The most honest evaluation of a residency program will never be on the website. It’s the resident who pulls you aside and says, “Hey…just so you know, this place is rough.”
You’re not crazy for feeling your stomach drop when that happens. You’re also not crazy for thinking, “So what do I do with this?”
Here’s the answer: you treat those quiet warnings like data. Valuable, emotionally loaded, sometimes biased data. Then you handle the situation strategically instead of either panicking or ignoring it.
This is how.
Step 1: Freeze Your Face, Not Your Brain
You’re on a tour. Or sitting at resident lunch. Or walking between interviews. A senior leans in and says some version of:
- “People here aren’t happy.”
- “If you have other options, look at them seriously.”
- “We work like crazy and leadership doesn’t care.”
- “Off the record… I wouldn’t rank this #1 if I were you.”
Your instinct might be to react. To ask, “Wait, really? Why?” in a way that makes everyone at the table turn and stare.
Do not.
You need two things in that moment:
- A neutral, non-committal exterior.
- A very active internal recorder.
What you actually say out loud:
- “Thanks for being honest, I appreciate it.”
- “Got it, that’s really helpful context.”
- “I hear you—can you tell me more later if there’s time?”
Tone: calm, appreciative, not shocked. You want them to keep talking without feeling like they’re about to get burned if you repeat this.
What you do internally:
- Mentally tag the comment: “Signal. Investigate.”
- Clock who said it: PGY level, specialty within the program (for IM subs, surgery services, etc.), vibe (burned out? bitter? thoughtful?).
- Note the setting: alone in a stairwell? Group lunch? Social event?
You are not deciding anything yet. You’re collecting.
Step 2: Pull the Signal Apart – What Exactly Are They Warning You About?
Residents rarely say, “Our ACGME case logs are inadequate” or “There’s a culture of retaliatory professionalism reports.”
They say things like:
- “We get crushed here.”
- “Leadership doesn’t listen.”
- “People burn out fast.”
- “Morale is horrible.”
Your job is to translate vague doom into something specific.
Here’s the quick mental framework I use. Ask yourself: are they talking about…
| Category | What It Usually Sounds Like |
|---|---|
| Workload / Hours | "We get crushed", "80 is a joke" |
| Culture / Support | "No one has your back", "Toxic" |
| Education / Training | "You just service", "No teaching" |
| Safety / Compliance | "Sketchy", "They ignore rules" |
| Career Outcomes | "People can’t match fellowships" |
You do not need to ask them this taxonomy explicitly. But in your head, try to fit their comments into one or more of these buckets. It changes how worried you should be.
A brutal but supportive, high-volume trauma program? That’s one thing.
A malicious, retaliatory, gaslighting culture? Entirely different.
Listen for concrete examples:
- “We regularly stay 4–5 hours past shift and still log 80 hours.”
- “We had three residents leave last year.”
- “Program director retaliated after someone reported duty hour violations.”
- “We’re solo covering 30+ ICU patients at night as PGY1s.”
The more specific the resident gets, the more you should pay attention.
Step 3: Ask Smarter Follow-Up Questions (Without Outing Them)
If a resident cracks the door open, you can gently push—if you do it right.
Key rule: protect them. You never ask anything that makes them identifiable in a complaint.
Good follow-ups in the moment:
- “When you say it’s rough, do you mean hours, culture, or training?”
- “Has it been getting better or worse over the last year or two?”
- “Do residents stay here for fellowship/attending jobs or try to get out?”
- “If you were applying again now, what would you do differently?”
If you’re on a social event / pre-interview dinner and it feels safe:
- “Are there things you wish you had known as an applicant that you only learned after starting?”
- “Do you feel like leadership listens when residents raise issues?”
- “How comfortable do you feel calling in sick or asking for help?”
Keep your voice neutral. You’re not fishing for drama; you’re doing due diligence.
If they seem nervous, back off. “No worries—thank you for being honest, that already helps a lot.” Let them control how much they share.
Step 4: Cross-Check With the Rest of the Day (Silently)
Never base your rank list on one burned-out PGY-2 you met post-night float. But also don’t ignore them.
You cross-validate.
Here’s what you quietly compare their warning against:
A. What other residents say
Patterns matter more than one voice.
