The wrong letter of recommendation can quietly sabotage your residency application—and yes, that includes a shiny new one from someone who barely knows you.
You’re asking the right question: should you replace an older, solid LOR with a new but unproven one? Short answer: usually no. But there are cases where you should. Let’s walk through exactly how to decide.
The Core Rule: Strong Old > Mediocre New
If you remember nothing else, remember this:
A strong older letter almost always beats a weak or generic newer letter.
Programs don’t reject you because a letter is from 18–24 months ago. They reject you because a letter:
- Sounds generic
- Feels lukewarm
- Doesn’t say anything concrete about how you work
- Conflicts with the rest of your story
I’ve watched residents on selection committees skim right past the date and zero in on:
- Does this attending clearly know this applicant?
- Are there specific examples?
- Does this letter place the applicant above peers?
If your old letter hits those, it’s an asset—even if it’s “last year’s” attending. If your new potential letter writer:
- Didn’t see you much
- Doesn’t supervise residents or students often
- Seems polite but vague when agreeing
…then you’re about to trade a known strength for a question mark. Bad move.
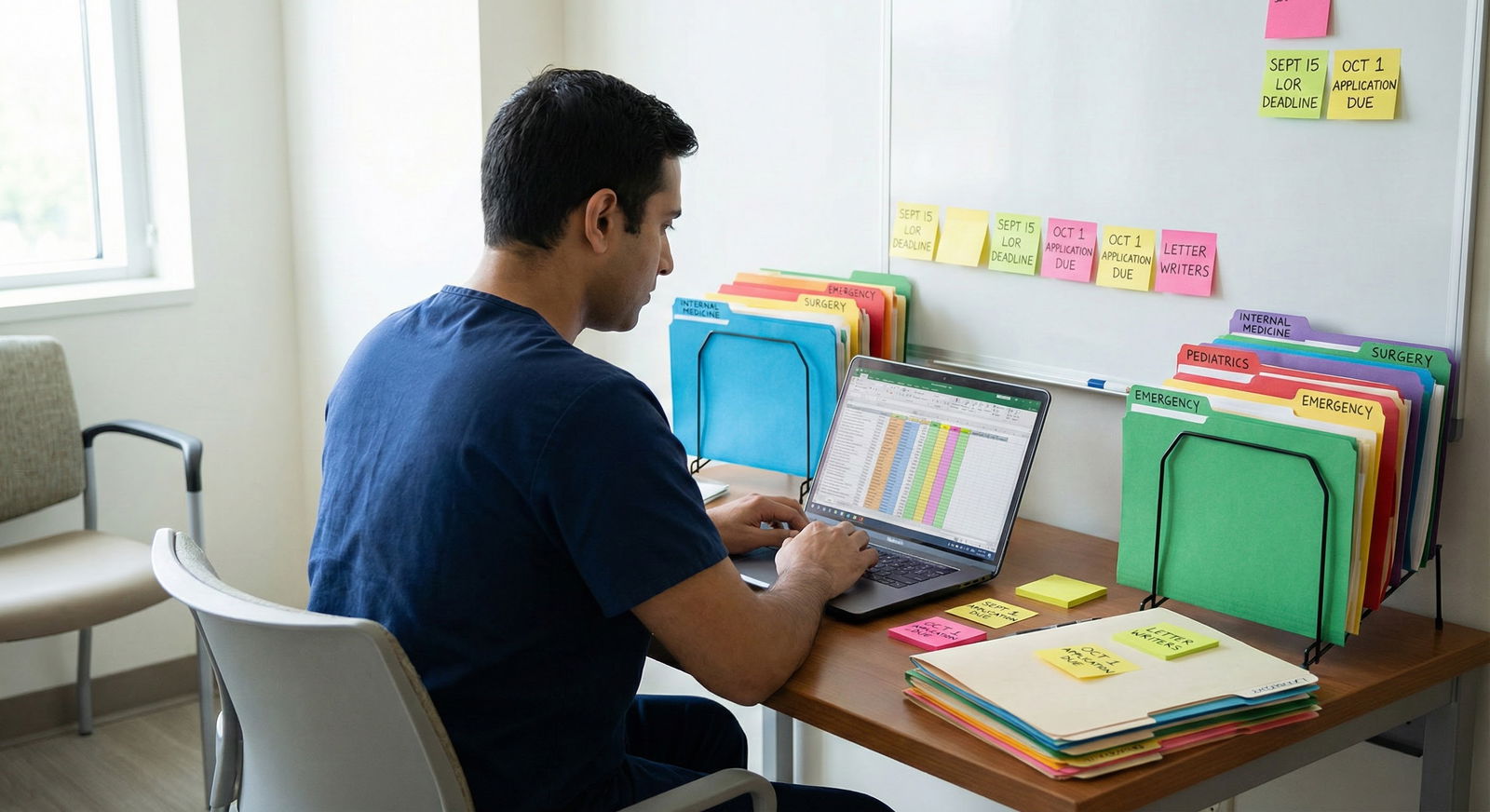
Step 1: Clarify Your Situation
You can’t decide about replacing a letter in the abstract. You need to map your actual letter portfolio.
