The way most people talk about night float is wrong.
Program directors sell it as a humane, modern solution to burnout. Residents in toxic programs swear it’s the root of all evil. Both camps are exaggerating. The data – and the day-to-day lived reality – are messier and far less romantic than either story.
Night float is neither automatically malignant nor automatically protective. It is a powerful tool that can do real harm or real good depending on how it’s built, staffed, and supervised. And a lot of programs get the details wrong.
Let’s strip away the mythology and deal with what actually happens to residents’ sleep, learning, safety, and burnout when you move from traditional 24–28 hour call to night float.
What Night Float Actually Is (Not the Sales Brochure Version)
At its core, a night float system means you have a dedicated team of residents who cover nights for a defined block of time, usually anywhere from 3–14 nights in a row, rather than having every resident take intermittent 24–28 hour calls.
The usual sales pitch you’ll hear on interview day:
- “We eliminated 28-hour calls to protect wellness.”
- “You’ll always have post-call days; night float centralizes the pain.”
- “Continuity is preserved on days; your clinic and day team aren’t constantly disrupted by call.”
Some of that is true. Some is half-true. A lot is just convenient branding to satisfy ACGME and make the PowerPoint look progressive.
The reality on the ground varies wildly:
- Some programs do 2 weeks on / 2 weeks off of night float, with 6-night weeks and one day off.
- Others cram 6–7 nights in a row, repeat, and pretend that one “golden weekend” cancels everything out.
- Some have full in-house attending coverage; others leave you as the de facto nocturnist with “phone attending” supervision.
If you talk about night float like it’s one single thing, you’ve already lost the plot. It’s a structure that can be optimized or abused.
What the Evidence Actually Shows: Sleep, Errors, and Safety
Let’s start with the part that’s not up for debate: extended-duration shifts wreck human performance.
Studies going back to the 2004 NEJM paper by Landrigan et al. showed interns working traditional Q3 24–30 hour shifts made more serious medical errors than those in an intervention schedule with shorter shifts and more night float. The D.C. motor vehicle crash risk paper from Barger et al. showed post-call residents were more likely to fall asleep at the wheel and crash.
So yes, the old-school “28 hours or you do not learn medicine” crowd is just wrong. The data is brutal: longer consecutive hours awake = worse cognitive performance and more errors. That’s not controversial in sleep medicine.
But here’s the twist nobody selling you night float on interview day wants to emphasize:
Night float does not magically fix fatigue. It just redistributes it.
Residents on night float often:
- Sleep poorly during the day (thanks to noise, light, family obligations, pager expectations)
- Build up cumulative sleep debt over consecutive nights
- Have circadian misalignment that tanks mood and cognitive function

| Category | Value |
|---|---|
| Day Shift | 6.5 |
| Traditional 28-hour Call | 4.5 |
| Night Float Block | 5.5 |
Typical pattern I’ve seen over and over: day shifts average 6–7 hours of sleep, brutal 28-hour calls get 3–5 hours, and night float blocks net something like 5–6 hours but with terrible quality and awkward timing. Better than post-call driving half-dead. Not exactly restorative.
From a pure patient safety standpoint, night float can reduce disastrous extended-wake-time errors. But if the block is long and the schedule is inhumane, you just trade short-term hazard for chronic cognitive dulling and emotional exhaustion.
So is it safer? Usually yes, compared to Q3 28-hour call. Is it the wellness utopia some PDs pretend? Not even close.
The Real Burnout Question: Chronic vs Acute Suffering
Burnout is not just about how tired you are after a single shift. It’s about:
- Predictability
- Control
- Sense of meaning
- Quality of supervision and team culture
- Cumulative moral injury and workload
Night float interacts with all of these, but not always how you expect.
Here’s the myth: “Night float protects against burnout because residents get post-call days and more structured rest.”
Reality: Night float helps some people and destroys others, depending entirely on implementation.
