
The biggest residency regret usually was not a surprise. The red flags were there. You just chose to ignore them.
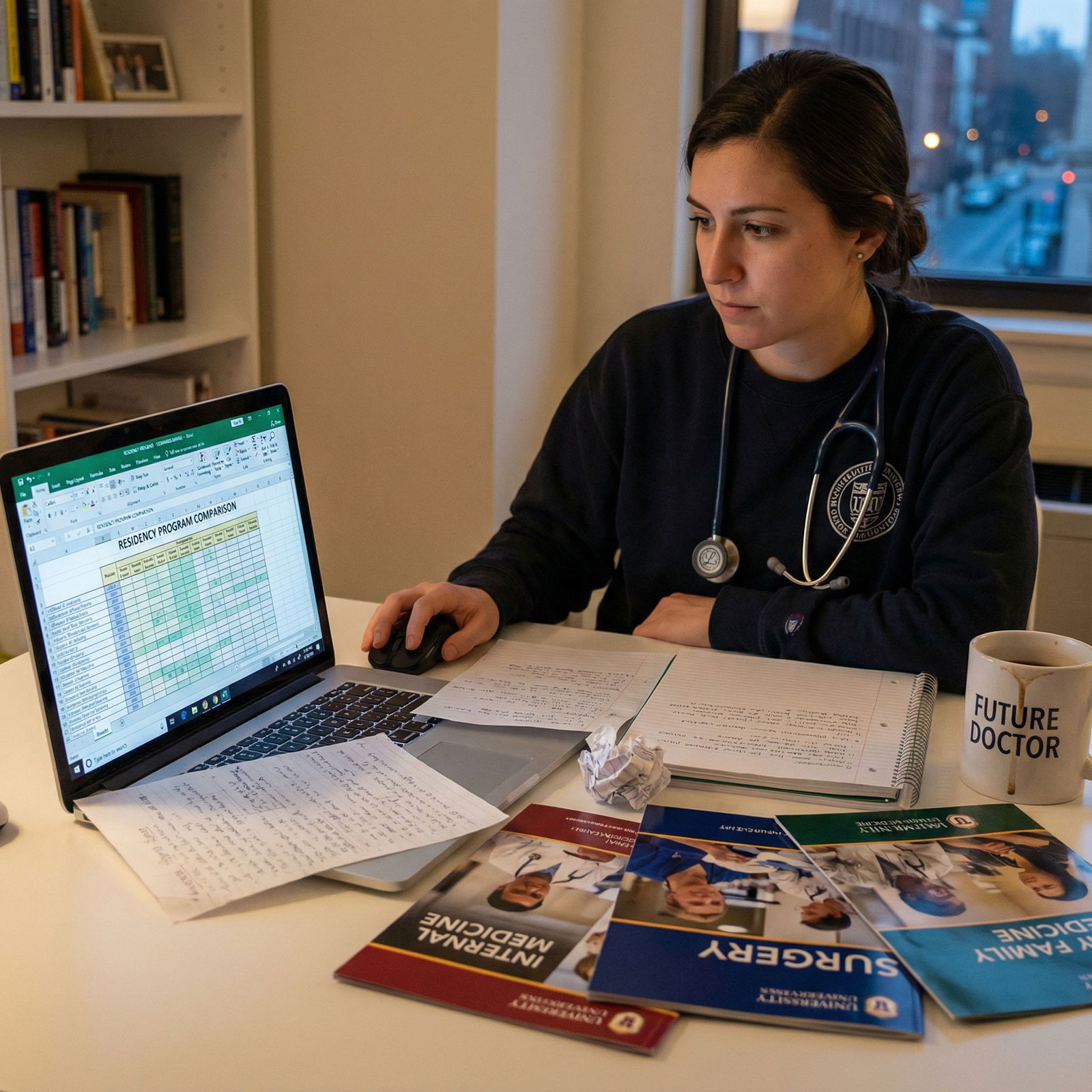
Let me be blunt: applicants spend hundreds of hours perfecting ERAS and maybe 10 minutes seriously evaluating how a program might destroy their sleep, their confidence, or their career trajectory. That is backwards.
You are not just matching to a name. You are matching to a culture, a workload, a set of expectations, and a leadership style that will shape the next 3–7 years of your life. If you miss the warning signs now, you will pay for them at 2 a.m. on call when no one is answering their pager and you realize: “Oh. This was not an accident. This is how this place works.”