Write down:
Total number of letters you can submit
- ERAS allows up to 4 per program.
What you already have (or expect):
- How many total letters?
- How many specialties (e.g., IM, Surgery, EM)?
- Who are the writers? (titles, relevance)
- How old is each letter?
What the target specialty expects. For example:
| Specialty | Ideal # of Specialty Letters | Chair/Department Letter Expected? |
|---|---|---|
| Internal Medicine | 2+ IM attendings | Sometimes, not always |
| General Surgery | 2+ surgery attendings | Often preferred |
| Emergency Medicine | 2–3 SLOEs | Yes, SLOEs are critical |
| Psychiatry | 1–2 psych attendings | Nice but not mandatory |
| Family Medicine | 1–2 FM attendings | Helpful but flexible |
If your old letter is one of only 1–2 strong specialty-specific letters you have, it’s almost never the one you drop.
Step 2: Judge Each Letter on the Only Two Things That Matter
Forget old vs new for a second. Every letter should be judged on two axes:
- Strength (how good is it likely to be?)
- Relevance (how well does it match the specialty and your application story?)
1. How to Estimate Letter Strength (Before You See It)
You’ll never see the actual text (and you shouldn’t try), but you can predict quality pretty well based on:
- How well the writer knows you.
- Did you work with them for 4–8 weeks? Or 3 random night shifts?
- How directly they observed your clinical work.
- Did they see you present, write notes, manage patients, take feedback?
- Their enthusiasm when you asked.
- “I’d be happy to write you a strong letter” = green light.
- “Sure, I can write something” = yellow/red.
- Their experience writing residency letters.
If your old letter came from a core rotation attending who loved you and said they’d write a strong letter, that’s gold. A new letter from a peripheral elective where the attending barely remembers you is not an upgrade.
2. How to Judge Relevance
Relevance comes from:
- Specialty match:
- Applying IM? IM letters > random research PI in neurosurgery (unless very involved).
- Role of writer:
- A medicine sub-I attending > a random consultant who saw you once.
- How it fits your story:
- If you’re pitching yourself as “clinically strong with great teamwork,” you want letters that explicitly back that up.
Step 3: When You Should Not Replace the Old LOR
Let’s be clear where people usually overthink this and shoot themselves in the foot.
Don’t replace the old letter if:
It’s clearly strong and specific.
- From an attending who supervised you closely
- From a core rotation or sub-I
- Known good letter writer (clerkship director, PD, etc.)
You don’t actually need to swap it out for space.
- ERAS lets you assign different combinations to different programs.
- If you have 5–6 decent letters, you don’t have to “globally replace” anything—you just assign selectively.
The only reason you’re nervous is the date.
- 1–2 years old? Programs see this constantly, especially from reapplicants or research year students.
- 3+ years old? Still can be fine if it’s your best clinical performance and you’ve been in a research/leave gap.
The new writer barely knows you.
- Any attending who’d struggle to recall a single patient you managed → they’ll write a vague letter. Vague kills.
Step 4: When You Should Strongly Consider a New Letter
There are situations where a new letter is absolutely worth getting, even if it means an older one gets benched for some programs.
Consider prioritizing a new letter if:
- You Have a Weak Link Letter
If you already suspect one of your letters is mediocre—replace that, not the strong older one. Clues a letter might be weak:
- Writer was hesitant or lukewarm when asked
- They barely saw you clinically
- They’re not in your specialty and don’t know you well in any other serious context
- They frequently write very generic letters (your seniors may warn you)
- Your Application Direction Has Changed
Examples:
- You did a prelim year in surgery, now applying to IM.
- You were research-heavy, now emphasizing clinical rebirth in your gap year.
In that case, a fresh letter showing your current clinical performance in the new specialty can be critical. But again, you add it to the mix; you don’t necessarily delete the older strong one unless you’re at the 4-letter cap.
- You Need a Required-Type Letter
For example:
- EM: you need SLOEs. No SLOE = application dead in the water.
- Some surgery programs: really want at least 1–2 surgery attendings.
In those cases, a relevant-but-new SLOE or surgery LOR beats an older but totally unrelated one. That’s not a “replace a strong letter” problem; it’s a “meet the minimum bar” problem.
Step 5: Handle Reapplicants and Gap Years Properly
This is where the “old vs new” anxiety really spikes.
If You’re a Reapplicant
Programs will recognize reused letters. That’s not automatically bad. What matters:
- Did you add at least one new letter showing recent growth or performance?
- Does your letter set as a whole feel more robust and targeted than last year?
For reapplicants, an ideal mix often looks like:
- 1–2 strong older clinical letters (still relevant)
- 1–2 new letters from your current year (research PI, new clinical work, new sub-I, etc.)
You don’t need to throw out a great letter just because the calendar flipped. But you do need something new.
If You Took a Research Year / Nonclinical Year
Programs want to know you didn’t disappear.
In that case, I’d aim for:
- Keep the strongest old clinical letters (even 2–3 years old)
- Add:
- 1 new letter from research PI or job supervisor
- OR 1 new letter from a short clinical refresh (locums, observership, sub-I, etc.)