Patterns that tend to reduce burnout:
- Shorter night float blocks (5–7 nights) with protected recovery days at the end
- Reasonable cap on admissions and cross-cover volume
- Real in-house attending or senior supervision
- Clear expectations that you are not chart-catching for overwhelmed day teams
- Limited night float rotations per year
Patterns that reliably increase burnout:
- 2–4 week blocks where you’re a ghost to your own program and social life
- Being the dumping ground for everything nobody else finished (“night float will clean it up”)
- No real supervision – just you, the cross-cover list, and a phone number you’re scared to use
- Using night float to silently increase total resident coverage without adding FTEs
So does night float protect from burnout? It can. But programs also use it as a fig leaf to hide structural understaffing and unrealistic expectations. That’s when it feels malignant.
Continuity of Care and Learning: The “Educational Black Hole” Myth
One of the favorite arguments of the anti-night-float old guard is that it “destroys continuity” and “kills education.”
Part of that is nostalgia for the era when you admitted a patient, slept three hours in a call room, rounded, and then followed that patient for days. That did create strong continuity. It also created dangerous fatigue and the illusion that suffering = learning.
The real trade-off with night float is different:
- You lose follow-through on the patients you admit at night.
- You sometimes become a pure fire-fighter: see the stemis, the GIBs, the septic shocks, and then hand them off.
But you also gain:
- More stable daytime teams who aren’t constantly post-call or absent
- More consistent attendance at conferences and clinics
- Focused exposure to acute pathology and rapid decision-making
I’ve heard residents call night float an “educational black hole.” That’s often because their program treats it that way:
- No bedside teaching at night
- No structured sign-out cases reviewed by attendings in the morning
- No feedback on overnight decisions unless something went wrong enough to start an inquisition
If you’re seeing that pattern, that is a program red flag, not a night float inevitability.
Well-run systems have:
- Attendings who come in early and debrief admissions with the night team
- Sim or case-review sessions targeted at the kind of problems that appear at 2 a.m.
- Evaluations that actually reflect your night performance, not just “unknown, they were on nights”
The continuity argument is not fake, but it’s overblown. You trade “I admitted and followed them” continuity for “our team is consistently functioning during the day” continuity. Some specialties feel that trade more (peds heme-onc; geriatrics with long LOS) and some less (ED, ICU).
The Red Flags: When Night Float Is Malignant by Design
Let me be very clear: night float itself is not automatically a red flag.
But how a program runs its night system tells you a lot about whether they respect residents as humans or see them as cheap labor.
Here are structural features that should make you pause:
- Endless night float blocks or too many per year
If a categorical internal medicine resident is doing 5+ months of night float over 3 years, that’s excessive. When you hear about 4-week blocks repeated multiple times per year, ask how people feel after their third block. You’ll get your answer.
- No cap and no backup
If cross-cover lists are absurd (“You’ll cover 80–100 patients overnight”) and there’s no built-in backup or flex system, that’s a workload problem mislabeled as “night float.”
- Phone-attending culture with fear of escalation
If residents consistently say things like “We don’t call attendings unless the patient is literally coding,” that’s not independence; that’s abandonment.
- Night float used to patch chronic daytime dysfunction
Red flag if residents tell you: “Days always dump unfinished notes and sign-outs on nights because they’re drowning.” That means the program is under-resourced and using nights as a pressure release valve.
- Zero protection of daytime sleep
If after a night you’re expected to come back early for mandatory conferences, educational half days, or random admin tasks, they are robbing you of the only recovery window you have. That’s not a small issue. That’s how chronic sleep debt and burnout are baked in.
- You never see attendings at night
Some subspecialties and smaller hospitals won’t have 24/7 in-house coverage; that’s reality. But if nobody ever comes in and every scary call ends with “just keep an eye on them,” that’s a safety and culture problem.
The Green Flags: When Night Float Really Is Protective
To be fair, some places get this right. And those places often have residents who defend night float fiercely because, in context, it’s genuinely better than the alternatives.
Green flag features:
- Night blocks limited to 1–2 weeks at a time with predictable off-nights
- Strict adherence to a reasonable census/cross-cover cap
- Built-in, no-punishment escalation to in-house or easily available attendings
- Program leadership that openly adjusts schedules when nights become unsustainable
- Thoughtful staggering of shifts to minimize circadian whiplash (not dumping you from nights to a 6 a.m. conference the next day)
| Feature | Well-Run Night Float | Malignant Night Float |
|---|---|---|
| Block length | 5–7 nights | 14+ nights |
| Supervision | In-house or easy | Distant phone only |
| Cross-cover load | Capped, monitored | “As many as needed” |
| Recovery time | Protected days off | Nights to early days |
| Use in system | Safety + education | Cheap coverage |
If you want to know which camp a program is in, do not listen to the PD slide deck. Ask the second- and third-years off to the side: “How do you feel after a night block?” Their face will answer faster than their words.