Below are 10 residency red flags applicants routinely ignore until it is too late—and how to avoid being one of them.
1. Residents Look Exhausted… and Flat
There is a difference between tired and defeated. Do not confuse them.
Every program will tell you they “take wellness seriously.” Ignore the words. Look at faces.
Red flags during your visit or virtual interactions:
- Residents with dark circles, slumped posture, emotionally flat
- Jokes that are a little too bitter: “You’ll never see your family again… haha…”
- Residents who answer honestly only when faculty leave the room
- Forced enthusiasm that collapses the second they think they are off-camera / off-mic
I have seen this play out at morning report. An applicant asks, “How are the hours?” Faculty smiles and answers for the residents. That is not a minor thing. That is control.
What you should do instead:
- Ask residents privately: “How many days off did you actually get last month?”
- Ask a senior: “How often do you violate duty hours, honestly?”
- Watch for subtle behavior: Do residents check the time constantly? Whisper about “getting back to the floors”? Apologize for “complaining too much”?
If everyone seems numb or hyper-cynical, do not pretend you will be different. You won’t. Culture eats optimism for breakfast.
2. Vague Answers About Duty Hours and Call
If you ask, “What are the hours like?” and get a 2-minute ramble with no numbers, you just got your answer: it is bad.
Specific red flags:
- “We work hard but we play hard” (translation: you will work more than you should)
- “It varies a lot, it’s hard to say” (translation: the schedule is unpredictable and often unreasonable)
- “We are technically within duty hours” (translation: people are routinely charting off the clock)

| Category | Value |
|---|---|
| Program A | 60 |
| Program B | 70 |
| Program C | 80 |
| Program D | 90 |
What you actually need to know:
- Average weekly hours on wards, ICU, and clinic
- Frequency of 24-hour or “short” calls
- Night float structure and how many consecutive nights
- Real post-call protection or “just finish up a few things”
And you need numbers, not vibes.
Ask residents:
- “How many hours did you work on your last ICU week, door-to-door?”
- “When you violate duty hours, what happens? Is it ignored? Are you told not to log them?”
If people laugh nervously or dodge, that is not shyness. That is a red flag. Duty hours are a safety issue, not just a comfort issue.
3. High Resident Turnover or Transfers
Residents rarely transfer without a very good reason. When multiple residents have left or changed programs, your alarm bells should be going off.
Concrete signs:
- You see “PGY-3” slots filled with new names every year
- Residents say things like, “We had someone leave, but it was not a good fit”
- They talk about “restructuring” after “feedback,” but current residents still seem unhappy
| Sign | Why It Matters |
|---|---|
| Multiple recent transfers out | Probably systemic problems, not just one bad fit |
| Unexpected open positions | Residents may have quit or been pushed out |
| Frequent recruitment mid-year | Indicates instability and poor planning |
| Defensive responses about attrition | Leadership may be hiding deeper issues |
Applicants love to rationalize:
- “Maybe those residents just wanted a different city”
- “Every program has someone leave”
- “At least it opened up a spot for me”
Do not do this. One transfer is unfortunate. Several in a short period is a pattern. Programs that consistently retain residents are doing something right. Programs that leak residents are usually doing the opposite.
Questions to ask:
- “Has anyone transferred out recently? What led to that?”
- “How many residents have left in the last 5 years before graduation?”
If they refuse to answer directly or pivot immediately, note that. And walk carefully.
4. No One Can Explain How Feedback or Remediation Works
You will make mistakes. You will struggle with something. A good program has a clear, humane process. A bad program has… vibes and fear.
Red flags:
- Chiefs or PD say “We are a family” when you ask about remediation. That is not an answer.
- No one can describe a structured feedback process (who meets with whom, when, how it is documented)
- Residents talk about “getting in trouble” rather than “getting support”
- You hear “We do not really put people on formal remediation” (translation: we quietly punish people instead)
Ask specifically:
- “If someone is struggling clinically, what happens?”
- “How often do you get formal feedback? Is it useful or just checkboxes?”
- “Has anyone been on remediation? How did that go for them?”
If residents look nervous about answering or glance at faculty before speaking, that is your cue. Programs that cannot talk openly about remediation often use it as a weapon instead of a tool.
5. Toxic Faculty or Bullying That Everyone Laughs Off
Every resident can name that attending. The difference between a survivable environment and a dangerous one is what happens next.