- Do multiple people independently mention “morale,” “communication,” “we just lost X faculty”?
- Do junior and senior residents tell totally different stories?
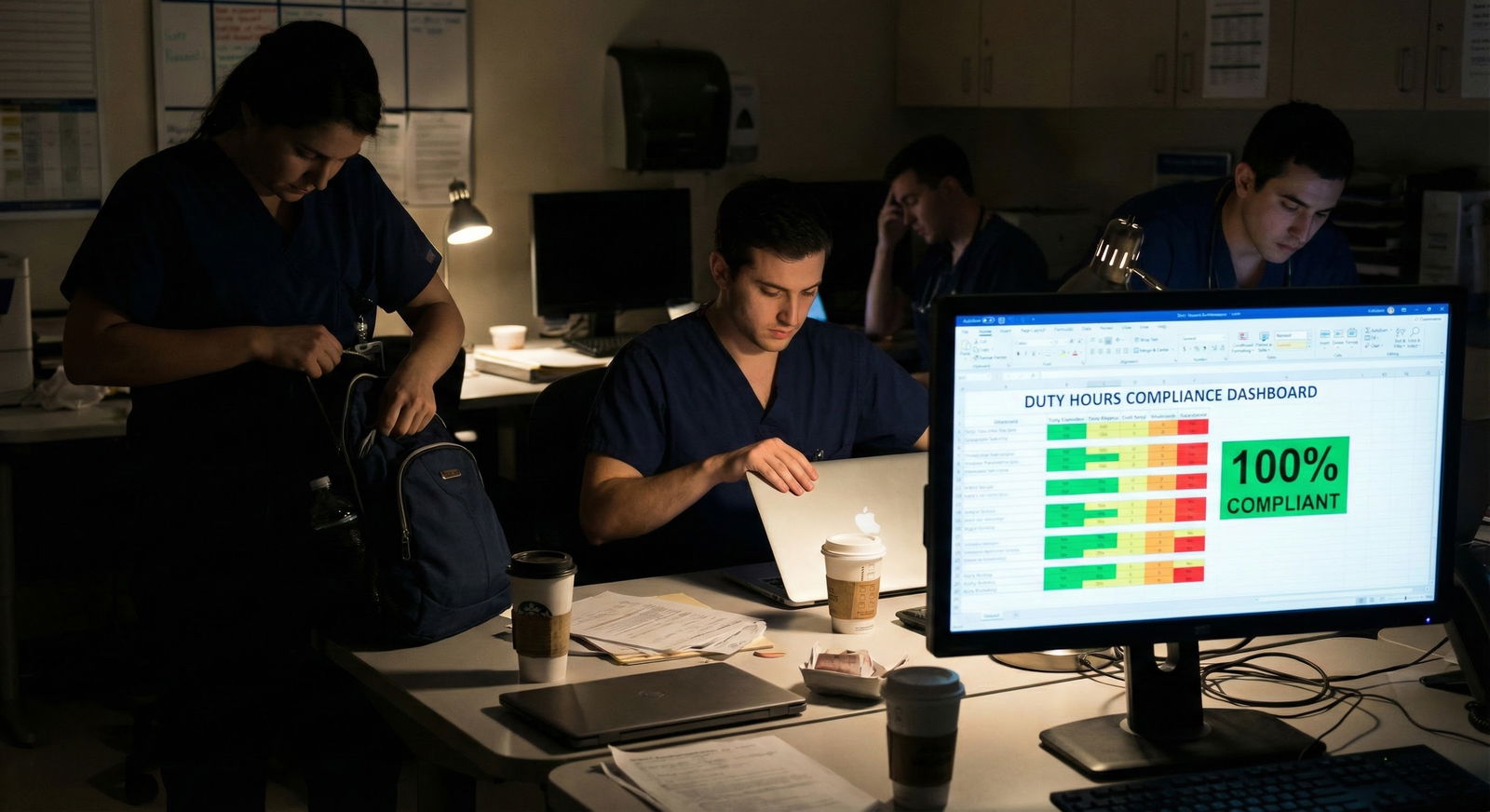
- Do residents contradict each other in front of you? (“We never violate duty hours!” vs “Yeah, we just don’t log over 80.”)