What You Should Actually Ask on Interview Day
You do not need to become a sleep-medicine researcher to figure this out. You just need to ask the questions most applicants are too polite or too naïve to ask.
A few concrete ones:
- “How many total weeks of night float will I do over the entire residency?”
- “What’s the typical cross-cover census for an intern on nights?”
- “Are attendings physically present in-house at night for X service, or only by phone?”
- “What happens if nights become overwhelming – is there a backup system?”
- “Do you ever pull residents from clinic or electives to cover consistent night coverage gaps?”
Pay very close attention to whether residents’ answers match leadership’s answers. If PDs talk about how night float “really protects wellness” and residents give tight smiles and say, “It’s… manageable,” that gap is your red flag.
The Future: Night Float 2.0 or Something Else?
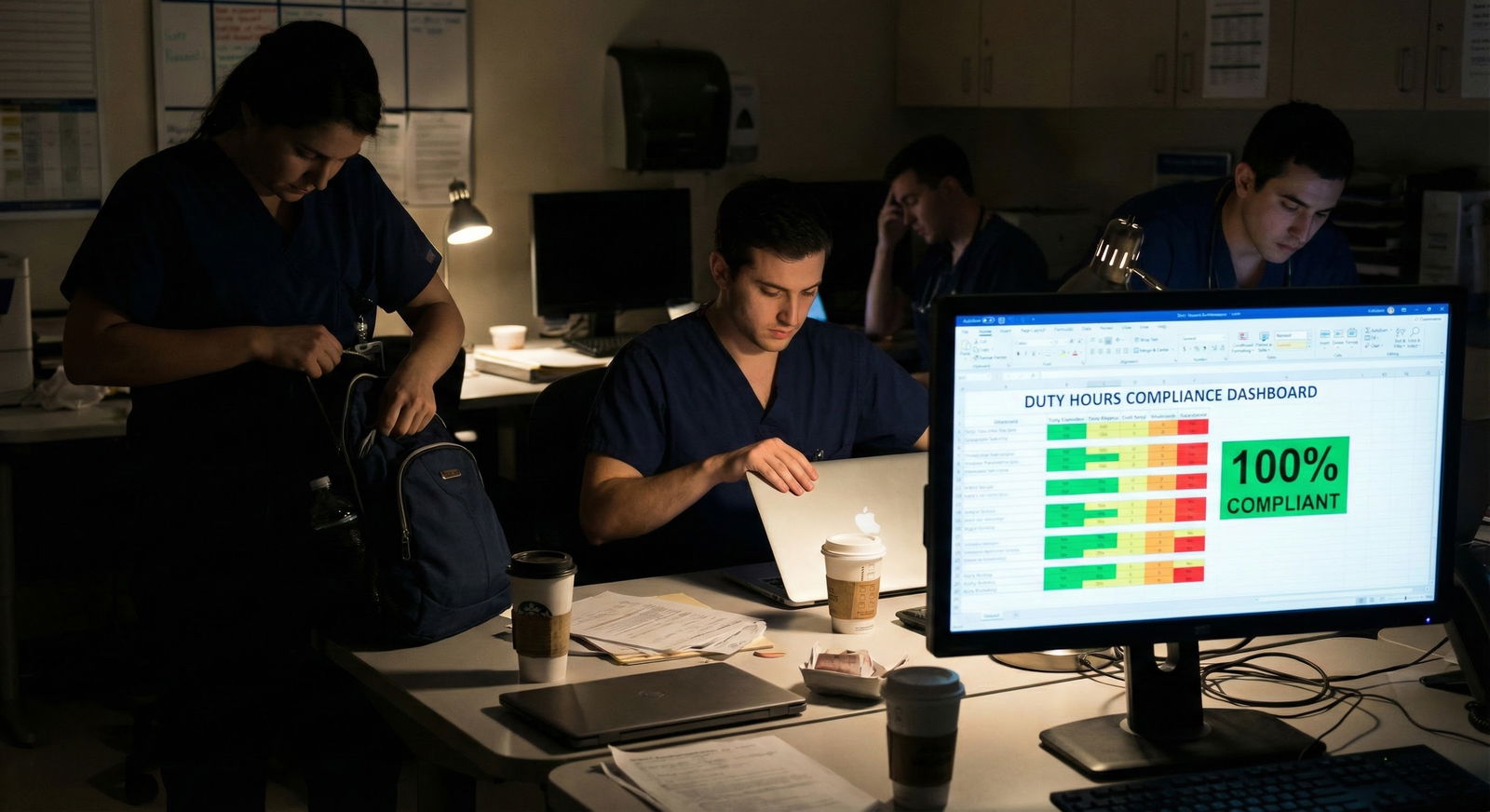
We’re in a weird transition era. ACGME duty hour limits knocked out the worst of the 36-hour-call-every-third-night insanity, but programs responded with some lazy fixes: bolt-on night float without rethinking staffing, workload, or educational goals.
