
Preparing for the Supplemental Offer and Acceptance Program (SOAP) can feel daunting—especially in a competitive field like urology. But strategic, early preparation can transform SOAP from a crisis into an opportunity to secure a strong training position and keep your long-term goals on track.
This guide walks you through everything you need to know about SOAP preparation in the context of the urology residency match: timelines, documents, communication strategy, mindset, and how to keep your urology aspirations alive even if you ultimately match into a different specialty through SOAP.
Understanding SOAP in the Context of Urology
Before you can prepare effectively, you need to understand what SOAP is and, just as importantly, what it is not—particularly for a urology applicant.
What is SOAP?
SOAP (Supplemental Offer and Acceptance Program) is an NRMP-organized process that allows eligible unmatched or partially matched applicants to pursue unfilled residency positions during Match Week.
Key points:
- It occurs during Match Week (usually Monday–Thursday).
- It is completely electronic via ERAS and NRMP.
- Applicants may apply to up to 45 programs total during SOAP.
- Programs review, interview (often virtually), and offer positions in a series of rounds.
- Positions offered through SOAP are categorical or preliminary PGY-1 slots (and sometimes advanced positions in non-urology specialties).
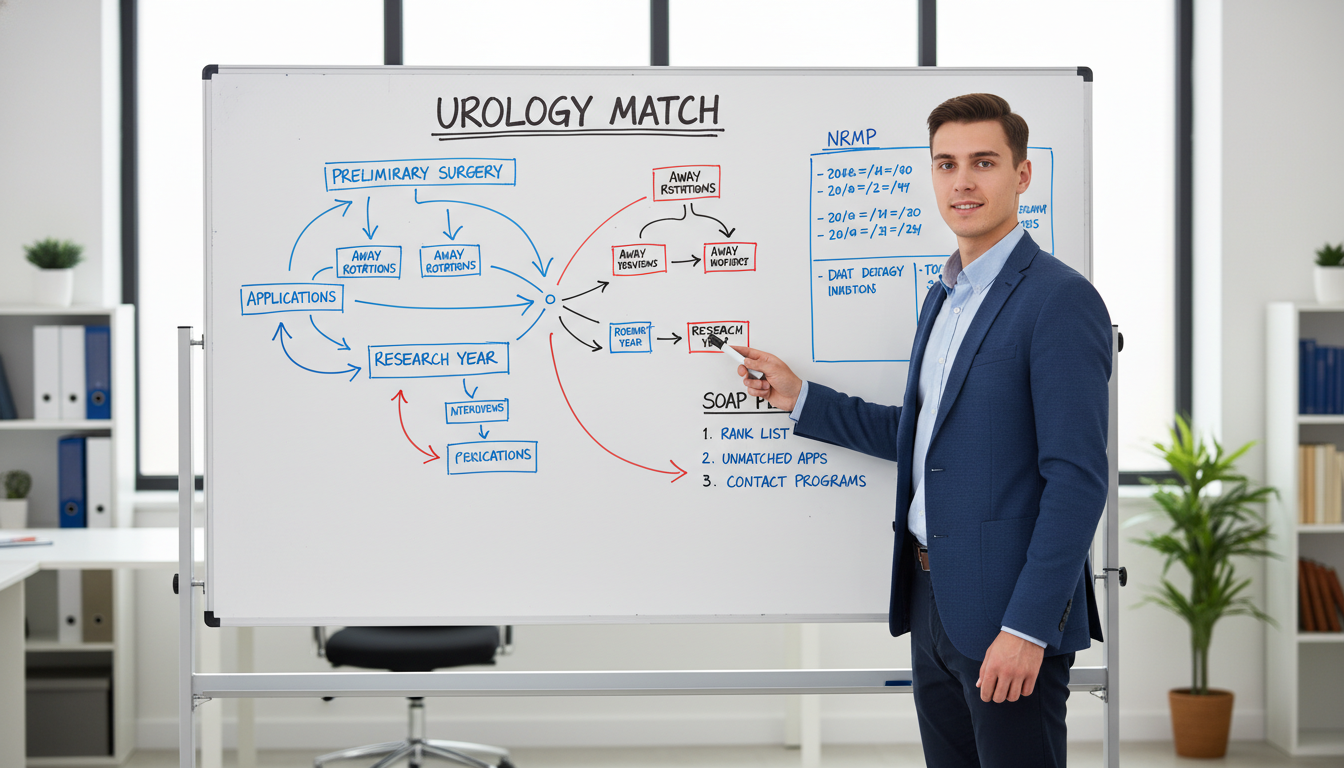
Urology Match vs Main NRMP Match
Urology is unique because it uses a separate match (organized by the AUA, though many elements use ERAS). That creates two distinct phases:
Urology Match (AUA Match)
- Typically concludes several months before the NRMP Main Match.
