fill in the main IR match.
- SOAP may have few or no IR‑integrated positions available in any given year.
- Some Diagnostic Radiology programs may appear on the unfilled list and are your best IR‑adjacent target.
Thus, a realistic SOAP strategy for a DO graduate IR aspirant often centers on:
- Casting a targeted net for Diagnostic Radiology positions that are DO‑friendly.
- Aggressively pursuing prelim/TY positions in hospitals with robust Interventional Radiology services.
- Keeping long‑term IR aspirations alive through networking and elective planning once you’re in any residency.
Tailoring Your Application Materials for SOAP
Your ERAS application will be re‑used during SOAP, but you can update key elements. Plan these changes ahead.
1. Personal Statement Strategy
Have two versions ready before Match Week:
Diagnostic Radiology / IR‑leaning personal statement
- Focus on:
- Your interest in image‑guided procedures.
- Cases or rotations with IR and DR that inspired you.
- Technical curiosity, procedural mindset, and teamwork in multidisciplinary care.
- Emphasize how you as a DO graduate bring:
- Holistic approach.
- Patient communication strengths.
- Osteopathic focus on function, pain, and quality of life.
- Focus on:
Transitional Year / Preliminary Medicine or Surgery statement
- Center on:
- Desire for broad clinical exposure.
- Goals of building a strong foundation for future IR or procedure‑heavy specialties.
- Your adaptability and commitment to patient‑centered care across settings.
- Center on:
During SOAP, you can assign these personal statements selectively to different program types.
2. IR‑Specific CV and Experiences
Highlight experiences that demonstrate an IR mindset:
- Procedural rotations: central lines, paracenteses, lumbar punctures, etc.
- IR shadowing or electives: number of weeks; specific procedures observed or assisted.
- Research:
- IR‑related projects (embolization, venous disease, oncologic interventions).
- Imaging, vascular, or minimally invasive therapy topics.
- Presentations or posters at SIR, RSNA, or local radiology/IR meetings.
- Osteopathic manipulative medicine (OMM) for pain and function—framed as complementary to minimally invasive procedural approaches.
Make sure your ERAS “Experiences” descriptions are updated and tightly written—SOAP programs often review applications very quickly.
3. Letters of Recommendation (LoRs)
You typically cannot add new letters during SOAP, but you can choose which to assign:
Priority for IR‑oriented SOAP applications:
- Letter from an Interventional Radiologist, if available.
- Letter from a Diagnostic Radiologist.
- Strong Medicine or Surgery letter emphasizing:
- Procedural skills.
- Clinical judgment.
- Resilience and teamwork.
If you anticipate SOAP early enough in the season, pro‑actively ask an IR or DR faculty member for a strong, specific letter that you can use across IR and DR applications.

Executing During Match Week: SOAP Tactics for DO IR Applicants
Once Monday of Match Week arrives, you’ll learn whether you are fully matched, partially matched, or unmatched. If you’re eligible for SOAP, the next steps are critical.
Step 1: Rapidly Analyze the Unfilled List
As soon as the NRMP releases the list of unfilled programs:
Filter by specialty:
- Interventional Radiology (rare).
- Diagnostic Radiology.
- Transitional Year.
- Preliminary Medicine, Preliminary Surgery.
- Categorical Internal Medicine or General Surgery at institutions known for strong IR.
Filter by geography and DO‑friendliness:
- Regions where DO graduates historically match (based on program websites, Charting Outcomes, or prior DO grads from your school).
- Institutions with a record of training DOs in Radiology/IR.
Create three tiers:
- Tier 1: DR programs and any IR‑integrated programs (if present) where you are plausibly competitive.
- Tier 2: TY/prelim programs at institutions with robust IR services or DR residencies.
- Tier 3: Categorical IM/Surgery programs at academic centers with IR departments.
Use your dean’s office or advisors to help with this triage quickly; you will be under time pressure.
Step 2: Allocate Your 45 Applications Strategically
For a DO graduate pursuing an IR match or IR‑adjacent path, a sample SOAP distribution might look like:
- 10–15 applications to Diagnostic Radiology programs that:
- Have current or prior DO residents.