Again, supplement. Don’t mindlessly replace.
Step 6: Decide Using a Simple Ranking System
If you’re stuck, rank all your potential letters. Literally score them.
Make a quick grid like this:
| Letter | Writer Role | Specialty Match | Strength (1–5) | Relevance (1–5) | Total |
|---|---|---|---|---|---|
| Old IM Attending | Core IM Faculty | IM | 5 | 5 | 10 |
| New Elective Attending | Outpatient IM | IM | 3 | 4 | 7 |
| Research PI | Cardiology Lab | Partial | 4 | 3 | 7 |
| Old Surgery Attending | Gen Surg | None (for IM) | 4 | 2 | 6 |
Your 4 highest totals are the default picks for that specialty. Older vs newer doesn’t matter; quality and fit do.
Step 7: Specific Scenarios and Clear Answers
Let’s cut through a few common real-life situations.
Scenario 1: MS4, Applying IM, Old Letter From 3rd-Year Core IM
- 8-week IM clerkship, attending loves you, said “strong letter”
- Letter is from 16 months ago
- New potential letter: 2-week IM elective where you saw them 3 days
Keep the old letter. Use the new one only if that attending also clearly knows you and you don’t already have 2–3 solid IM letters.
Scenario 2: Reapplying to EM, Have 1 Strong Old SLOE, 1 Meh SLOE
Your priorities:
- Get at least one new SLOE this year if at all possible.
- Keep the strong old SLOE.
- Replace the weaker SLOE with the new one.
Here, you absolutely do not drop the strong older SLOE just because a new letter exists.
Scenario 3: Switched Specialties Last Minute
Let’s say you did all your sub-Is in surgery, then pivoted to IM.
- Old letters: 2 surgery, 1 lukewarm IM
- New possibility: 4-week IM sub-I now
You should 100% get a new IM letter. Then:
- Keep the best of your surgery letters if it speaks broadly to work ethic, resilience, or clinical reasoning.
- Drop the lukewarm IM letter if the new one is strong.
Visual: How Programs Value Letter Types

| Category | Value |
|---|---|
| Strong Specialty Clinical LOR | 95 |
| Strong Non-Specialty Clinical LOR | 80 |
| Strong Research/PI LOR | 70 |
| Generic LOR from Big Name | 40 |
| Old but Strong Specialty LOR | 85 |
Those numbers aren’t from a single study—they reflect how program directors consistently talk about letters. Notice where “old but strong” lands: still extremely valuable.
How to Ask for the New Letter Without Burning Bridges
If you’re leaning toward adding a new letter, here’s how to do it intelligently.
Ask directly for a “strong” letter.
Email or in person: “Would you feel comfortable writing me a strong letter of recommendation for internal medicine?”- If they say yes confidently → good.
- If they hedge → don’t use them.
Give them ammo.
- CV
- Personal statement draft
- ERAS experiences list
- Brief bullet list of patients or situations where you worked closely with them
Don’t promise them you’ll definitely use it for every program.
You’re allowed to manage your application strategically. They don’t see which programs actually receive their letter.
The One Time You Truly Should Replace a Strong Old Letter
There’s one ugly corner case:
- The old letter may accidentally undermine your current narrative.
Examples:
- Old letter emphasizes your enthusiasm for surgery, but you’re now applying psychiatry with zero explanation.
- Old letter describes performance with words like “adequate,” “solid,” “reliable” while your newer performance is dramatically stronger and you have letters saying “top 5%.”
If the old letter makes your growth story confusing or contradicts your current direction, that’s when you can justify moving it off the main stage—even if it was “strong” in isolation.
A Quick Flow to Make Your Final Call
Here’s a simple way to think it through:

| Step | Description |
|---|---|
| Step 1 | Have Old LOR |
| Step 2 | Okay to replace with better option |
| Step 3 | KEEP the old LOR |
| Step 4 | Still consider keeping for some programs |
| Step 5 | Replace for most programs |
| Step 6 | Is Old LOR from core/specialty rotation and likely strong? |
| Step 7 | Do you have 4 clearly stronger and more relevant letters? |
| Step 8 | Does old LOR conflict with your current specialty/story? |
Where Dates Actually Matter
Let’s be precise: dates matter in these situations:
- You’ve been out of clinical work for several years, and all your letters are old → get something new.
- You’re a reapplicant and submitted literally identical letters, no updates → looks lazy or stagnant.
- You’ve had poor performance since that old letter that isn’t addressed anywhere → committees might wonder.
But “this letter is from last year’s rotation” on a current MS4? That’s just normal.
What You Should Do Today
Don’t guess. Inventory.
Today, open a document and:
- List every current or potential letter writer.
- For each, write:
- Specialty, role, how long they knew you, how strong you think the letter is, and how relevant it is.
- Rank them for your target specialty.
- Decide which 4 letters you’d send if ERAS locked today.
Then ask yourself one focused question:
“Is this new potential letter likely to be stronger and more relevant than one of my current top 4?”
If the honest answer is no or “I don’t know,” don’t replace a proven older LOR just because it’s new.





