- You may find out you are unmatched in urology well before NRMP rank list deadlines.
- You then decide whether to:
- Enter the NRMP Match in another specialty, or
- Sit out a year and reapply in urology.
NRMP Main Match & SOAP
- If you participate in the NRMP Match and do not match, you may become eligible for SOAP.
- SOAP then becomes your rapid pathway to obtain a PGY-1 position.
Critical implication for urology applicants:
SOAP positions in urology essentially do not exist. SOAP is primarily a way to secure non-urology PGY-1 spots (preliminary surgery, internal medicine, transitional year, etc.) after an unsuccessful main match. For a urology-focused applicant, SOAP is about answering:
“How can I secure a solid PGY-1 position that keeps me competitive and flexible for a future urology application (or re-application)?”
Who Is Eligible for SOAP?
SOAP eligibility is determined by the NRMP, not the AUA. In simplified terms, you must:
- Be registered for the Main NRMP Match.
- Be unmatched or partially matched after the initial algorithm.
- Be eligible to start residency on July 1 (graduation, exams, visas, etc.).
- Not have accepted a matched position outside NRMP that would start at the same time.
Urology-specific nuance:
- If you matched into urology via the AUA match, you are not participating in SOAP.
- If you did not match in urology and chose to apply to other specialties through NRMP, you may enter SOAP if you go unmatched there.
Strategic Planning: Before You Ever Reach SOAP
Effective SOAP preparation for urology starts months before Match Week—often before you submit a single application.
1. Build a Parallel Plan Early
You should think in terms of Plan A and Plan B:
- Plan A: Match in urology residency.
- Plan B: Secure a position through NRMP or SOAP that:
- Provides strong clinical training and
- Adds value for a future urology application.
Common Plan B paths for future urology re-applicants:
- Preliminary general surgery
- Transitional year
- Preliminary internal medicine (less ideal but still workable)
- Dedicated research year (not via SOAP, but a separate option)
Ask yourself early:
- “If I don’t match urology, which alternate fields or PGY-1 structures would best support a later urology application?”
- “Which specialties would I realistically be content training in if I ultimately do not return to urology?”
This mindset helps you choose NRMP specialties and programs wisely and sets you up to use SOAP intentionally, not reactively.
2. Understand Program Perspectives
Programs reviewing SOAP applications are often looking for:
- Applicants who can hit the ground running on July 1.
- Evidence of professionalism, resilience, and maturity.
- Clear interest in their specialty or program, even if you’re coming from a urology background.
They are not necessarily concerned that you previously pursued urology; many program directors understand the competitiveness of the urology match. However, they want reassurance that:
- You will show up fully committed.
- You won’t be disengaged or “checked out” during the year.
- You respect their specialty and are not treating it as a disposable backup.
3. Clarify Your Long-Term Goal
There are three realistic trajectories:
- SOAP into a PGY-1 that you plan to complete, then re-apply in urology.
- SOAP into a specialty you’d be happy to pursue long term if urology does not materialize.
- Pause residency, pursue research or further clinical exposure, and re-apply later (outside SOAP framework).
Your SOAP strategy—what programs you target, how you present your story, what you emphasize in personal statements—should align with the trajectory you’d accept as your future.
Document & Logistics Preparation for SOAP
SOAP unfolds extremely quickly. Most of the “work” is actually done before Match Week—if you prepare correctly.
Core Documents to Have Ready
Updated CV
- Include:
- All clinical experiences, especially surgical and urology rotations.
- Research (urology and otherwise), including posters and abstracts.
- Leadership roles (e.g., surgery/urology interest groups, QI projects).
- Save as a standalone PDF in case a program requests it separately from ERAS.
- Include:
SOAP-Ready Personal Statements
Because you can only upload a limited number of personal statements in ERAS and SOAP moves quickly, you should have multiple tailored versions ready:
A general SOAP personal statement:
- Focused on resilience, adaptability, teamwork, and your growth as a clinician.
- Less specialty-specific; can be used broadly.