If you hear the same concern from 3+ residents at different times that day, that’s not random. That’s smoke. Sometimes fire.
B. The vibe in resident-only spaces
Pay attention to what happens when attendings leave the room.
- Laughter suddenly becomes darker, more cynical?
- Residents make jokes like “Yeah…this program likes to pretend that doesn’t happen” and the table gets quiet?
- Someone says, “Hey, don’t scare them off,” and people glance at each other?
Those micro-moments are incredibly diagnostic.

C. Faculty behavior and language
Red flag combo: residents quietly warning you + attendings acting defensive.
Watch for:
- Overly rehearsed lines about “we’re a family” with no specifics.
- Faculty brushing off resident concerns: “They complain, but every program is like this.”
- Any hint of “we don’t tolerate weakness,” “we need residents who won’t complain.”
That last one in particular? Believe them. That’s exactly how they’ll treat you.
D. Objective data you can see
You’re not going to get the entire truth in a day, but you can still scan for:
- Board pass rates (if they’re weirdly low or not reported at all).
- Recent or current ACGME warning/citations (Google “[program name] ACGME letter” later).
- How many residents are on the roster vs how many faces you actually see. Quiet missing residents = sometimes people left.
Step 5: After You Leave – Investigate Without Burning Bridges
Once the interview day ends, you have way more freedom to dig. This is where most applicants either go too hard (panicked cold-DM blasts to every alum) or too soft (pretend they never heard the warning).
You’re going to be deliberate.
Reach out to non-interview-day residents
If the program gave you a list of email contacts “for questions,” use it. You write something like:
Hi Dr. X,
Thank you again for speaking with us during the interview day for [Program]. I had a great time meeting everyone.
I’m in the process of building my rank list and wanted to ask a candid question or two about resident life and culture. Would you be open to a quick 10–15 minute call sometime this week or next?
Thanks again,
[Your Name]
On the call, you ask broad and then gradually more pointed questions:
- “How has the program changed since you started?”
- “What’s the biggest strength and the biggest weakness?”
- “How do residents handle it when they’re overwhelmed or struggling?”
- “Do people generally stay for the full program? Have there been any unexpected departures?”
If the warning you heard was serious—like retaliation, bullying, chronic unsafe staffing—you can carefully probe:
- “I heard hints that morale has been a challenge recently. Is that something you’ve noticed too, or does it depend on the rotation/team?”
Do not quote the specific resident or the exact moment. You protect them.
Use alumni and mentors
Ask people at your home institution:
- “Have you heard anything about [Hospital X]’s IM program recently?”
- “Do we have any alumni there? Are they happy?”
- “Would you rank this program high for someone like me?”
Faculty hear things you don’t. They trade impressions all the time. Use that network.
Step 6: Weighing the Warning Against Your Situation
Now we’re at the hard part: what do you actually do with all of this?
You’re balancing:
- Your competitiveness and options
- The severity of the issues
- Your personal priorities and risk tolerance
Let’s be blunt.

| Category | Value |
|---|---|
| Brutal Hours Only | 40 |
| Weak Teaching | 50 |
| Bad Morale | 60 |
| Toxic Leadership | 80 |
| Unsafe / Retaliatory | 95 |
Interpretation:
- 30–50 range: Serious but sometimes manageable with eyes open.
- 60–80: High-risk; you need strong reasons to still rank them high.
- 90+: Program should drop sharply on your list unless you have almost no alternatives.
If you’re a strong applicant with options
If you have multiple solid interviews, no red flags, and then one where residents quietly warn you off?
You don’t martyr yourself “for the name” or the city.
Here’s my stance: you almost never need to put a clearly toxic or unsafe program in your top 3 if you have other viable places. Prestige, fellowship pipelines, city desirability—none of that compensates for three miserable, dangerous years with no support.
You can still keep them on the list (you should almost always rank every place you’d be willing to attend), but moved down. Sometimes way down.
If your application is average and options are limited
This is trickier. You may feel like, “If I don’t rank them, I might not match.”
Reality: an imperfect, hard program still beats not matching at all—if the issues are not outright abusive or unsafe.