- Are community‑based or hybrid academic‑community (often more DO‑friendly).
- 10–20 applications to Transitional Year and preliminary Medicine/Surgery programs at:
- Hospitals with IR fellowship or integrated IR residents.
- Institutions with strong DR departments.
- 10–15 applications to categorical Internal Medicine or General Surgery at:
- Centers known for robust Interventional Radiology services, vascular surgery, or complex oncologic care.
Be realistic—if your metrics are significantly below typical DR thresholds, increase your emphasis on TY/prelim and categorical IM opportunities.
Step 3: Prepare for Accelerated Communication and Interviews
During SOAP, programs may:
- Contact you via email or phone to schedule rapid virtual interviews.
- Conduct short, focused interviews (10–20 minutes) with program directors or chief residents.
SOAP Interview Preparation
Have a concise framework ready for common questions:
“Tell me about yourself.”
- 1–2 minute narrative:
- Background → DO training → key IR/DR experiences → what you’re seeking in residency.
- 1–2 minute narrative:
“Why Diagnostic Radiology / this specialty?”
- Emphasize:
- Love for imaging and problem‑solving.
- Interest in procedures (if DR/IR).
- Value of noninvasive diagnosis and longitudinal patient impact.
- Emphasize:
“You’re interested in IR. Why are you applying to our TY/prelim/IM/Surgery program?”
- Response structure:
- Acknowledge IR interest honestly.
- Explain that you value strong clinical foundation.
- Highlight their hospital’s IR/DR department and multi‑disciplinary care environment.
- Clarify that you will be a committed, engaged resident in any role you accept.
- Response structure:
“What happened in the main Match?”
- Be honest but concise:
- “IR and DR are highly competitive. I targeted a narrow list because of my strong interest in X. While I didn’t match, I remain deeply committed to training, and I’m excited about the opportunities SOAP provides—particularly at a program like yours where I could build a strong foundation.”
- Be honest but concise:
Avoid defensiveness or blame; focus on readiness to work hard wherever you match.
Long‑Term IR Strategy If You Match Through SOAP
Landing your dream IR‑integrated program via SOAP is unlikely but not impossible. More commonly, a DO graduate will secure a DR, TY/prelim, or categorical IM/Surgery position. The key is to keep the IR pathway alive once you’re in training.
If You SOAP into Diagnostic Radiology
You are in an excellent position to pursue:
- Independent IR residency after DR.
- IR‑focused rotations during radiology residency.
- Participation in IR call, conferences, and research.
Action items:
- Seek an IR mentor at your institution early (PGY‑2).
- Plan IR electives and research projects.
- Attend SIR (Society of Interventional Radiology) meetings if possible.
- Build a reputation as a hard‑working, teachable DR resident—program directors talk.
If You SOAP into Transitional Year or Preliminary Year
Use this year as a launch platform:
- Request rotations with:
- Interventional Radiology.
- ICU and step‑down units (IR closely collaborates here).
- Surgical subspecialties and vascular services.
- Maintain close communication with your home med school and prior IR mentors about:
- Reapplying to DR or IR the following cycle.
- Securing updated letters that reflect your performance during the TY/prelim year.
This path can significantly strengthen your application for the next match cycle, especially if your clinical performance and professionalism are outstanding.
If You SOAP into Categorical IM or Surgery
You have several options:
- Fully commit to your new specialty and pursue interventional subspecialties:
- Interventional Cardiology, Vascular Medicine, Endovascular Surgery, etc.
- Keep a door open to future IR if:
- You build strong imaging and procedural experience.
- You maintain relationships with IR/DR faculty.
- You remain open to complex and potentially non‑traditional pathways (though transitions later can be challenging and are not guaranteed).
Whatever path you follow, success in residency—and ultimately in any interventional field—depends heavily on your professionalism, work ethic, and reputation as a colleague.
Practical Tips and Common Pitfalls for DO Graduates in SOAP
Actionable Tips
Engage Your Dean’s Office Early
- Meet with your Student Affairs or GME advisors before rank list submission.