Specialty-specific versions, such as:
- Preliminary General Surgery PS
- Transitional Year PS
- Internal Medicine PS (if relevant)
For each:
- Explain authentically why this particular experience (prelim year or TY) makes sense for you.
- If you intend to re-apply in urology, you do not need to hide it—but frame it carefully:
- Emphasize the skills you’ll gain (operative fundamentals, perioperative management, critical thinking) that will make you a better urologist (or surgeon/physician in general).
- Reassure programs that you will be a fully engaged and reliable team member regardless of your long-term plans.
- Letters of Recommendation (LoRs)
Aim to have:
- At least 3–4 strong letters in ERAS by the main application season:
- Ideally:
- One from a urologist.
- One from a general surgeon or surgical service.
- One from a non-surgical core faculty, e.g., internal medicine, if relevant.
- Ideally:
- These same letters can be used during SOAP—so you want them to be broadly positive and versatile, not hyper-specialized to urology only.
If you know you’re at higher risk for not matching (limited interview numbers, weaker exam history), consider:
- Asking a surgical faculty member (outside urology) to write a more general letter that speaks to your operative potential and work ethic.
- USMLE/COMLEX and MSPE
- Confirm all scores are released and visible in ERAS ahead of Match Week.
- Review your MSPE for any potential red flags or wording issues so you are prepared to discuss them coherently if asked during SOAP interviews.
- Program List Templates
You will need to move very quickly once the List of Unfilled Programs is released. Prepare:
A spreadsheet with:
- Program names by specialty.
- Columns for:
- Location
- Program type (prelim surgery, TY, IM prelim, etc.)
- Historical reputation (if you know it)
- Prior alumni presence or known contacts
- “Fit” score (you can assign 1–5 informally)
Build draft priority lists for:
- Preliminary general surgery programs.
- Transitional year programs.
- Any other specialties you could realistically accept.
This framework lets you plug in unfilled programs rapidly during SOAP.
Step-by-Step: How to Navigate SOAP Week as a Urology Applicant
1. Monday: Confirm SOAP Eligibility & Emotional Reset
On Monday of Match Week, at 11 a.m. ET, you learn whether you are:
- Matched
- Partially matched
- Unmatched
If you’re unmatched or partially matched and NRMP deems you SOAP-eligible, your status will reflect that.
Your first tasks:
Breathe and stabilize emotionally.
It is entirely normal to feel stunned, ashamed, or anxious. Take 2–3 hours to:- Talk to a trusted friend, mentor, or family member.
- Step away from your computer briefly.
- Remind yourself: this is a detour, not a dead end.
Contact key advisors.
- Your Dean’s Office / Student Affairs.
- A trusted urology mentor.
- A career advisor or program director from your home institution. Ask specifically:
- “Given my profile, which types of SOAP programs should I prioritize?”
- “Would you be willing to speak on my behalf if a program contacts you quickly?”
Get clarity on your long-term aim.
- Do you still strongly intend to pursue urology later?
- Are you open to settling into a different specialty if SOAP provides that opportunity? Your answers will shape your SOAP ranking of prelim vs categorical positions.
2. Monday Midday: Review Unfilled Positions & Build Your Target List
NRMP releases the List of Unfilled Programs to SOAP-eligible applicants.
Actions:
Filter by program type relevant to your goals, such as:
- Preliminary General Surgery: Often best aligned with future urology.
- Transitional Year: Offers broad exposure and time for research, sometimes with lighter call.
- Preliminary Internal Medicine: Less ideal but still clinically valuable.
- Categorical positions in fields you’d be ok with as a long-term career (e.g., anesthesia, internal medicine, family medicine).
Apply your pre-made spreadsheet framework.
- Add new unfilled programs to your sheet.
- Quickly categorize as:
- High priority
- Medium priority
- Low priority / unlikely
Consider geography and support systems.
- A tough, intense prelim year can be more tolerable if you have family or friends nearby.
- Proximity to research institutions with urology departments can also be strategic for future networking.
3. Monday–Tuesday: Submitting SOAP Applications
Remember:
- You may submit a total of up to 45 program applications during SOAP.
Best practices:
- Prioritize quality over sheer number—45 is a limit, not a goal.
- Make sure your personal statement matches the program type:
- Prelim surgery programs should receive your prelim surgery PS, not a generic or IM-focused one.
- Double-check:
- LoRs assigned properly.