Do they:
- Roll their eyes and say, “Yeah, Dr. X is like that, but we do not tolerate abuse here”
- Or laugh and say, “You just have to survive that rotation, everyone gets yelled at”
Warning signs:
- Residents share “horror stories” as if they are just a normal rite of passage
- Faculty openly belittle residents during conference, and no one intervenes
- PD or APD jokes about “being tough” or “not everyone is cut out for this” when you ask about mistreatment

Do not ignore this because the program is “prestigious.” Prestige will not help you when your confidence is destroyed and you dread coming to work.
You want to hear:
- Specific reporting mechanisms
- Examples of bad behavior being addressed
- Residents who feel safe giving upward feedback
If everyone just shrugs and says “surgery is like that” or “this specialty attracts strong personalities,” they have chosen culture over safety. Believe them.
6. Numbers-Obsessed, Education-Optional
Some programs are fundamentally about education. Others are about service and metrics with a thin layer of lectures taped on top.
Red flags you will see if you pay attention:
- PD talks more about board pass rates than actual teaching
- Residents frequently miss conference because “the floor is too busy”
- No protected education time, or “protected” time that is constantly violated
- Residents describe learning as “on the job sink-or-swim”

| Category | Value |
|---|---|
| Program X | 2 |
| Program Y | 4 |
| Program Z | 6 |
Ask:
- “How often is conference truly protected? What happens if a nurse calls during?”
- “Who covers the floor while residents are in didactics?”
- “Do attendings actually teach on rounds, or is it mostly task-focused?”
Look for:
- A real schedule of teaching (not “we try to do noon conference most days”)
- Residents who can name attendings who are strong teachers, not just big names
- Time for reading, reflection, and procedural training, not just endless scut
If a program proudly calls itself “busy” but cannot describe how they intentionally teach you, they want your labor, not your growth.
7. Poor Board Pass Rates or Fellowship Match… with Excuses
You cannot ignore outcome data. You would not join an airline that says, “We crash more than average, but we mean well.” Yet applicants ignore clear outcome problems all the time.
Serious red flags:
- Below-average board pass rates over multiple years
- Weak fellowship match in your field of interest, year after year
- Hand-waving explanations: “We had a bad year” or “Those residents were not very motivated”
| Metric | What To Look For |
|---|---|
| Board pass rate (5 years) | Consistently high, not one good year |
| Fellowship match list | Match to solid programs, not just random |
| In-house fellowship acceptance | Fair access, not political |
| Research output | Opportunities for those who want it |
| Alumni careers | Graduates doing what you hope to do |
Ask to see:
- 5-year rolling board pass rates
- Recent fellowship match lists (not cherry-picked)
- Where graduates are working and in what roles
If the program gets defensive about this or will not share data, that is not “privacy.” That is hiding weakness.
Yes, you can succeed anywhere if you are exceptional and lucky. But why choose a place that demonstrably fails to prepare a significant percentage of residents for exams or competitive fellowships—then blames the residents?
8. Residents Do All the Scut, Others Do All the Procedures
You are not a ward clerk. You are not pure service. If your “training” consists of putting in orders and notes while others get the actual procedures and decision-making, you will graduate underprepared.
Red flags:
- Residents constantly running to answer pages, do transport, place basic orders
- Little exposure to key procedures for your specialty
- Critical decisions always made by fellows or attendings while residents are scribes
You want to hear residents say things like:
- “We do all the lumbar punctures and central lines on the floor”
- “We staff with attendings, but we are the primary decision-makers on our patients”
- “We get graduated autonomy—by PGY-3, we really run the show with backup”
Ask:
- “Who usually does central lines, LPs, intubations, etc.?”
- “What procedures do you feel comfortable doing independently by graduation?”
- “Do you feel like a clinician or a task robot here?”
If residents struggle to name procedures they own or decisions they are responsible for, this is not training. It is cheap labor.
9. Chaos, Disorganization, and “You Just Figure It Out”
Some programs are busy but coordinated. Others are pure noise.
Disorganization as a lifestyle is a massive red flag:
- Rotations not finalized or changed last-minute without explanation
- Orientation described as “you will figure it out on the first day”
- Residents always complaining about “schedule issues” or “no one told us”
- No clear policies for time off, parental leave, or sick days

| Step | Description |
|---|---|
| Step 1 | Ask about schedule |
| Step 2 | Better sign |
| Step 3 | Red flag |
| Step 4 | Frequent last minute changes |
| Step 5 | Unclear coverage policies |
| Step 6 | Residents confused about rules |
| Step 7 | Clear answers? |
Chaos is not a neutral inconvenience. It:
- Increases error risk
- Destroys trust
- Makes every day more exhausting than it needs to be
Ask:
- “How far in advance do you get your schedules?”