Where this is heading if people are honest:
- More true nocturnist attendings in academic centers, with residents as learners, not primary unsupervised night coverage.
- Smarter scheduling that uses data on actual admission patterns and cross-cover needs instead of “we’ve always done it this way.”
- Tech that actually helps (better sign-out tools, real-time dashboards), not more clicks and alerts dumped on the night team.
If a program’s idea of “innovation” is just “switch to night float and call it wellness,” they’re behind. The direction of travel is toward systems that simultaneously protect residents’ sleep and provide real supervision and sane workloads. Night float can be part of that. It’s not synonymous with it.
So: Malignant Innovation or Burnout Protection?
Here’s the blunt answer:
Night float is neither hero nor villain. It’s a scalpel. In careful hands, it prevents harm. In the wrong hands, it cuts the people holding it.
When you’re evaluating a residency:
- Do not be impressed just because they say “we use a night float system.”
- Do not be scared off just because someone on Reddit had a miserable night float experience somewhere else.
- Look at how many nights, what protections exist, how supervision works, and whether residents sound like human beings or hostages when they talk about it.
If the structure respects physiology and reality, night float can absolutely reduce catastrophic fatigue and acute exhaustion. If it’s slapped on top of an already broken, understaffed service, it becomes malignant fast.
You’re not choosing “night float or no night float.” You’re choosing between programs that think deeply about how nights work – and programs that use residents as plug-and-play night coverage.

| Category | Value |
|---|---|
| Well-Run Programs | 70 |
| Average Programs | 40 |
| Red-Flag Programs | 10 |
(Interpretation: rough illustration of percent of residents who view night float as net-positive in different environments – the structure, not the concept, drives perception.)
FAQ
1. Is a residency without night float automatically better?
No. A program with traditional 24–28 hour calls can be far more dangerous and exhausting than a well-designed night float system. The question isn’t “night float vs no night float,” it’s “how are nights staffed, supervised, and limited?” A no-night-float program that still works you 28 hours every third night is not a win.
2. How many weeks of night float is too many?
As a rough rule of thumb, if you’re doing more than 4–5 months of nights across a 3-year residency, that’s heavy. You want blocks that are time-limited, with clear recovery periods, and not stacked back-to-back. A single brutal 4-week night block repeated multiple times per year is a warning sign unless the workload and backup are excellent.
3. Is it okay if attendings are only available by phone at night?
It depends on the service and the culture. Phone-only can work if volumes are sane, expectations for calling are supportive, and attendings actually pick up and come in for sick patients. If “only by phone” is combined with huge cross-cover lists and a culture of “don’t wake the attending,” that is a red flag. The supervision model matters more than the label.
Key points: Night float is a neutral tool, not inherently malignant or protective. Its impact on burnout and safety depends entirely on how it’s structured and supervised. And when you’re evaluating programs, ignore the marketing spin and interrogate the actual schedule, workload, and resident experience around nights.






