- Correct CV and documents linked.
- No mention of program names in your PS that could conflict with different institutions.
If you’re torn between maximizing prelim surgery vs categorical positions in a different field:
- Ask yourself honestly: “If I never become a urologist, which path would I most regret not pursuing?”
- Many urology re-applicants find prelim surgery the most aligned with future urology, but:
- A strong categorical spot in another specialty can also be a great long-term career.
4. Tuesday–Thursday: Interviews & Offers
During SOAP, programs may contact you by:
- ERAS messaging
- Phone call
- Virtual interview invites (often very short and scheduled on short notice)
Key restrictions:
- You may not initiate contact with programs outside allowed mechanisms.
- You must follow NRMP rules on communication—violations can jeopardize your ability to participate.
SOAP Interviews: How to Present Yourself as a Urology Applicant
Anticipate questions like:
- “I see you applied to urology—what brings you to our program now?”
- “How committed are you to our specialty or prelim year?”
- “If you plan to re-apply in urology, how do you see this year fitting into your trajectory?”
Answer structure:
Acknowledge your prior goal clearly and without shame.
- “Yes, I applied to urology this cycle and unfortunately did not match.”
Express respect for their specialty/program.
- “I have a strong interest in operative care and perioperative medicine, and your prelim surgery program offers the exact kind of rigorous training that will make me a stronger physician.”
Articulate how their position fits your development.
- “This year would allow me to deepen my operative skills, manage complex surgical patients, and contribute to the team while I reevaluate or potentially re-apply in urology.”
Reassure them about your engagement.
- “Whether I ultimately continue in urology or another field, I am fully committed to giving everything I have to this program and to patient care this year.”
If interviewing for a categorical non-surgical specialty, adjust language:
- “While my initial interest was in a procedural surgical field, I’ve consistently enjoyed my internal medicine rotations, particularly complex diagnostic reasoning and longitudinal patient relationships. If I’m fortunate to join your program, I’d be committed to internal medicine as a primary career path, not just a placeholder.”
Programs may also explore:
- Red flags (exam failures, gaps, professionalism concerns).
- Resilience and coping with disappointment.
- How you function in high-stress or high-volume environments.
Stay honest, accountable, and focused on growth and learning rather than blame.

Maximizing a SOAP Outcome for a Future in Urology
Matching into a non-urology position through SOAP does not end your urology aspirations. Many successful urologists took indirect paths.
Choosing the Best SOAP Position for Future Urology
If your overriding goal is to re-apply in urology, a preliminary general surgery year is often the most synergistic because it:
- Delivers intensive OR experience and surgical floor management.
- Demonstrates that you can handle surgical residency workload.
- Provides strong surgical faculty advocates for future letters.
A transitional year can also be valuable, especially if:
- It includes elective time you can use for urology rotations or research.
- It has a supportive environment that allows you to excel academically and clinically.
Less directly aligned but still useful options:
- Preliminary internal medicine
- Categorical positions in anesthesia or radiology (if you might pivot away from urology long-term)
How to Use Your PGY-1 Year Strategically
Once you SOAP-match into a PGY-1 spot:
Excel Clinically
- Show up prepared and early.
- Be reliable, good-humored, and professional.
- Offer to help with cases, notes, pre-op/post-op management. Strong evaluations from your PGY-1 year can significantly boost your candidacy if you re-apply.
Build Relationships with Surgical and Urology Faculty
- Identify surgeons or urologists at your institution who are open to mentoring.
- Ask for opportunities to:
- Scrub into urology cases when your schedule allows.
- Participate in urology research or QI projects.
- Be very respectful of duty hour rules and your primary program’s expectations.
Plan the Timing of Your Re-Application
- Many urology re-applicants:
- Start planning in late PGY-1 (or early research year, if they take one).
- Coordinate with their program director about logistics and references.
- It’s crucial to maintain transparent and professional communication with your primary residency about your intentions, especially if you will later depart.
- Many urology re-applicants:
Consider a Dedicated Research Year (If Needed)
- If you SOAP into a preliminary position without a guaranteed PGY-2 spot:
- A subsequent research year in urology at an academic center can be powerful.
- This is especially beneficial if:
- You lack prior urology publications.
- You need stronger networking and mentorship within the field.
- If you SOAP into a preliminary position without a guaranteed PGY-2 spot:
Guarding Your Well-Being and Mindset
It is easy to let a SOAP outcome feel like a permanent judgment on your worth. It is not.