- “How hard is it to switch a call shift if something important comes up?”
- “What happens if someone is sick on a call day?”
If the answer is, “We beg each other in the group chat and hope someone covers,” you are looking at chronic understaffing and leadership failure.
10. Residents Are Afraid to Speak When Leadership Is Present
This is one of the biggest, most ignored red flags. Psychological safety is not just a buzzword. It is the foundation of patient safety and resident sanity.
Warning behaviors:
- Residents give glowing, generic answers with faculty present, then completely reverse tone when alone
- No one asks questions in conferences if attendings are in the room
- Jokes about “don’t say that, the PD is here”
- Chiefs look visibly anxious during Q&A sessions
You want to see:
- Residents respectfully disagree with faculty during conference without being shut down
- Real questions during town halls, not fake pre-screened ones
- PDs who leave the room at some point so residents can talk freely to applicants
If a program has to stage-manage resident interactions with you, there is a reason. Believe the tension you feel in the room, even if their slide deck says “supportive learning environment.”
Putting It Together: How To Actually Protect Yourself
Most applicants make one huge mistake: they evaluate programs but ignore patterns. One red flag you can rationalize. Four or five together? That is the reality.
Here is a simple way to avoid blundering into a toxic environment:
Make a checklist before interviews.
List these 10 areas plus anything personally important (location, family support, etc.). Bring it with you. Literally.Score each program right after each interview day.
Not “how much did I like them,” but:- Resident demeanor
- Duty hour truthfulness
- Teaching quality
- Culture / psychological safety
- Outcomes (boards, fellowship, jobs)
Weigh red flags heavier than prestige.
Matching at a big-name program that chews people up is not a win. It is a branding exercise at your expense.Trust what residents say off-script.
Hallway comments. Zoom chat side remarks. The resident who says, “Feel free to email me later with questions” from a non-program email. That is where the truth lives.Remember: you are not the exception.
You will not “rise above the culture.” You will become part of it. Choose carefully.
FAQs
1. How many red flags are “too many” before I should drop a program from my rank list?
One serious red flag (consistent duty hour violations, abusive faculty, terrible board pass rates) is enough to move a program way down. Two or more significant red flags that align—exhausted residents, vague answers about hours, high turnover—should put that program at the bottom or off your list entirely. Do not talk yourself into thinking “every program has issues” when you see a clear pattern.
2. Should I confront the program directly if I notice something concerning?
You can ask clarifying questions, but do not expect a program to confess systemic problems on interview day. Instead, ask residents privately and compare their answers with what leadership says. If there is a big mismatch, that is your answer. You are not there to fix them; you are there to assess them.
3. How do I get honest information if everything is virtual?
Use resident socials, 1:1 chats, and follow-up emails. Ask for contact with a resident who shares your interests (research, family, specific fellowship). Pay close attention to tone and consistency between different residents. You can also reach out to alumni from your medical school who matched there. People are much more candid off the official schedule.
4. Is it ever worth choosing a “toxic” big-name program for the career boost?
Usually not. A strong, mid-tier program with healthy culture, solid training, and supportive mentors will carry you much further than a malignant “name” that leaves you burned out, undertrained, or with a damaged reputation from struggling in a bad environment. Fellowship directors care about your performance, letters, and skills—those are all worse when your residency is a disaster.
5. What if all the programs I liked had at least one red flag?
You are choosing humans and systems, not fantasy camps; none will be perfect. The goal is not “no red flags ever.” The goal is:
- No major red flags that threaten your health, training, or career
- Leadership that acknowledges problems and is transparent about fixes
- Residents who, despite normal stress, would still choose the program again
If you can find that combination—even without fancy branding—you are doing better than many applicants who only looked at the name on the door.
Key points, so you do not pretend you did not see them later:
- Believe what residents show you, not what brochures tell you.
- Treat duty hours, culture, and outcomes as non-negotiable, not “soft” factors.
- Patterns of red flags are not bad luck; they are the truth of the program. Choose accordingly.






