Where I draw the line for “only if no alternative”:
- Multiple residents describe retaliation for raising concerns.
- Systematic duty hour violations with pressure to lie.
- Chronic understaffing that puts patients (and you) at real risk.
- Pattern of residents leaving, being fired, or not graduating on time.
If we’re at that level, I’d rather see you:
- Expand to SOAP if needed.
- Consider a prelim year then reapply or pivot.
- Look at less competitive specialties or less shiny locations.
You can recover from a non-match or detour. It’s much harder to recover from being destroyed in a malicious program.
Step 7: How to Talk About It (To Others, Not To Them)
You might be tempted to “help” future applicants by blasting the program anonymously online or telling everyone you know it’s awful.
Calm down.
You can share honest experiences without getting dragged into drama or defamation.
With classmates and trusted juniors:
- “Some residents expressed real concerns about [culture / hours / support]. I’d encourage you to talk to people there directly before ranking.”
- “I’d be cautious. Ask pointed questions about [morale, leadership responsiveness, turnover].”
You don’t need to recount exact names or quotes.
With faculty / advisors:
Be a bit more specific; they have context and power.
- “Two different residents warned me about morale and leadership being unresponsive. One mentioned residents leaving the program mid-year.”
They can decide how to handle that information.
With the program itself:
Do not email the PD afterward to say, “Your residents are warning people about your program.” That helps no one and puts residents at risk. The only exceptions:
- You witnessed or experienced blatant discrimination or harassment that needs institutional reporting.
- There’s a patient safety issue so severe you’d file a report at your own institution too.
Even then, consider reporting through appropriate channels, not a casual PD email.
Step 8: Specific Red and Yellow Phrases – How to Interpret Them
Residents use code. Let me translate some of the more common ones I’ve heard.
“We’re very busy, but you learn a lot.”
Translation: High workload. Could be fine if culture is good. Yellow flag, not automatic no.“We’re working through some ‘growing pains’.”
Often means: Program expanded too fast / leadership turnover / chaos. Ask: “Have those changes settled or still ongoing?”“We take care of very sick, underserved patients.”
Could be amazing. Could also mean: high acuity + low resources + poor backup. Need more detail.“You need a thick skin to work here.”
Culture often includes yelling, shaming, or belittling. Not always, but often. Big caution sign.“If you’re resilient, you’ll be fine here.”
Translation: We will not protect you. We expect you to tolerate whatever happens.“Off the record, I’d go somewhere else if you can.”
That’s about as loud as a resident can scream without using a megaphone. Take it seriously.
Step 9: Handling It Emotionally (Because Yes, This Messes With Your Head)
Let me guess: you interviewed at a “dream” program. Top name. Great city. Then three residents quietly tell you it’s hell.
You will go through a tiny grief cycle.
- Denial: “Maybe they’re just a negative clique.”
- Bargaining: “I can handle anything for three years; the prestige is worth it.”
- Anger: “Why does this place have such a good reputation?”
- Acceptance: “Okay. It’s not what I thought. I need to adjust.”
Give yourself a day or two to be disappointed. Vent to a friend or mentor you trust. Then get back to making a rational list.
Residency is not four weeks. It’s three to seven years. You cannot grind through a consistently toxic environment without it changing who you are.
You want hard. You don’t want harmful.
Step 10: If You Decide to Still Rank Them High
Sometimes, after all this, you’ll still say: “I’m going to rank them near the top.”
Fine. Adults make trade-offs.
If you do, then you go in eyes wide open and with a survival plan:
- Identify at least 1–2 senior residents who seemed grounded and candid. Those are your early allies.
- Before starting, clarify wellness resources, ombudsman, and how to escalate real safety issues.
- Set boundaries around off-the-books work: do not falsify duty hours or accept unsafe assignments without at least documenting your concerns to someone.
- Have an outside mentor (home institution, prior attending) you can call if things get bad.
Your goal: extract the training, minimize the damage.
Open your notes app right now and write down, for the last “iffy” program you saw: (1) what exactly residents warned you about, and (2) how severe you honestly think it is. When you sit down to build your rank list, those two sentences will keep you from rewriting history to fit what you wish were true.






