- Many urology colleagues, including residents and attendings, have non-linear paths:
- Prior prelim years.
- Research fellowships.
- Initially matching in another field before transitioning.
- Focus on:
- Skill acquisition
- Relationships
- Professional growth
- Being someone others want to work with and support
These qualities matter as much as board scores in the long run.
Common Pitfalls in SOAP (and How to Avoid Them)
1. Waiting Too Late to Plan
Pitfall: Hoping everything will work out in urology and doing zero preparation for alternative paths.
Solution:
- Start SOAP preparation when you:
- Receive few urology interview invites, or
- Have significant red flags.
- Quietly develop:
- Alternative personal statements.
- A list of potentially compatible specialties/program types.
- Relationships with non-urology mentors who could champion you in SOAP.
2. Over-Focusing on Prestige
Pitfall: Only applying to “top-tier” prelim or TY programs, ignoring geography or realistic competitiveness.
Solution:
- SOAP is about securing a strong, workable position, not prestige labels.
- A mid-tier program with:
- Supportive leadership,
- Reasonable workload, and
- Opportunities for mentorship can be far more valuable than a “big name” program where you are anonymous and unsupported.
3. Underselling Your Urology Experience
Pitfall: Hiding your urology attempts, fearing it will hurt your SOAP chances.
Solution:
- Present your urology interest as evidence of:
- Commitment to procedural and operative care.
- Experience in complex clinical decision-making.
- Clarify that:
- You respect all specialties.
- You will give your full effort to any program that accepts you.
4. Poor Communication During SOAP
Pitfall: Being disorganized, slow to respond, or overly aggressive in messages.
Solution:
- Check email/ERAS frequently during SOAP days.
- Answer calls professionally (even unknown numbers).
- When messaging programs:
- Keep it concise, professional, and error-free.
- Avoid emotional or desperate tones.
FAQs: SOAP Preparation for Urology Applicants
1. If I don’t match into urology, should I always try SOAP, or is a research year better?
It depends on your profile and priorities:
SOAP into a prelim surgery or TY is often better if:
- You want to start residency immediately.
- You already have some urology research and need more clinical credibility.
- You prefer income and structured training over a pure research position.
A dedicated research year may be better if:
- Your application lacks urology publications, strong letters, or evidence of commitment.
- You can work with a high-impact urology mentor.
- You are comfortable delaying clinical training to build a more competitive file.
Discuss this with your urology mentors and Dean’s Office; the best choice is highly individual.
2. Will programs be turned off that I “failed” to match urology?
Most program directors understand:
- Urology is extremely competitive.
- Many strong applicants go unmatched each year due to numbers, not quality.
They will be more concerned about:
- Your attitude (do you show humility and maturity?).
- Your work ethic and team orientation.
- Whether you can clearly articulate why their program makes sense for you now.
Frame your unmatched status as:
- A disappointment that you’ve reflected on, and
- A catalyst for growth, not a source of bitterness.
3. Can I re-apply to urology while in a categorical program from SOAP?
Yes, but you must handle it carefully:
- You owe your categorical program honest and professional communication once you are seriously considering leaving.
- Some programs will be supportive of your re-application; others may not.
- If you match into urology while holding a categorical contract, you must:
- Coordinate a mutually respectful departure, and
- Follow all NRMP and institutional policies.
If you think re-applying is likely, a prelim surgery year is often simpler logistically than leaving a categorical spot—though both can be navigated if handled maturely.
4. How many programs should I apply to in SOAP, and how do I decide the mix?
You may apply to up to 45 programs. Many applicants use 30–45 applications, focusing on:
- A majority of prelim surgery or TY if aiming to re-apply to urology.
- A smaller subset of categorical programs in another field if open to a different long-term career.
Choose based on:
- Your competitiveness (exam scores, academic record).
- Your geographic flexibility.
- Your long-term plan:
- 100% committed to re-apply to urology → more prelim/TY.
- Open to alternate careers → mix in more categorical positions.
Preparing for SOAP as a urology applicant is fundamentally about planning for uncertainty with clarity and purpose. If you recognize your risk level early, assemble thoughtful documents, engage mentors, and maintain a resilient mindset, you can turn a difficult week into a meaningful start to your career—whether that ultimately leads back to urology or toward another fulfilling specialty.





