- Ask specifically: “If I go unmatched, what does strong SOAP preparation look like for me as a DO aiming for IR?”
Know Your DO‑Friendly Programs
- Ask prior graduates which DR and TY/IM/Surgery programs have historically welcomed DOs.
- Cross‑reference with unfilled lists as soon as SOAP opens.
Set Up Your Technology
- Reliable internet, camera, microphone, and a neutral backdrop for rapid‑fire virtual interviews during SOAP.
- Keep a professional outfit ready for last‑minute video calls.
Have Talking Points for DO‑Specific Questions
- If asked about osteopathic training:
- Emphasize holistic viewpoint, early clinical exposure, hands‑on skills, and communication.
- Bridge this to IR: “These strengths help me connect with patients undergoing minimally invasive procedures and manage complex, longitudinal conditions like PAD or cancer.”
- If asked about osteopathic training:
Take Care of Yourself
- SOAP is intense and emotionally draining.
- Schedule short breaks and maintain sleep as much as possible—clear thinking improves your decision‑making under pressure.
Common Pitfalls to Avoid
Chasing only IR‑integrated spots
If no realistic IR‑integrated positions are in SOAP, do not waste most of your 45 applications on unreachable goals. Secure any strong IR‑adjacent pathway.Ignoring transitional and prelim options
A solid TY/prelim year at a strong teaching hospital can transform your competitiveness for the next cycle.Under‑communicating with mentors
Your IR or DR mentors can:- Advocate on your behalf.
- Help you interpret unfilled program reputations.
- Give you honest feedback about your competitiveness.
Emotional decision‑making in offer rounds
Review your pre‑written priority list before each acceptance window opens. If necessary, involve a trusted advisor before you accept.
FAQs: SOAP Preparation for DO Graduates Targeting Interventional Radiology
1. As a DO graduate, is it realistic to match into Interventional Radiology directly through SOAP?
Directly matching into an integrated IR residency through SOAP is rare for any applicant, MD or DO, because most IR positions fill in the main IR match. A DO graduate residency match into IR‑integrated via SOAP is possible but should be seen as a bonus outcome, not your primary expectation. Instead, prioritize Diagnostic Radiology, Transitional Year, and strong prelim positions that keep an IR‑aligned future open.
2. How should I balance applications between DR, TY/prelim, and categorical IM/Surgery during SOAP?
Base it on your competitiveness and the unfilled list, but a common approach:
- Start with all reasonable DR programs that look DO‑friendly.
- Add TY and prelim spots at hospitals with active IR/DR departments.
- Use remaining slots on categorical IM/Surgery at institutions with strong interventional services.
You want a range of options so you don’t end SOAP without a position, while still keeping your IR goals in view.
3. If I accept a TY or prelim spot in SOAP, can I realistically reapply to IR or DR later?
Yes. Many residents use a TY or prelim year to strengthen their application and reapply for DR (and later IR). Success depends on:
- Excellent performance and evaluations in your TY/prelim program.
- Establishing mentorships with Radiology/IR faculty.
- Updating your application with stronger letters, more clinical experience, and possibly research.
This is a viable bridge strategy, particularly for DO graduates whose initial osteopathic residency match aspirations in IR didn’t materialize.
4. What is SOAP preparation I can do now if I’m still months away from Match Week?
You can:
- Clarify your IR and DR goals and backup pathways.
- Meet with your Dean’s office about SOAP logistics.
- Update ERAS experiences and prepare two personal statements (IR/DR‑focused and TY/IM/Surgery‑focused).
- Confirm that your letters of recommendation include at least one from IR or DR.
- Research DO‑friendly DR and TY/IM programs, especially those with strong IR services.
- Set up your technology and a quiet space ready for virtual SOAP interviews.
Thorough SOAP preparation doesn’t guarantee you an IR‑aligned position, but it dramatically increases your odds of landing a residency that keeps your Interventional Radiology goals within reach.





















